Topographic anatomy of the lateral vault - temporal region
Region boundaries. Lower - zygomatic arch (arcus zygomaticus) and infratemporal crest of the temporal bone (crista mfratemporalis);
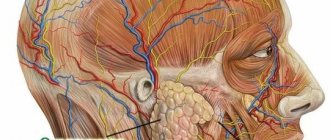
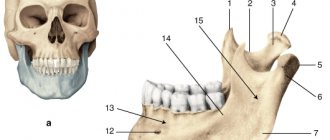
upper, anterior and posterior - correspond to the arcuate line of attachment of the temporal muscle (Hh. temporalis superior). Layer structure. The skin is thin, mobile, partially covered with stripes. Subcutaneous tissue is loose, moderately expressed. 1-2 cm anterior to the auricle in the tissue passes a. temporalis superficialis, accompanied by the vein of the same name and n. auriculotemporalis. Above the anterior third of the zygomatic arch, the r. frontalis rises to the frontal muscle, and the r. rises to the orbicularis oculi muscle. zygomaticus of the facial nerve. The temporal aponeurosis (fascia temporalis) consists of two leaves that diverge above the zygomatic arch and are attached to the outer and inner surfaces of the latter, forming a closed interaponeurotic cellular space. Between the deep layer of the temporal aponeurosis and the outer surface of the temporal muscle there is a subgaleal cellular space. Above, in front and behind, this space is limited by the attachment of the temporal aponeurosis to the frontal, parietal and temporal bones. In a downward direction, the fiber continues along the temporal muscle until the latter attaches to the coronoid process of the lower jaw. Behind the zygomatic arch, it closes with the submasseterial tissue and then with the fatty accumulation of the cheek (corpus adiposum Bicnat). The temporal muscle (m. temporalis) performs the temporal fossa. It starts from the entire surface of the temporal fossa along the upper to lower temporal lines. Fan-shaped muscle fibers form a powerful tendon that attaches to the coronoid process of the lower jaw. In the thickness of the muscle (sometimes between the muscle and the periosteum of the temporal bone) there are branches of the deep temporal artery (a. temporalis profunda). Between the inner surface of the muscle and the periosteum of the squama of the temporal bone is the axillary tissue space of the temporal bone. The fiber located here directly communicates with the temporopterygoid and subtemporal cellular spaces. Thus, in the temporal region, the following localizations of the purulent-inflammatory process are possible: in the subcutaneous tissue, in the interaponeurtic, subaponeurotic, and axillary tissue spaces.
Complications
In very severe cases of phlegmon of the maxillofacial area, purulent exudate can spread into the subcutaneous tissue and directly into the skin, followed by their destruction. In places of erosion, pus flows freely, which often leads to self-healing.
Due to its rapid spread, this pathology can cause the following dangerous complications :
- Osteomyelitis of the bone structures of the head.
- Mediastinitis.
- Meningitis.
- Brain abscess.
- Destruction of the walls of large vessels.
All these complications can end the patient’s life, so the doctor’s main task is to correctly diagnose phlegmon of the maxillofacial area and prescribe competent treatment .
Characteristic local signs of abscess, phlegmon of the temporal region
Complaints of pulsating pain in the temporal region, the intensity of which depends on the depth of localization of the infectious-inflammatory process: the deeper the purulent-inflammatory focus is located, the more intense the pain.
Objectively. There is asymmetry of the face due to swelling of the tissues of the temporal region, the severity of which depends on the prevalence of the infectious-inflammatory process and its localization: the more superficial the purulent-inflammatory focus is located, the greater the swelling of the tissues and the brighter the hyperemia of the skin above the inflammatory infiltrate. Palpation of the infiltrate causes pain. When the process is localized in the subcutaneous fatty tissue, the inflammatory infiltrate often does not have clear boundaries and can spread to neighboring anatomical areas (frontal, parotid-masticatory, zygomatic, eyelid area), while the inflammatory infiltrate with an abscess, phlegmon of the subgaleal, axillary retinal space at the top is strictly limited by the temporal region - the line of attachment of the temporal aponeurosis. With an abscess of the interaponeurotic space, the inflammatory infiltrate occupies the lower part of the temporal region and has a clearly defined border along the zygomatic arch. Dysfunction in the form of limited mouth opening due to inflammatory contracture of the temporal muscle can be observed with an abscess, phlegmon of the subgaleal cellular space and, especially clearly, when the purulent-inflammatory focus is localized in the axillary cellular space.
Topical diagnosis of abscesses and phlegmons of the face.
