The parotid glands are paired and are the largest and main glands for the production of saliva in humans. They are located between the mouth and the right and left ears, respectively.
Each parotid gland is located around a ramus of the mandible and secretes saliva through the parotid duct into the mouth to facilitate swallowing and initial digestion of food.
The appearance of the parotid glands begins in the sixth week of fetal development, when large salivary glands are formed. The epithelial rudiments of these glands are located on the inner surfaces of the cheeks, near the labial commissure. These buds grow posteriorly to the auditory placodes of the ears to form solid, cord-like objects, which become the parotid ducts by the tenth week of pregnancy. Secretion of the parotid glands begins in the eighteenth week of pregnancy.
Structure of the parotid gland
The parotid gland has four surfaces: lateral, superior, anteromedial and posterior, as well as three borders: anterior, medial and posterior. Also, the parotid gland has an upper and lower end.
The facial nerve, external carotid artery, parts of the greater auricular nerve, superficial temporal artery, maxillary artery, and retromandibular vein pass through the parotid gland.
The parotid glands are a pair of mostly serous salivary glands that are located inferiorly and anterior to the external auditory canal, secreting saliva into the oral cavity through the ducts of the parotid glands. Each gland is located posterior to the ramus of the mandible and anterior to the mastoid process of the temporal bone. Each gland is easily palpable and approximately wedge-shaped. The duct of the parotid gland exits from its anterior section into the masticatory muscle. This canal passes through the buccal muscle and enters the oral cavity from the inside of the cheek opposite the second molar of the upper jaw. The parotid papilla is a small rise of tissue and is the opening of the parotid canal on the inside of each cheek.
Each parotid gland has a capsule of its own dense connective tissue, but also has a false capsule from a layer of deep cervical fascia. The fascia on an imaginary line between the mastoid process and the angle of the mandible is divided into superficial plates and deep plates embedded in the gland. Some of this substance is found in the laughter muscle.
The parotid gland has short striated canals and long intercalated canals. The intercalated channels are multiple and built from cubic epithelial cells, while they have lumens larger than those of the acini. The striated canals of the parotid glands are also numerous and consist of simple columnar epithelium, having strata representing inclusions of basement membranes and mitochondrial cells.
Although the parotid glands are the largest of the salivary glands, they produce only about 25% of the total volume of salivary fluid. In the parotid glands, serous cells predominate, which makes their secretion mainly a serous secretory product. The parotid glands also secrete salivary alpha-amylases, which serve to break down starch during chewing. These are the main glands that secrete this product. These substances break down amylose and amylopectin by alpha hydrolysis of the 1,4 bond. Alpha-amylases are also thought to prevent the accumulation of bacteria in the mouth.
Each parotid gland is located deep in the skin, has inclusions of a layer of deep cervical fascia and the greater auricular nerve, namely its anterior branch C2 and C3.
The parotid gland is located posterolateral to the ramus of the mandible, masseter and medial pterygoid muscles. Part of the parotid gland may be located between the ramus and the medial pterygoid bone, as well as the pterygoid process. The branches of the facial nerve and the parotid duct emerge from this place.
The parotid gland is located anterolateral to the mastoid process of the temporal bone with its connections to the sternocleidomastoid and digastric muscles.
The parotid gland contacts the superior pharyngeal constrictor, which indicates the need to examine the pharynx for mumps.
Parotid gland (glandula parotis)
⇐ PreviousPage 3 of 3The parotid gland (glandula parotis) lies on the masticatory muscle and a significant part of it is located behind the lower jaw. Surrounded by fascia and muscles, it, together with the vessels and nerves passing through its thickness, forms the muscular-fascial space (spatium parotideum), which is also called the bed of the gland. This space is delimited by the leaves of the fascia parotideomasseterica and the muscles: m.masseter and m.pterygoideus (between them - the lower jaw), m. sternocleidomastoideus. In the depths of the face, this space is delimited by muscles starting from the styloid process of the temporal bone, and below by the posterior abdomen of the m.digastricus. At the top, the spatium parotideum is adjacent to the external auditory canal, the cartilage of which has notches that allow lymphatic vessels to pass through. Here is a “weak spot” in the fascial covering of the gland, subject to rupture during purulent parotitis, which often opens into the external auditory canal. Below, the spatium parotideum is delimited from the gl.submandibularis bed by a dense fascial layer connecting the angle of the lower jaw with the sheath of the sternocleidomastial muscle.
Spatium parotideum
not closed on the medial side, where the pharyngeal process of the parotid gland fills the gap between the styloid process and the internal pterygoid muscle, being deprived of fascial cover (the second “weak spot” is in the fascial sheath of the gland); here the process is directly adjacent to the anterior part of the peripharyngeal space (Fig. 4). This makes it possible for the purulent process to transfer from one space to another.
Rice. 4. Parotid gland and parapharyngeal space.
1 – longissimus capitis muscle, 2 – sternocleidomastoid muscle, 3 – posterior belly of the digastric muscle, 4 – stylohyoid muscle, 5 – submandibular vein, 6 – external carotid artery, 7 – styloglossus muscle, 8 – stylopharyngeal muscle, 9 – parotid gland, 10 – parotid fascia, 11 – medial pterygoid muscle, 12 – branch of the mandible, 13 – masticatory muscle, 14 – masticatory fascia, 15 – buccal-pharyngeal fascia, 16 – parotid duct, 17 – buccal muscle, 18 – vestibule mouth, 19 – upper dental arch, 20 – incisive papilla, 21 – transverse palatal folds, 22 – palatal suture, 23 – hard palate, 24 – palatoglossal arch, 25 – soft palate, 26 – palatopharyngeal arch, 27 – superior pharyngeal constrictor, 28 – uvula, 29 – anterior parapharyngeal space, 30 – retropharyngeal space, 31 – pharyngeal tonsil, 32 – posterior parapharyngeal space, 33 – prevertebral fascia, 34 – pharyngeal-vertebral fascia, 35 – stylopharyngeal fascia, 36 – internal carotid artery, 37 – internal jugular vein. (From: Sinelnikov R.D. Atlas of Human Anatomy. - M., 1972.- T. II.)
