The frequency of development of abscesses and phlegmon of the maxillofacial area of the head is due to the high prevalence of chronic focal odontogenic and tonsillogenic infections, as well as infectious and inflammatory lesions of the skin and oral mucosa. Based on data on the localization of the infectious-inflammatory process in various anatomical sections, zones, regions, as well as spaces of the head and neck, their systematization is built. From the description of the topographic-anatomical structure of the areas of the face, the perimandibular and adjacent areas of the neck, one can see the complexity of their anatomy. There are many cellular spaces, numerous lymph nodes and vessels scattered throughout all areas of the face, an abundant network of arteries and veins with rich innervation of these areas.
Classification of abscesses and phlegmons of the face.
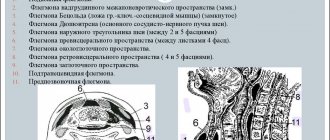
To facilitate the recognition and treatment of lymphadenitis, phlegmons and facial abscesses of various localizations, one should have an idea of the classification of inflammatory processes, which can be based on both topographic-anatomical and clinical signs of the disease (Zhakov M.N., 1969). A. Cellulitis and abscesses of the lateral surface of the head and neck. I. Cellulitis and abscesses of the temporal region. I. Phlegmons and abscesses of the lateral surface of the face: - buccal area; - chewing area; - parotid-masticatory area. III. Phlegmons and abscesses of the supraglottic region: - submandibular region; - submental area. B. Cellulitis and abscesses of the deep lateral region of the face, oral cavity, pharynx and pharynx. I. Phlegmons and abscesses of the deep lateral area of the face: - pterygo-maxillary space; - interpterygoid space; - temporopterygoid space. II. Phlegmons and abscesses of the oral cavity, pharynx, pharynx: - sublingual area; - language; - peri-almond fiber; - peripharyngeal space; - floor of the mouth. B. Diffuse phlegmon, involving two or more cellular spaces. I. Phlegmon of the floor of the mouth. II. Submandibular phlegmon and tissue of the vascular bed of the neck. III. Phlegmons of the interpterygoid, temporal and subtemporal regions. Orbital phlegmon. IV. Phlegmon of the floor of the mouth and peripharyngeal spaces. V. Cellulitis with a large number of cellular spaces involved in the inflammatory process. From a pathomorphological point of view, the basis for the division of purulent inflammatory processes into abscesses and phlegmons is the sign of delimitation of the purulent focus from the surrounding tissue structures, first by the granulation shaft of infiltrating tissue, and later by the connective tissue capsule. However, at the early stage of acute purulent inflammation, when the mechanisms for delimiting the purulent focus have not yet fully activated, clinicians base the differential diagnosis of abscesses and cellulitis on the sign of the prevalence of the inflammatory process (in length, area, volume). Thus, in case of acute purulent inflammation of a small volume of tissue space (for example, the area of the canine fossa) or damage to only part of the tissue of the anatomical area (for example, the submandibular region), an abscess is diagnosed. When clinical signs of damage to the entire tissue of the anatomical area or the spread of the inflammatory process to neighboring anatomical areas and spaces are revealed, a diagnosis of phlegmon is made. Thus, we can say that an abscess is a limited accumulation of pus in various tissues and organs with the formation of a cavity (for example, an abscess of the gluteal region, a brain abscess), and phlegmon is an acute diffuse purulent inflammation of fatty tissue, not prone to limitation. Odontogenic phlegmons most often appear on the face, which are initially localized in the chewing tissue space, in the tissue of the canine pit area or in the tissue of the floor of the mouth. The fate of the patient depends on the timeliness of the patient’s admission to the hospital, on the localization of phlegmon, on the choice of the correct methods of treatment and surgery, on the reactivity of the body: either a smooth course of the disease and recovery will follow, or complications will arise, sometimes very severe, delaying recovery for a long time. With abscesses, phlegmon of the face and neck, the following complications may occur : 1. Thrombophlebitis of the veins of the pterygoid plexus and orbital veins. 2. Thrombosis of the cavernous sinus of the skull, meningitis, encephalitis. 3. Sepsis, septicopyemia, mediastenitis. This classification of complications in abscesses and phlegmon of the face and neck is based on the topographic-anatomical principle of localization of the process. This classification included elements of a functional order, for example, dysfunctions of the organs of the initial part of the digestive system, which arise with different localization of abscesses, phlegmons of the face and neck. For example, impaired chewing occurs due to inflammatory contracture of the masticatory muscles (usually temporary), and impaired swallowing occurs due to pain or difficulty passing food through the inflamed tissues of the pharynx and pharynx. Such a classification, which takes into account dysfunctions of chewing and swallowing, can help in making the correct topical diagnosis and choosing the right treatment (Zhakov M.N., 1969) .