The effectiveness of surgical intervention in patients with abscesses and facial phlegmon largely depends on the accuracy of topical diagnosis of a purulent focus. In case of abscess and phlegmon of anatomical areas that have a layer-by-layer structure, topical diagnosis consists of clarifying the layer in which the focus of purulent inflammation is localized. In this case, it is fundamentally important to resolve the issue of the level of localization of the inflammatory process in a patient: superficial or deep .
Variants of localization of abscesses (phlegm) of the temporal region:
I - in subcutaneous tissue; II - in the interaponeurotic (interfascial) space; III - in the subfascial cellular space; IV in the axillary tissue space. Inflammatory processes in the cellular spaces of the face and neck are manifested by subjective and objective symptoms. Subjective symptoms are pain (dolor) and dysfunction (functio lacsa), and objective symptoms are swelling (tumor), redness (rubor), increased local temperature (calor). Depending on the localization of the process in different areas of the face, these main symptoms are not always expressed to the same degree.
The most characteristic symptoms of abscess and phlegmon of the face of various locations.
Limitation of mouth opening: 1 - temporal region (axillary space); 2 - infratemporal fossa; 3 - chewing area (masticatory space); 4 - interpterygoid and pterygomaxillary spaces.
Swallowing problems due to pain: 5 - peripharyngeal space; 6 - soft palate; 7 - sublingual area; 8 - area of the submandibular triangle; 9 - body and root of the tongue.
Swelling, hyperemia of the skin: 10 - frontal area; 11 - temporal region (subcutaneous tissue); 12 - eyelid area; 13 - zygomatic region; 14 - infraorbital region; 15 - upper lip; 16 - buccal area; 17 - lower lip; 18 - chin area. Pain is a companion to inflammation of any location. They are more often spontaneous, intensifying when palpating the inflamed area, swallowing movements, or when trying to open the mouth or move the jaw. Sometimes pain appears only when examining and applying pressure to the inflamed area of tissue. Often there is irradiation of pain along the branches of the trigeminal nerve and sympathetic plexuses. Due to pain and increasing inflammation, symptoms of dysfunction of chewing, swallowing, speech, and sometimes breathing appear. In some localizations of the process, swallowing, and, consequently, the patient’s nutrition is significantly impaired. In other localizations, more or less significant restrictions on jaw movements occur. The combination of these symptoms can often be a differential diagnostic sign for some localizations of phlegmon, facilitating their topical diagnosis. Inflammatory hyperemia that appears on the skin or mucous membrane does not always occur at the beginning of the disease; more often it is a sign of later stages of inflammation, beginning to suppurate. Earlier and more often it appears with superficial localization of phlegmon in the submandibular triangle, in the submental area, on the cheek. With deep phlegmon (pterygomaxillary, parapharyngeal space), inflammatory hyperemia on the skin does not appear in the initial stages, and if it does appear, it is in advanced stages of the disease. With these localizations, phlegmon should be looked for on the mucous membrane of the oral cavity or pharynx. During an external examination of the face, the tumor is also not detected in all locations of phlegmon. Thus, with deep phlegmon of the lateral area of the face, swelling and even swelling on the outer surfaces of the face may not appear for a long time. This sign can most likely be noticed when examining the oral cavity, pharynx, and sometimes only by examining the finger, comparing palpation data with the healthy side. The formation of an abscess, the accumulation of exudate in a closed cavity, is manifested by another symptom - fluid fluctuation . It is necessary to distinguish between a false fluctuation, which occurs when tissue edema, and a true fluctuation, which appears when purulent exudate accumulates in a closed cavity. The symptom of true fluctuation is determined in this way: the index finger of one hand is placed motionless on the edge of the infiltrate, and a jerk-like pressure is applied with the finger of the other hand on the opposite side of the infiltrate. In the presence of fluid and tissue, the immobile finger feels shocks transmitted through the bone vein; but this feeling may be false. The same should be repeated in another direction, perpendicular to the first. The sensation of tremors even with the new position of the fingers will indicate the presence of fluid (pus) in a closed cavity. The symptom of true fluctuation indicates the need for an incision. With deep localizations of phlegmon, the absence of a symptom of fluctuation is not a contraindication to the incision. When phlegmon occurs in the pterygomaxillary space or in the infratemporal fossa, paresthesia or anesthesia of the skin sometimes appears in the area of the branching of the mental nerve due to compression of the mandibular nerve by infiltrate (Vincent's symptom), which most often manifests itself in fractures of the body of the jaw, due to nerve damage, in osteomyelitis ( if the inflammatory exudate covers the walls of the jaw canal). Difficulty swallowing - a common symptom with phlegmon of the tongue, sublingual region, floor of the mouth, pterygomaxillary and parapharyngeal space - can occur due to pain when trying to swallow, but with some effort food can move through the pharynx and pharynx into the esophagus. In other cases, due to swelling or infiltration of the tissues of the pharynx and pharynx, a mechanical obstacle occurs to the passage of food and even liquid into the esophagus. Sometimes liquid food can enter the nasopharynx and flow out through the nose when swallowed. This is explained by the spread of edema and infiltration to the soft palate, which ceases to act as a valve separating the nasopharynx and oropharynx at the time of food movement. This phenomenon should be distinguished from paresis or paralysis of the muscles of the soft palate, which occurs as a complication of diphtheria of the pharynx or other diseases of the nervous system. Contracture of the masticatory muscles, which limits the mobility of the lower jaw , occurs when the masticatory, temporal or medial pterygoid muscles are involved in the inflammatory process.