The external carotid artery, retromaxillary vein, facial and auriculotemporal nerves pass through the gland. A.carotis externa is divided in the thickness of the gland into terminal branches:
1) a.temporalis superficialis, giving off a.transversa faciei and going, accompanied by n.auriculotemporalis, to the temporal region;
2) a.maxillaris, passing into the deep area of the face.
N.facialis forms a plexus - plexus parotideus, located closer to the outer surface of the gland. In the thickness of the gland and directly under its capsule lie the lymph nodes (nodi parotidei).
A purulent process developing in the parotid gland (spatium parotideum) can cause paralysis of the facial nerve or severe bleeding from vessels destroyed by pus that pass through the thickness of the gland (external carotid artery, retromandibular vein).
The excretory duct of the parotid gland, ductus parotideus, is located on the anterior surface of the masticatory muscle at a distance of 2.0-2.5 cm downward from the zygomatic arch. On its way to the vestibule of the oral cavity, the ductus parotideus pierces the buccal muscle (and often the fatty body of the cheek) near the anterior edge of the m. masseter The place where the duct enters the vestibule of the mouth in approximately half of the cases lies at the level of the space between the first and second upper molars, in approximately 1/4 of the cases - at the level of the second molar.
Deep facial area (regio facialis profunda)
The deep region of the face (regio facialis profunda) contains various formations related primarily to the masticatory apparatus. Therefore, it is also called the maxillary-masticatory region. The basis of the region is made up of the upper and lower jaws and the masticatory muscles starting mainly from the sphenoid bone: m.pterygoideus lateralis, attached to the articular process of the lower jaw, and m.pterygoideus medialis, attached to the inner surface of the angle of the lower jaw.
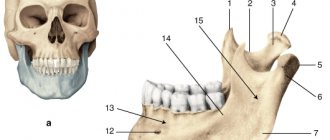
By removing the branch of the lower jaw, vessels, nerves and loose fatty tissue are revealed. N.I. Pirogov was the first to describe the cellular spaces in the deep region of the face, located between the branch of the lower jaw and the tubercle of the upper jaw. He called this part of the face the intermaxillary region and distinguished two spaces here. One of them, the temporopterygoid space (interstitium temporopterygoideum), is located between the terminal section of the temporal muscle, attached to the coronoid process of the mandible, and the lateral pterygoid muscle; the other, the interpterygoid space (interstitium interpterygoideum), is located between both pterygoid muscles - lateral and medial.
In both spaces, communicating with each other, there are vessels and nerves surrounded by fiber. The most superficial is the venous plexus - plexus pterygoideus. It lies mostly on the outer surface of the lateral pterygoid muscle, between it and the temporal muscle, i.e. in the temporopterygoid space. The other part of the plexus is located on the deep surface of the m.pteryoideus lateralis. Deeper than the venous plexus and mainly in the interpterygoid space, arterial and nerve branches are located.
A.maxillaris is often visible in both spaces. This is explained by the fact that three arches are formed along the artery, of which the last two, as shown by N.I. Pirogov, are located in the interpterygoid and temporopterygoid spaces. Numerous branches depart from the artery, of which we will note some. A.meningea media penetrates through the foramen spinosum into the cranial cavity; a.alveolaris inferior enters the canal of the lower jaw, accompanied by the nerve and vein of the same name; aa.alveolares superiores are directed to the teeth through the openings in the upper jaw; a.palatina descendens goes to the pterygopalatine canal and further to the hard and soft palate.
N. mandibularis emerges from the foramen ovale, covered by the lateral pterygoid muscle, and soon splits into a series of branches. Of these, n.alveolaris inferior passes in the space between the adjacent edges of both pterygoid muscles and the inner surface of the branch of the lower jaw, then descends to the opening of the mandibular canal; behind it pass the artery and vein of the same name. N.lingualis, to which the chorda tympani is attached at some distance from the oval foramen, lies similarly to n.alveolaris inferior, but anterior to it and, passing under the mucous membrane of the floor of the mouth, gives branches to it and to the mucous membrane of the tongue.
The location of n.alveolaris inferior on the inner surface of the lower jaw branch is used to produce so-called mandibular anesthesia. A puncture of the mucous membrane and the introduction of a novocaine solution are performed slightly above the level of the lower molars. When removing upper molars, anesthesia is carried out by intraoral injection of novocaine solution into the area of the tubercle of the upper jaw.
The transfer of infection from the tooth to the jaw can lead to the development of an infiltrate, compressing the vessels and nerves passing into the bones. Compression by the infiltrate of n.alveolaris inferior leads to disruption of nerve conduction, resulting in anesthesia of half the lip and chin. If thrombophlebitis v.alveolaris inferior develops, it causes swelling of the face within the corresponding half of the lower jaw and lower lip.
Branches to the masticatory muscles also arise from the mandibular nerve, in particular nn.temporales profundi; buccal nerve n.buccalis, which pierces the buccal muscle and supplies the skin and mucous membrane of the cheek; n.auriculotemporalis, which is directed through the thickness of the parotid gland to the temporal region. On the deep surface of the mandibular nerve, immediately below the foramen ovale, there is an ear ganglion, ganglion oticum, in which the parasympathetic fibers of the glossopharyngeal nerve for the parotid gland are interrupted. Postganglionic secretory fibers for this gland are part of the auriculotemporal nerve and reach the gland tissue through the branches of the n.facialis.
In the deepest part of the region, in the pterygopalatine fossa, the ganglion pterygopalatinum is located. The second branch of the trigeminal nerve also enters here, from which the pterygopalatine nerves (nn.pterygopalatini) approach the ganglion. In addition to the latter, the nerve of the pterygoid canal approaches the ganglion. nn arise from the ganglion. palatini, going through the canalis pterygopalatinus to the hard and soft palate (together with a.palatina descendens), and nn.nasales posteriores, going into the nasal cavity (through the foramen sphenopalatinum).