I. Abscesses and phlegmons of the face, not accompanied by trismus of the masticatory muscles and painful swallowing. II. Abscesses and phlegmons of the face, accompanied by painful and difficult swallowing. III. Abscesses and phlegmons of the face, accompanied by temporary trismus of the masticatory muscles. IV. Abscesses and phlegmons of the face, combined with temporary trismus of the masticatory muscles and painful, difficult swallowing. These symptoms should be identified during the initial examination of the patient. As the disease progresses, symptoms of functional impairment may change, and these changes become an indicator of improvement or worsening of the disease. Of course, there cannot be a complete correspondence between the type of abscess, phlegmon and the nature of the dysfunction, as presented above, since the degree of functional impairment is subject to significant fluctuations, and, in addition, it changes as the disease progresses. However, a correct analysis of the causes of dysfunction facilitates the recognition of the localization of phlegmon, and contributes to the establishment of an accurate diagnosis, and, consequently, correct treatment.
Forecast
With timely diagnosis and immediate initiation of treatment, the prognosis is quite favorable. After just a few weeks, the patient is able to return to his normal lifestyle. With putrefactive perimaxillary phlegmon and secondary complications, the prognosis for life is more doubtful.
Plisov Vladimir, dentist, Melitsinsky warrior
7, total, today
( 47 votes, average: 4.74 out of 5)
Enostosis of the femur: treatment and features of the disease
Dental canal filling: the essence of the procedure and possible complications
Related Posts
Topical diagnosis of abscesses and phlegmons of the face.
The effectiveness of surgical intervention in patients with abscesses and facial phlegmon largely depends on the accuracy of topical diagnosis of a purulent focus. In case of abscess and phlegmon of anatomical areas that have a layer-by-layer structure, topical diagnosis consists of clarifying the layer in which the focus of purulent inflammation is localized. In this case, it is fundamentally important to resolve the issue of the level of localization of the inflammatory process in a patient: superficial or deep .
Variants of localization of abscesses (phlegm) of the temporal region:
I - in subcutaneous tissue; II - in the interaponeurotic (interfascial) space; III - in the subfascial cellular space; IV in the axillary tissue space. Inflammatory processes in the cellular spaces of the face and neck are manifested by subjective and objective symptoms. Subjective symptoms are pain (dolor) and dysfunction (functio lacsa), and objective symptoms are swelling (tumor), redness (rubor), increased local temperature (calor). Depending on the localization of the process in different areas of the face, these main symptoms are not always expressed to the same degree.
The most characteristic symptoms of abscess and phlegmon of the face of various locations.
Limitation of mouth opening: 1 - temporal region (axillary space); 2 - infratemporal fossa; 3 - chewing area (masticatory space); 4 - interpterygoid and pterygomaxillary spaces.
Swallowing problems due to pain: 5 - peripharyngeal space; 6 - soft palate; 7 - sublingual area; 8 - area of the submandibular triangle; 9 - body and root of the tongue.
Swelling, hyperemia of the skin: 10 - frontal area; 11 - temporal region (subcutaneous tissue); 12 - eyelid area; 13 - zygomatic region; 14 - infraorbital region; 15 - upper lip; 16 - buccal area; 17 - lower lip; 18 - chin area. Pain is a companion to inflammation of any location. They are more often spontaneous, intensifying when palpating the inflamed area, swallowing movements, or when trying to open the mouth or move the jaw. Sometimes pain appears only when examining and applying pressure to the inflamed area of tissue. Often there is irradiation of pain along the branches of the trigeminal nerve and sympathetic plexuses. Due to pain and increasing inflammation, symptoms of dysfunction of chewing, swallowing, speech, and sometimes breathing appear. In some localizations of the process, swallowing, and, consequently, the patient’s nutrition is significantly impaired. In other localizations, more or less significant restrictions on jaw movements occur. The combination of these symptoms can often be a differential diagnostic sign for some localizations of phlegmon, facilitating their topical diagnosis. Inflammatory hyperemia that appears on the skin or mucous membrane does not always occur at the beginning of the disease; more often it is a sign of later stages of inflammation, beginning to suppurate. Earlier and more often it appears with superficial localization of phlegmon in the submandibular triangle, in the submental area, on the cheek. With deep phlegmon (pterygomaxillary, parapharyngeal space), inflammatory hyperemia on the skin does not appear in the initial stages, and if it does appear, it is in advanced stages of the disease. With these localizations, phlegmon should be looked for on the mucous membrane of the oral cavity or pharynx. During an external examination of the face, the tumor is also not detected in all locations of phlegmon. Thus, with deep phlegmon of the lateral area of the face, swelling and even swelling on the outer surfaces of the face may not appear for a long time. This sign can most likely be noticed when examining