In other cases, cramping occurs due to a reflex contraction of the mouse in response to pain, although the muscles themselves are not yet inflamed. In rare cases, with widespread phlegmon of the floor of the mouth or tongue, patients complain of difficulty breathing or a feeling of lack of air. This condition, caused by mechanical obstacles to the flow of air into the lungs and threatening asphyxia, is often observed and is caused by dislocation and stenotic asphyxia. It is possible with severe phlegmon with extensive swelling and infiltration of the walls of the pharynx, complicated by swelling of the mucous membrane of the epiglottis or larynx. Thus, taking into account the different localization of inflammatory processes, this classification of phlegmons of the face and neck can be used according to the topographic-anatomical principle with classification based on functional disorders. For superficial abscesses and phlegmons of the maxillofacial area, the following are most characteristic: 1 - swelling of tissues; 2 - redness of the skin and mucous membrane over the site of inflammation; 3 - local increase in tissue temperature. At the same time, for deep abscesses and phlegmons of the maxillofacial area the most characteristic are: 1 - pain; 2 - dysfunction of chewing, swallowing and breathing. With phlegmon, damage to two, three or more anatomical areas and cellular spaces is often observed, which makes the clinical picture of the disease more diverse and topical diagnosis more complex.
Method of operation for opening an abscess, phlegmon of subcutaneous fatty tissue of the temporal region
When the inflammatory focus is localized in the subcutaneous fat, Fig. 18, A):
1. Anesthesia - local infiltration anesthesia with premedication, anesthesia
2. A radial skin incision in the temporal region (Fig. 18, B) is made through the middle of the inflammatory infiltrate along its entire length.
3. If found in a wound a. et v. temporalis superficialis or their large branches, the vessels are isolated, ligated and crossed to prevent arrosive bleeding in the postoperative period (Fig. 18, C, D, E).
4. By exfoliating the subcutaneous fat with a hemostatic clamp, the cavity of the purulent-inflammatory focus is opened and the pus is evacuated (Fig. 18, E).
5. Gauze turunda or tape drainage made from rubber gloves or plastic film are loosely inserted into the surgical wound (Fig. 18, G).
6. Apply an aseptic cotton-gauze bandage with a hypertonic solution and antiseptics.
Technique for opening an abscess in the interaponeurotic space of the temporal region
1. Anesthesia - local infiltration anesthesia with premedication, anesthesia.
2. Skin incision along the upper edge of the zygomatic arch (Fig. 19, A, B).
3. Using a hemostatic clamp, subcutaneous fat is peeled off from the outer surface of the temporal aponeurosis 0.5-1 cm upward from the edge of the zygomatic arch (Fig. 19, B).
4. The superficial layer of the temporal aponeurosis is dissected at the site of its attachment to the temporal arch for 1.5-2 cm (Fig. 19, D).
5. A hemostatic clamp is inserted into the interaponeurotic space and the tissue is separated, the purulent focus is opened, and the pus is evacuated (Fig. 19, E).
6. A tape drainage made of rubber gloves or plastic film is inserted into the wound (Fig. 19, E).
7. Aseptic cotton-gauze bandage with hypertonic solution, antiseptics.
Method of operation for opening an abscess of the axillary cellular space of the temporal region
When the inflammatory focus is localized under the temporal muscle (Fig. 21, A):
1. Anesthesia - anesthesia or local infiltration anesthesia accompanied by premedication.
2. Radial skin incision in the temporal region through the middle of the inflammatory infiltrate along its entire length (Fig. 21, B).
3. If found in a wound a. et v. temporalis superficialis or their large branches, the vessels are isolated, ligated and crossed to prevent arrosive bleeding in the postoperative period (Fig. 21, C, D, E).
4. Having grabbed and lifted the temporal aponeurosis with two tweezers, cut it in an area of 0.5-0.7 cm (Fig. 21, E).
5. Through the incision, a hemostatic clamp is inserted into the subgaleal cellular space, and then the temporal aponeurosis is dissected over the separated jaws of the clamp along the entire length of the wound (Fig. 21, G).