The fiber of the temporopterygoid and interpterygoid spaces passes into neighboring areas either directly or along the course of blood vessels and nerves. Spreading upward, it covers the temporal muscle, and then at the anterior edge of the latter it passes behind the zygomatic arch into the buccal region, where this fiber is known as the fatty body of the cheek (Bishat), located between the mm.masseter and the buccinator. Surrounding these vessels and nerves, the fiber of the temporopterygoid and interpterygoid spaces reaches the openings at the base of the skull; in the posterior and inward direction it reaches the pterygopalatine fossa and the orbit. Along the course of the lingual nerve, the fiber of the interpterygoid space reaches the floor of the oral cavity. The cellular spaces of the intermaxillary region can be involved in a purulent inflammatory process with so-called osteophlegmons, i.e. suppuration of tissue with a primary focus in the bone.
The most common cause of osteophlegmon, in particular perimandibular, is damage to the lower molars. In this case, the medial pterygoid muscle is involved in the process, resulting in trismus, i.e. inflammatory contracture of the named muscle, making it difficult to open the mouth. Further spread of the infection can lead to phlebitis of the veins of the pterygoid plexus with the subsequent transition of the inflammatory process to the veins of the orbit. Suppuration of the tissue of the temporopterygoid space can spread to the dura mater along the course of a. meningea media or branches of the trigeminal nerve (through the spinous, oval or round foramen).
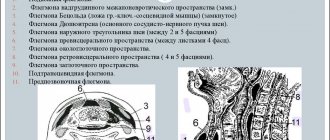
In the development of deep phlegmon, the fiber of two spaces located in the circumference of the pharynx, the retropharyngeal and peripharyngeal, also plays a significant role. The peripharyngeal space (spatium parapharyngeale) surrounds the pharynx from the sides. It is separated from the retropharyngeal space, located behind the pharynx, by a lateral septum, which is formed by a fascial sheet stretched between the prevertebral fascia and the fascia of the pharynx (aponeurosis pharyngoprevertebralis).
The peripharyngeal space is enclosed between the pharynx (from the inside) and the bed of the parotid gland and the medial pterygoid muscle (from the outside). At the top it reaches the base of the skull, and at the bottom - the hyoid bone, and m.hyoglossus is separated from the submandibular salivary gland and its capsule. In the peripharyngeal space, two sections are distinguished: anterior and posterior. The border between them is formed by the styloid process with the muscles starting from it (mm.stylopharyngeus, styloglossus and stylohyoideus) and the fascial layer stretched between the styloid process and the pharynx (aponeurosis stylopharyngea).
The anterior part of the parapharyngeal space is adjacent to: from the inside - the palatine tonsil, from the outside (in the interval between the medial pterygoid muscle and the styloid process) - the pharyngeal process of the parotid gland. Vessels and nerves pass through the posterior part of the parapharyngeal space: v.jugularis interna is located outside, a.carotis interna and nn.glossopharyngeus, vagus, accessorius, hypoglossus and sympathicus are located inward from it. The uppermost group of deep cervical lymph nodes is also located here.
In the anterior part of the parapharyngeal space there are branches of the ascending palatine artery and veins of the same name, which play a role in the spread of the inflammatory process from the tonsil area (for example, with peritonsillar abscess).
The retropharyngeal space (spatium retropharyngeale) is located between the pharynx (with its fascia) and the prevertebral fascia and stretches from the base of the skull to the level of the VI cervical vertebra, where it passes into the spatium retroviscerale of the neck. Usually the retropharyngeal space is divided by a septum located in the midline ,
into two sections - right and left (A.V. Chugai). This explains the fact that retropharyngeal abscesses, as a rule, are unilateral.
Infection of the peripharyngeal space is often observed with lesions of the seventh and eighth teeth of the lower jaw and the tissue of the interpterygoid space. The transition of the purulent process from this gap to spatium parapharyngeale is possible either due to secondary infection of spatium parotideum, or through the lymphatic tract. Inflammation of the tissue in the peripharyngeal space leads to symptoms such as difficulty swallowing, and in severe cases, difficulty breathing. If an infection from the anterior part of the spatium parapharyngeale penetrates into the posterior part (destruction of aponeurosis stylopharyngea), then its further spread can occur along the spatium vasonervorum of the neck into the anterior mediastinum, and if the infection passes to the spatium retropharyngeale, along the esophagus into the posterior mediastinum.
With purulent damage to the tissue of the posterior part of the peripharyngeal space, there is a danger of necrosis of the wall of the internal carotid artery (with subsequent severe bleeding) or the development of septic thrombosis of the internal jugular vein.
Incisions on the face during purulent processes.
To make incisions on the face, it is necessary to strictly follow anatomical landmarks in order to avoid possible damage to the branches of the facial nerve, leading to functional disorders and deformation of the face (Fig. 5). Based on the topographic-anatomical distribution of the main branches of the facial nerve, it is necessary to select the most “neutral” spaces between them for incisions. This requirement is met by radial incisions running from the external auditory canal in a fan-shaped manner towards the temporal region, along the zygomatic arch, to the wing of the nose, to the corner of the mouth, to the corner of the lower jaw and along its edge.
V.F. To open phlegmon in the retromandibular area (parotitis, parapharyngeal phlegmon), Voino-Yasenetsky recommends making an incision in the skin and fascia near the angle of the lower jaw, and penetrating deeper with a blunt method (preferably with a finger). With this incision, the n. colli is intersected, which does not cause significant disorders; sometimes the n.marginalis mandibu1ae (innervates the muscles of the chin) can be damaged. Cheek phlegmon in the m.masseter area, which is most often the spread of mumps, is opened with a transverse incision running from the lower edge of the earlobe (2 cm in front) towards the corner of the mouth. The incision passes between the branches of the facial nerve; they are damaged during such incisions only in rare cases. It is recommended to open perimaxillary phlegmons involving the buccal fatty lump (corpus adiposum buccae) with an incision starting 2-3 cm outward from the wing of the nose and continuing towards the earlobe for 4-5 cm. The incision should not be made deep, because here you can damage the v.facialis and stenon ducts. The branches of the facial nerve are rarely damaged with this incision. For perimaxillary phlegmon, it is better to make an incision through the mucous membrane of the vestibule of the mouth on the buccal-maxillary fold.
In the temporal region, the main typical incision should be behind the frontal process of the zygomatic bone between the fan-shaped temporal branches of the facial nerve.
Rice. 5. The most typical cuts on the face.
(From: Elizarovsky S.I., Kalashnikov R.N. Operative surgery and topographic anatomy. - M., 1967.)
Theoretical questions for the lesson:
1. Borders, division into areas of the lateral area of the face.
2. External landmarks and projections (neurovascular formations, parotid gland and its duct).
3. Buccal area of the face, layered topography, contents: fatty body of the cheek, its processes.
4. Parotid-masticatory region: layer-by-layer structure; parotid gland: bed, excretory duct, vessels and nerves.
5. Deep area of the face: fascia, cellular spaces, muscles, blood vessels and nerves.
6. Paths of spread of purulent-inflammatory processes and anatomical rationale for incisions in the lateral area of the face.
7. Malformations of the facial part of the head.
8. Features of primary surgical treatment of facial wounds.
Practical part of the lesson:
1. Be able to determine the projection of the main vessels and nerves of the face, the excretory duct of the parotid salivary gland.
2. Master the technique of layer-by-layer preparation of the lateral area of the face.
Questions for self-control of knowledge
1. What are the boundaries and external landmarks of the lateral area of the face?
2. What is the boundary between the parotid-masticatory and buccal regions?
3. Name the branches of the facial nerve?
4. Name the formations that are located under the capsule of the parotid salivary gland.
5. What is the structural feature of the bed of the parotid salivary gland?
6. What areas are the weak points of the gland?
7. What cellular spaces are allocated in the deep area of the face?
8. List the neurovascular formations of the deep region of the face.
9. What incisions are used for purulent-inflammatory processes on the face?
10. What is trismus?
11. What complications arise when the facial nerve is damaged?
Self-control tasks
Problem 1
To drain the suppurative process from Bichat's lump, the surgeon made an incision along the anterior edge of the masticatory muscle. Is the incision made correctly and what formations will the surgeon encounter?
Problem 2
Can pus from the parotid salivary gland during purulent parotitis spread into the parapharyngeal cellular space? If yes, then in what way?
Problem 3
To drain the suppurative process of the parotid salivary gland, the surgeon made 5 incisions running from the base of the earlobe radially towards the temporal bone, to the corner of the eye, to the wing of the nose, to the corner of the mouth, to the corner of the lower jaw and along its edge. Did the surgeon make the incisions correctly?
Problem 4
A patient with purulent parotitis began to experience profuse erosive arterial and venous bleeding. From which vessels is bleeding possible in this case?
Problem 5
A patient with purulent parotitis developed symptoms of drooping of the corner of the mouth, smoothing of the nasolabial and nasobuccal folds. What is the reason for their appearance?
Standards of correct answers
Problem 1
When making incisions in the buccal area, firstly, the cosmetic effect is taken into account. Secondly, when making an incision along the anterior edge of the masticatory muscle, there is a danger of damaging the branches of the facial nerve, which will lead to paralysis of the facial muscles, or the excretory duct of the salivary gland. Therefore, it is most advisable to open the suppurative processes of Bisha’s lump from the vestibule of the oral cavity.
Problem 2
The space of the parotid salivary gland is not closed on the medial side, where the pharyngeal process of the parotid gland fills the gap between the styloid process and the internal pterygoid muscle, being deprived of fascial cover. Here the process is directly adjacent to the posterior part of the peripharyngeal space, which makes it possible for the purulent process to transfer from one space to another.
Problem 3
Wrong. When making incisions on the face, the cosmetic effect must be taken into account. To drain purulent foci, a retromaxillary incision is most often used.
Problem 4
Since the external carotid artery and the retromandibular vein pass through the thickness of the parotid saliva gland, with purulent mumps the walls of these vessels are eroded.
Problem 5
The facial nerve passes through the thickness of the parotid saliva gland; as a result of the inflammatory process in the gland, it can be compressed, which leads to paresis of facial muscles.
Test tasks for self-control
⇐ Previous3
Innervation of the parotid glands
The innervation of the parotid glands is completely autonomous. The gland is innervated by postganglionic sympathetic fibers from the superior cervical sympathetic ganglion. The periarterial nerve plexus passing around the external carotid artery reaches the parotid gland. Their main function is to narrow blood vessels.
The cellular inclusions of the pregaglionic sympathetic nerves are usually located in the lateral branches of the upper thoracic spinal segments.
Preganglionic parasympathetic fibers emerge from the brainstem from the inferior salivary nucleus in the glossopharyngeal nerve. Salivation of the parotid glands is caused mainly by the glossopharyngeal nerve.
Enzymes of human saliva
The digestive system breaks down the nutrients we eat, turning them into molecules. Cells, tissues and organs use them as fuel to carry out various metabolic functions.
The digestion process begins the moment food enters the mouth. The oral cavity and esophagus do not produce any enzymes themselves, but the saliva produced in the salivary glands contains a number of important enzymes. Saliva mixes with food during the act of chewing, acts as a lubricant and begins the digestion process. Enzymes in saliva begin to break down nutrients and protect you from bacteria.
Salivary amylase
Saliva amylase molecule
Salivary amylase is a digestive enzyme that acts on starch, breaking it down into smaller carbohydrate molecules. Starches are long chains that are attached to each other. Amylase breaks the bonds along the chain and releases the maltose molecules. To experience the effects of amylase, just start gnawing on a cracker and within a minute you will feel that it has a sweet taste. Salivary amylase performs its functions better in a slightly alkaline environment or at a neutral pH; it cannot act in the acidic environment of the stomach, only in the oral cavity and esophagus! The enzyme is produced in two places: the salivary glands and the pancreas. The type of enzyme produced in the pancreas is called pancreatic amylase, which completes the digestion of carbohydrates in the small intestine.