6. Additionally, the temporal aponeurosis is dissected in the transverse direction in order to create conditions for better drainage of the purulent focus (Fig. 21.3).
7. Using a hemostatic clamp, the fibers of the temporal muscle are moved apart over the inflammatory infiltrate, bluntly exfoliating the tissue with the clamp, penetrate into the axillary tissue space, open the purulent-inflammatory focus and evacuate the pus (Fig. 21, I).
8. A tubular drainage is inserted into the axillary tissue space through the surgical wound (Fig. 21, K), which allows irrigating, washing the wound with antiseptic solutions, and performing vacuum drainage.
9. Aseptic cotton-gauze bandage with hypertonic solution, antiseptics.
Method of operation for opening phlegmon of the axillary space of the temporal region
With phlegmon of the axillary space (Fig. 22, A):
1. Anesthesia - anesthesia or local infiltration anesthesia accompanied by premedication.
2. An arcuate skin incision above the upper line of attachment of the temporal muscle to the temporal bone (Fig. 22, B).
3. Using a hook, pull the lower edge of the wound down, isolate, bandage and cross the large branches of a. et v. temporalis superficialis (Fig. 22, C, D).
4. Cross the temporal aponeurosis and temporalis muscle along lin. temporalis superior (Fig. 22, D).
5. Peeling off the temporal muscle from the place of its attachment to the temporal bone with a raspatory, they enter the axillary tissue space, open the purulent-inflammatory focus, and evacuate the pus (Fig. 22, E).
6. A tubular drainage is inserted into the axillary tissue space, allowing for washing, irrigating the wound with antibiotics, enzymes, and performing vacuum drainage (Fig. 22, G).
7. Aseptic cotton-gauze bandage with hypertonic solution, antiseptics.
Did you like the article? Share with friends
0
Similar articles
Next articles
- Abscess, phlegmon of the eyelids
- Abscess, phlegmon of the infraorbital region
- Abscess, phlegmon of the mouth area
- Abscess, phlegmon of the nose area
- Abscess, phlegmon of the chin area
Previous articles
- Abscess, phlegmon of the middle vault
- Methods of conduction anesthesia in the head and neck area
- Treatment planning for patients with acute odontogenic infection, taking into account the prognosis of the disease
- Principles of surgical treatment of patients with abscesses, phlegmon of the head and neck
- Topical diagnosis of abscesses, phlegmons of the head and neck
Classification and clinical manifestations of pathologies
A.I. Evdokimov and G.A. Vasiliev distinguished in his articles:
- periodontitis;
- periostitis;
- osteomyelitis;
- soft tissue damage.
This classification is the most popular.
Based on the nature of the pathogen, they are distinguished:
- anaerobic (microbes develop in the absence of oxygen);
- aerobic (needs air for development).
According to the location of the affected area, phlegmon is distinguished:
- The deep space of the neck is affected and inflammation descends to the jugular cavity.
- The pathological process moves to the mediastinum, mediastinitis begins.
- Pus is located in the mediastinum, regardless of the severity of tissue damage.
Regardless of the location of the source of infection, the disease is considered serious and requires urgent treatment.
Symptoms of phlegmon of the neck
The location of the phlegmon turns red and hurts, the local temperature rises
A characteristic feature is the acute and sudden onset of the disease:
- There is a high body temperature (more than 38 degrees). The patient's condition worsens every hour.
- There is noticeable redness and severe swelling on the neck.
- Difficulty and painful swallowing.
- Pain at the site of infection, which intensifies when the tissue is displaced to the side.
- The vessels on the affected side dilate noticeably.
- The lymph node is inflamed and enlarged.
- Possible breathing problems.
- In some cases, an adult patient develops functional torticollis as a reliable sign of phlegmon.
Severe hyperemia is visually noticeable; upon palpation, greater heat is felt (compared to the patient’s general body temperature), the skin is tense. All touches are extremely painful.
Intensely increasing intoxication leads to a severe general condition, putrefactive-necrotic phlegmons of the face and neck appear. Symptoms:
- dyspnea;
- frequent intermittent shallow breathing;
- pulse quickens;
- hyperemia and swelling increase;
- against the background of severe intoxication, confusion may appear;
- a violation of water-electrolyte metabolism develops.
The situation requires urgent hospital treatment.
Symptoms of a neck abscess
It involves the formation of a cavity of connective tissue, which acts as a protective capsule within which the inflammatory process occurs. The symptoms are as follows:
- low-grade fever;
- pain in the area of inflammation;
- swelling of the site of infection;
- redness of the skin in the affected area.
The course is slower than with phlegmon, which is often a complication of an abscess.