Saliva lysozyme
Saliva lysozyme molecule
Lysozyme is secreted into tears, nasal mucus and saliva. The functions of salivary lysozyme are primarily antibacterial! This is not an enzyme that will help digest food, it will protect you from any harmful bacteria that enter the oral cavity with food. Lysozyme destroys polysaccharides in the cell walls of many bacteria. Once the cell wall has been broken, the bacterium dies, bursting like a water balloon. From a scientific point of view, cell death is called lysis, so the enzyme that performs the task of destroying bacteria is called lysozyme.
Lingual lipase
Lingual lipase molecule
Lingual lipase is an enzyme that breaks down fats, particularly triglycerides, into smaller molecules called fatty acids and glycerol. Lingual lipase is found in saliva, but it doesn't finish its job until it reaches the stomach. A small amount of lipase, called gastric lipase, is produced by stomach cells. This enzyme specifically digests milk fat in food. Lingual lipase is a very important enzyme for babies because it helps them digest the fats in milk, which makes digestion much easier for their immature digestive system.
Proteases
Proteases
Any enzyme that breaks down proteins into their constituent parts, amino acids, is called a protease, which is a general term. The body synthesizes three main proteases: trypsin, chymotrypsin and pepsin. Special cells in the stomach produce the inactive enzyme pepsinogen, which is converted to pepsin when it comes into contact with the acidic environment in the stomach. Pepsin breaks certain chemical bonds in proteins called peptides. The human pancreas produces trypsin and chymotrypsin, enzymes that enter the small intestine through the pancreatic duct. When partially digested food moves from the stomach to the intestines, trypsin and chymotrypsin produce simple amino acids that are absorbed into the blood.
Other salivary enzymes in the human body Although amylase, protease and lipase are the three main enzymes that the body uses to digest food, many other specialized enzymes also help in this process. The cells that line the intestines produce enzymes: maltase, sucrase and lactase, each capable of converting a specific type of sugar into glucose. Likewise, special cells in the stomach secrete two other enzymes: renin and gelatinase. Renin acts on the protein in milk, converting it into smaller molecules called peptides, which are then completely digested by pepsin.
Disease of the parotid glands
Mumps
Among the diseases of the parotid glands, the most common is mumps - inflammation of one or both parotid glands. In addition to a viral infection, certain types of bacteria can cause mumps when bacterial mumps develops. This infection causes blockage of the parotid gland ducts. Inflammation and swelling of the parotid glands can also be caused by benign lymphoepithelial lesions, which are caused by Mikulicz's disease and Sjögren's syndrome.
Granuloma
Tuberculosis and syphilis can provoke the formation of granulomas in the parotid gland.
Parotid stones
Typically, stones in the parotid glands form at the junction of the main duct and the small ducts of the gland. Symptoms in this case manifest themselves in the form of severe pain during salivation. Or the parotid glands become enlarged before eating, when intense salivation occurs. Treatment for stones in the parotid glands involves surgical removal of them, and in some cases, removal of the gland itself.
Tumors
Approximately 80% of tumors arising in the parotid glands are benign. Moreover, 70% of them are pleomorphic adenomas, occurring mainly in women; other types of tumors are adenolymphomas, which more often affect men. The growth of the tumor can cause pain because the tumor itself affects the nerve passing through the parotid gland.
The remaining 20% of tumors are malignant, the most common being mucoid squamous cell carcinoma or mucoepidermoid carcinoma, as well as lymphoid cystic carcinoma.
Surgical treatment of tumors of the parotid glands presents certain difficulties due to the passage through the tissue of the facial nerve. That is why detection of the tumor in the early stages is very important in treatment.
Where are the salivary glands located?
There are small and large groups of salivary glands. The minor glands are labial, buccal, molar, lingual and palatine. All of them are located in separate clusters in the thickness of the oral mucosa. The glands of this group secrete saliva with a high content of lipase, which is responsible for the breakdown of fats.
The major salivary glands include three paired groups: sublingual, parotid and submandibular.
- The parotid glands are the largest (weighing up to 20 g) and are located under the skin in front and downward from the ears, in contact with the lower jaw. The excretory duct of the gland pierces the buccal muscle and opens on the inner surface of the cheek at the level of the second upper molar. They synthesize saliva with a high content of amylase (participates in the breakdown of carbohydrates), chlorine, potassium and sodium ions.
- The sublingual glands are considered the smallest of this group, their weight reaches 5 g. They are located on the floor of the oral cavity to the right and left of the frenulum of the tongue. Excretory ducts can open as separate openings or together with the ducts of the submandibular glands. They synthesize saliva with a high content of mucin.
- The submandibular glands are intermediate in size between the previous groups. They are located in the submandibular triangle, which is bounded above by the lower jaw, on the inside by the styloglossus muscle, on the outside by the facial arteries and veins, and in front by the edge of the mylohyoid muscle. The composition of saliva is mixed (protein-mucous), contains enzymes and mucin.
All of these groups of salivary glands are involved in digestion processes in the oral cavity.
In continuation of the topic, be sure to read:
- When, how and how much to brush your teeth to stay healthy?
- Bad breath: causes and methods of eliminating it
- What medications should I use for increased gas formation?
- Details about the coprogram: preparation, conduct and interpretation of the analysis
- List of enzymes to improve digestion and their intake
- Peritonitis: what kind of disease is it, how does it manifest and be treated?
- Causes of bloating and increased gas formation, treatment methods
- Gastroesophageal reflux disease (GERD): symptoms, treatment methods and complications
- Consistency of stool in an adult: where is the norm and where is the pathology?
- Stool color in newborns: where is the norm and where is the pathology?
Age-related features of the functioning of the salivary glands
Read:- I. Organ-specific tumors of the thymus.
- I. Physiology of the fetal thyroid gland
- II. Examination of patients with thyroid nodules
- II. Organ-nonspecific tumors of the thymus.
- II. Thyroid hormone medications
- III) Major salivary glands
- III) Male gonads
- III) Pancreas
- III. Locally advanced breast cancer stage III
- III. Thymus tumors
The secretion of the salivary glands is subject to natural age-related changes. The salivary glands function from the moment of birth, but at first the secretion of saliva is insignificant, which causes some dryness of the oral mucosa in children in the first months of life. However, from the 5-6th month of life, salivation increases significantly. Sometimes children do not have time to swallow saliva and it involuntarily flows out of the mouth (physiological drooling).
The projection of the duct of the parotid salivary gland in newborns and young children is different than in adults. The duct is located low, has an indirect course and opens at a distance of 0.8-1 cm from the anterior edge of the masticatory muscle. The parotid salivary gland is more rounded, extends slightly forward and reaches the angle of the lower jaw. The facial nerve lies superficially. During puberty, secretory processes in the salivary glands occur especially intensively, which is due to hormonal changes in the body.
Age-related involution of the glands of the oral mucosa begins after 60-70 years. In old age, some of the protein glands of the mucous membrane stop secreting protein secretions and begin to secrete secretions rich in acidic and neutral glycosaminoglycans. Some gland cells atrophy, the layer of connective tissue increases, and fat cells appear in large numbers. Atrophic changes are observed in the epithelial cells lining the ducts of these glands, which is accompanied by a violation of the secretory function of the glands and the development of dry mucous membrane.
A functional system that ensures the formation of a bolus of food adequate for swallowing
The functional system that ensures the formation of a bolus of food adequate for swallowing begins with the eruption of the first teeth (at 6-8 months) and ends with the end of the eruption of molar milk teeth (at 2.5-3 years). By the time the first teeth erupt, the child is not able to chew. However, from the moment the antagonist teeth of the incisor group erupt at 10-12 months, he gradually learns to bite off small pieces of food. The food bolus is not yet formed during this period. Those parts of food that enter the mouth are sucked, moistened with saliva and, if they reach the root of the tongue, swallowed. More often, these pieces, together with saliva, are pushed out by the tongue. This happens because the lips are not yet able to tightly close the entrance to the oral cavity, and the tongue makes mainly piston-like movements back and forth, providing sucking. When the tongue moves forward, the contents are pushed out of the oral cavity. This is clearly observed when feeding an infant porridge, part of which is swallowed, and the other part is pushed out. Over the course of several months, the child gradually learns to form a food bolus from mushy foods. In artificially fed children, this process goes much faster. A full-fledged food bolus is usually formed by 2.5-3 years, when all the primary teeth erupt. At this time, the child can already eat various foods on his own.
Studies in children conducted by masticationography have shown that after the eruption of the first milk teeth, chewing movements are still weakly expressed, arrhythmic, alternating with sucking. With an increase in the number of primary teeth, the chewing movements of the lower jaw become more differentiated, the amplitude of the chewing waves increases, and they become more rhythmic. By the age of three, the masticogram becomes stable.
An increase in the time of formation of the food bolus and a decrease in chewing power is observed in children aged 9-10 years, which is associated with the change of IV and V milk teeth to permanent ones. As the permanent occlusion becomes established and the formation of the dental system completes, chewing efficiency increases and reaches its maximum by the age of 12. Thus, children aged 10 years spend 18 seconds chewing a hazelnut kernel weighing 800 mg, making 29-30 chewing movements. At the age of 12 years, chewing the same nut takes 15 seconds with 20-23 chewing movements.
After a complete change of primary teeth with intact dentition, the masticationogram is a sequential alternation of all elements of chewing waves, reflecting normal chewing movements of the lower jaw. From this time (12-13 years), the functional chewing system until old age ensures the formation of a food bolus adequate for swallowing.
In old age, there is an increase in the time of formation of the food bolus, which is associated with the involutive processes that occur in the dentofacial apparatus with aging. With age and tooth loss, the functional masticatory system first uses its compensatory capabilities. At the beginning, compensation is achieved by lengthening the time of formation of the food bolus. In the future, in the absence of a large number of teeth or their complete loss, it becomes possible to eat only crushed, mushy or liquid food.
On masticograms of elderly people, the amplitude of masticatory waves decreases. They become less rhythmic and additional waves disappear. This is associated with a weakening of the tone of the masticatory muscles and various disorders in the dentofacial apparatus.
Functional speech production system
The functional system of speech production begins to form at 8-10 months and ends at 2.5-3 years. The development of speech function occurs in accordance with a certain system of language, which is built on the basis of intonation structures and its phonemic composition. The process of speech development itself is divided into 1) a preparatory period, including screaming, humming and babbling; 2) the period of understanding the speech of adults, and the use of words-sentences in active speech, and 3) the period of mastering phrasal speech.
The first functional connections in the corresponding morphological structures, united into a functional speech production system, arise when a newborn cries. The acoustic characteristics of a newborn's cry contain the same components as speech sounds and occur at the same frequencies. In this case, the cry, perceived by the auditory analyzer, stimulates the functional activity of the speech areas of the cerebral cortex.
In the first months of a child's life, vocal reactions of humming
(sounds such as AU, EU), gradually acquiring different intonation colors, which indicates the beginning of assimilation of the intonational pattern of the language.
From 5-6 months of life, the child begins to develop vocal reactions such as babbling
. He begins to pronounce the sounds BA, MA, PA. From the 8th-9th month, babbling becomes longer, its intonation coloring is enriched, sounds begin to repeat, gradually acquiring the meaning of words (BABA, MOTHER, DAD). At this time, the child’s organs of articulation continue to develop, and the auditory analyzer gradually becomes capable of subtle auditory perceptions necessary for distinguishing phonemes. There is a gradual improvement in the relationship between the speech-motor analyzer and the auditory one, which leads to the formation of a speech-auditory analyzer.
From 9-10 months, the child develops understanding of speech, words acquire a certain meaning. Gradually, the word itself acquires a dominant meaning as a certain combination of speech sounds. To master the semantic composition of speech, it is necessary to form connections between words and related objects. These connections are formed by adults by associating specific objects and actions with the words denoting them, as well as by stimulating the child’s active speech activity and his speech imitation.
By the end of the first year of life, the child pronounces phonemes according to the language system, which he hears both in the speech of adults and in his own sounds of humming (vowels like A, E, U) and babbling (consonants like M, P, T). The remaining phonemes (all hissing sounds, L, R sounds) are pronounced by the child later - in the second and third years of life.
The child's active speech begins with the first words, the pronunciation of which is initially very imperfect; the combination of speech sounds only vaguely resembles the words that they are supposed to denote. Usually this child’s speech is well understood by those who work with him and raise him. At this age, the words spoken by the child can reflect the meaning of an entire sentence. For example, the word MOTHER is used when the mother leaves or comes. During this period, onomatopoeic words like AB-AB (dog), TIK-TAK (clock), etc. appear.
Understanding of speech develops most rapidly in the second year of life. The child begins to understand speech addressed to him and carries out simple instructions. This means that the function of the speech-auditory analyzer for recognizing acoustic structures according to the native language system has been formed. In the second half of the second year of life, a qualitative leap occurs in the development of active speech. At this time, an attempt appears to connect words into phrases using plural forms. By the age of two, a child’s vocabulary reaches approximately 300 words.
In the third year of life, the child masters the correct pronunciation of phonemes, numerous phrases and subordinate clauses appear, and pronouns and conjunctions are actively used. During this period, the main formation of the functional speech production system ends. The formation of the primary occlusion is of great importance in this process. If there are deviations in it (open, pronounced progeny or prognathism), then the formation of phonemes may slow down or be disrupted. If there is an anomaly in the development of the tongue or facial muscles, then a disturbance in speech formation may manifest itself in the form of burr, lisp, and tongue-tiedness. Consequently, the ability to form phonemes, and therefore word formation, depends largely on the state of the organs of the cavity, on the degree of their participation in phonation.
Difficulties in the formation of phonemes are observed in children aged 7-8 years when changing the incisive group of teeth, and at the age of 12-14 years due to the end of the formation of a permanent bite in the dentoalveolar apparatus.
The formation of the speech production function entirely depends on the state of the auditory analyzer, as well as on the environment in which the child develops, and on the degree of communication with other people. Children who are deaf from birth, due to the lack of auditory stimuli, are not able to learn to speak. Partial deafness and hearing loss also affects the ability to form speech. Hearing loss even in adulthood leads to changes in speech production function.
The environment is of great importance in the formation of speech. If a child has not learned to speak before the age of 10-12, then in subsequent years he will not learn to speak. There are known examples of “Mowgli” children raised among wild animals in the jungle. Usually such children cannot be taught to speak.
Regular changes in speech production are observed in boys during puberty. Due to the restructuring that occurs during this period in the larynx, vocal cords, and facial skeleton, the volume of the vocal tract changes and, as a consequence, phonation and voice formation. At the same time, the voice acquires new, individual shades of timbre, and due to the restructuring of the psyche, a change in the rate of speech production may occur.
The state of neuroendocrine homeostasis is of no small importance in speech production. When the level of sex hormones changes, the volume and timbre of the voice may change, and a masculine timbre may appear in women and a feminine timbre in men.
In old age, speech formation undergoes certain changes associated with involutive processes in the dental system, in particular in the word-forming organs. The timbre of the voice changes, trembling and vibration appear in it, and the formation of many phonemes is disrupted.
CONTROL QUESTIONS
Date added: 2015-02-02 | Views: 2719 | Copyright infringement
| | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | | 48 | | | | |
Operations
When removing the submandibular gland, a 7-8 cm long incision is made parallel to the lower edge of the body of the lower jaw, 2 cm away from it. The skin, subcutaneous tissue, subcutaneous muscle of the neck, and the superficial plate of the fascia of the neck are dissected, the gland capsule is opened, and the facial vein is ligated. . P.J. easily separates from the tissues of the bed. When separating the inner surface of the pancreas. The facial artery is isolated and ligated. In the region of the upper pole of the pancreas. the excretory duct is isolated and ligated and the facial artery is re-ligated. If the gland is removed due to an inflammatory process, then one should not go beyond its capsule so as not to damage the facial nerve (marginal branch of the lower jaw). The wound is sutured in layers, leaving the wound closed for 24 hours.
Bibliography:
Zedgenidze G. A. X-ray diagnosis of diseases of the salivary glands, L., 1953, bibliogr.; Kasatkin S.N. Anatomy of the salivary glands, Stalingrad, 1948; Sazama L. Diseases of the salivary glands, trans. from Czech., Prague, 1971, bibliogr.; Solntsev A. M. and Kolesov V. S. Surgery of the salivary glands, Kyiv, 1979, bibliogr.; Burch RJ a. Woodward HW Differential diagnosis and surgery of the submaxillary gland, J. oral Surg., v. 18, p. 470, 1960; Rauch S. Die Speicheldriisen des Menschen, Stuttgart, 1959; Schulz HG Das Rontgenbild der Kopfspeicheldriisen, Lpz., 1969, Bibliogr.
I. F. Romacheva; V. S. Speransky (an., hist.).
Treatment of salivary gland cyst
Despite its painless occurrence, as well as mild pain, a salivary gland cyst must be treated. Currently, the only effective method for eliminating it is surgery.
Depending on the location of the cyst, the operation is performed both from the inside of the oral cavity and from the outside. Neutralization of the submandibular gland cyst is carried out together with the cyst itself. The submandibular parotid salivary gland is treated in a similar way; it is shown in the photo.
Diagnosis of salivary gland cyst
Diagnosis of the submandibular salivary gland is carried out to identify signs of pathology, including signs of cystic formations. The first stage of the study will include a visual examination of the patient using instrumental and laboratory devices.
Often, upon examination, a specialist is unable to distinguish a cyst from a tumor, so the study is continued using computed magnetic resonance imaging (MRI), cystography, ultrasound and sialography.
In advanced forms of the disease, additional examinations are often prescribed, such as cyst puncture and fine-needle aspiration biopsy. The collected biological material is sent for laboratory cytological and biochemical studies, the main purpose of which is to exclude malignant tumors.
Anatomy and histology
Sublingual region, sublingual gland, submandibular region, submandibular gland.
Rice. 1. Topography of the submandibular and sublingual areas (the right half of the lower jaw is removed, the skin and muscles are retracted). Rice. 2. Topography of the sublingual area (the tongue is raised, part of its mucous membrane is removed). Rice. 3. Topography of the submandibular region (the subcutaneous muscle of the neck and the superficial plate of the cervical fascia have been removed): 1 - tongue, 2 - anterior lingual salivary gland, 3 - deep artery of the tongue, 4 - submandibular duct, 5 - sublingual gland, 6 - lower jaw (partially removed ), 7 - mylohyoid muscle, 8 - geniohyoid muscle, 9 - submandibular gland, 10 - facial artery, 11 - facial vein, 12 - sublingual - lingual muscle, 13 - submandibular lymph node, 14 - upper root of the cervical loop , 15 - sternocleidoid - mastoid muscle, 16 - submandibular vein, 17 - internal jugular vein, 18 - internal carotid artery, 19 - external carotid artery, 20 - deep cervical lymph nodes, 21 - hypoglossal nerve, 22 - posterior belly of the digastric muscles, 23 - stylohyoid muscle, 24 - parotid gland, 25 - masticatory muscle, 26 - deep vein of the tongue, 27 - branch of the mandible (partially removed), 28 - lingual nerve, 29 - sublingual papillae, 30 - sublingual fold, 31 - frenulum of the tongue, 32 - anterior belly of the digastric muscle, 33 - subcutaneous muscle of the neck, 34 - superficial plate of the cervical fascia, 35 - base of the mandible, 36 - marginal branch of the mandible of the facial nerve. The submandibular gland is a paired organ, has a flattened-round, ovoid or ellipsoidal shape, its length in an adult is 3.5-4.5 cm, width 1.5-2.5 cm, thickness 1.2-2 cm. Weight ) gland in a newborn averages 0.84 g, in an adult 10-15 g. In old age, the gland undergoes sclerosis and its weight decreases. The submandibular gland is located in a niche limited laterally by the body of the lower jaw (corpus mandibulae), medially by the mylohyoid (m. mylohyoideus) and sublingual (m. hyoglossus) muscles; from below it is covered by skin, subcutaneous tissue, subcutaneous muscle of the neck (platysma) and the superficial plate of the cervical fascia (lamina superficialis fasciae cervicalis). In front, the gland borders with the anterior belly of the digastric muscle (venter ant. m. digastrici), behind - with the posterior belly of the digastric muscle (venter post. m. digastrici) and the stylohyoid muscle (m. stylohyoideus), below it approaches the greater horn of the hyoid bone (cornu majus osis hyoidei). The process of the Submandibular Gland penetrates the gap between the mylohyoid and sublingual muscles and can reach the sublingual gland (gl. sublingualis). The projection of the Submandibular Gland onto the surface of the face and neck has the shape of a diamond. The superficial plate of the cervical fascia, splitting, covers the gland, forming its capsule (saccus gl. submandibularis). The submandibular gland, unlike the parotid gland, is loosely connected to the capsule and is easily separated from it. The capsule of the Submandibular Gland includes the facial artery (a. facialis) and in some cases the facial vein (v. facialis). The artery goes around the gland from above or behind and lies in a groove on its medial surface, sometimes going deeper into the tissue of the gland. The facial vein runs along the lateral surface of the gland (tsvetn. Fig. 1). Near the submandibular gland there are also the submental artery and vein (a. et. v. submentales). On the surface of the Submandibular gland there are submandibular lymph nodes (Submandibular lymph nodes, T.; nodi lymphatici submandibulares). The submandibular duct (submandibular duct, T.; ductus submandibularis) was first described in 1656 by T. Barton. The duct emerges from the front part of the pancreas. and, going around the posterior edge of the mylohyoid muscle, goes above it, first between the geniohyoid and hyoglossus muscles, then along the medial surface of the sublingual gland, under the mucous membrane of the floor of the mouth in the sublingual region and opens on the sublingual papilla (caruncula sublingualis) nearby or together with the large sublingual duct. The length of the submandibular duct is 40-60 mm, internal diameter. 2-3 mm, at the mouth the duct narrows to 1 mm. The submandibular duct is usually straight, rarely arcuate or S-shaped. In almost half of the cases, additional lobules of the pancreas are located above and below it. On the sialogram in the lateral projection, the submandibular duct and its branches are projected onto the body and angle of the mandible.
The blood supply to the Submandibular Gland is carried out by the glandular branches of the facial artery: its upper anterior part is the submental artery (a. submentalis), and its lower anterior part is the lingual artery (a. lingualis). Venous outflow is carried out into the veins of the same name. Lymph flows into the submandibular and lateral deep cervical lymph nodes.
The submandibular gland is innervated in the same way as the sublingual gland (see).
The submandibular gland is a complex tubuloalveolar gland with mixed serous-mucosal secretion. It consists of lobules separated by layers of connective tissue, in which vessels and nerves pass. The lobules have serous and mixed (serous-mucosal) terminal sections. The serous end sections have the same structure as in the parotid gland (see). They have short intercalary and long, highly branching striated ducts. The mixed terminal sections consist of two types of cells—mucocytes and serocytes. Mucocytes are larger, occupy the central parts of the terminal sections, serocytes are located on the periphery, forming serous crescents, the so-called. crescent of Januzzi, characteristic of mixed terminal sections. Outside the serous crescents lie myoepithelial cells. Intralobular ducts of the pancreas. pass into interlobular, then interlobar, and the latter merge into the submandibular duct.
Physiology and biochemistry
P. g. - see Salivary glands.