the oral cavity, pharynx, and sometimes only by examining the finger, comparing palpation data with the healthy side. The formation of an abscess, the accumulation of exudate in a closed cavity, is manifested by another symptom - fluid fluctuation . It is necessary to distinguish between a false fluctuation, which occurs when tissue edema, and a true fluctuation, which appears when purulent exudate accumulates in a closed cavity. The symptom of true fluctuation is determined in this way: the index finger of one hand is placed motionless on the edge of the infiltrate, and a jerk-like pressure is applied with the finger of the other hand on the opposite side of the infiltrate. In the presence of fluid and tissue, the immobile finger feels shocks transmitted through the bone vein; but this feeling may be false. The same should be repeated in another direction, perpendicular to the first. The sensation of tremors even with the new position of the fingers will indicate the presence of fluid (pus) in a closed cavity. The symptom of true fluctuation indicates the need for an incision. With deep localizations of phlegmon, the absence of a symptom of fluctuation is not a contraindication to the incision. When phlegmon occurs in the pterygomaxillary space or in the infratemporal fossa, paresthesia or anesthesia of the skin sometimes appears in the area of the branching of the mental nerve due to compression of the mandibular nerve by infiltrate (Vincent's symptom), which most often manifests itself in fractures of the body of the jaw, due to nerve damage, in osteomyelitis ( if the inflammatory exudate covers the walls of the jaw canal). Difficulty swallowing - a common symptom with phlegmon of the tongue, sublingual region, floor of the mouth, pterygomaxillary and parapharyngeal space - can occur due to pain when trying to swallow, but with some effort food can move through the pharynx and pharynx into the esophagus. In other cases, due to swelling or infiltration of the tissues of the pharynx and pharynx, a mechanical obstacle occurs to the passage of food and even liquid into the esophagus. Sometimes liquid food can enter the nasopharynx and flow out through the nose when swallowed. This is explained by the spread of edema and infiltration to the soft palate, which ceases to act as a valve separating the nasopharynx and oropharynx at the time of food movement. This phenomenon should be distinguished from paresis or paralysis of the muscles of the soft palate, which occurs as a complication of diphtheria of the pharynx or other diseases of the nervous system. Contracture of the masticatory muscles, which limits the mobility of the lower jaw , occurs when the masticatory, temporal or medial pterygoid muscles are involved in the inflammatory process. In other cases, cramping occurs due to a reflex contraction of the mouse in response to pain, although the muscles themselves are not yet inflamed. In rare cases, with widespread phlegmon of the floor of the mouth or tongue, patients complain of difficulty breathing or a feeling of lack of air. This condition, caused by mechanical obstacles to the flow of air into the lungs and threatening asphyxia, is often observed and is caused by dislocation and stenotic asphyxia. It is possible with severe phlegmon with extensive swelling and infiltration of the walls of the pharynx, complicated by swelling of the mucous membrane of the epiglottis or larynx. Thus, taking into account the different localization of inflammatory processes, this classification of phlegmons of the face and neck can be used according to the topographic-anatomical principle with classification based on functional disorders. For superficial abscesses and phlegmons of the maxillofacial area, the following are most characteristic: 1 - swelling of tissues; 2 - redness of the skin and mucous membrane over the site of inflammation; 3 - local increase in tissue temperature. At the same time, for deep abscesses and phlegmons of the maxillofacial area the most characteristic are: 1 - pain; 2 - dysfunction of chewing, swallowing and breathing. With phlegmon, damage to two, three or more anatomical areas and cellular spaces is often observed, which makes the clinical picture of the disease more diverse and topical diagnosis more complex.
Clinical picture of the disease
In the initial stages, abscesses and phlegmons adjacent to the lower jaw are manifested by compaction and progressive swelling of the soft tissues of the face. The skin over the purulent focus is often hyperemic. The key symptom of suppuration is fluctuation - the feeling of fluid in a confined space.
The course of phlegmon is accompanied by general intoxication, in which the patient presents the following complaints:
- malaise and feeling of chronic fatigue;
- increase in body temperature;
- fatigue and joint pain.
Abscesses, as a rule, do not cause such symptoms due to the limited nature of the pathological process.
Abscess, phlegmon of the maxillofacial area in children is characterized by an acute and severe course of the disease. Diffuse purulent lesions of soft tissues are formed as a result of the imperfection of the children's immune system.
General principles of opening abscesses and facial phlegmons.
The basic principle of treatment of inflammatory diseases of the facial part of the head is based on the common biological laws of wound healing - the unity of the pathogenesis of the wound process (N.N. Bazhanov, D.I. Shcherbatyuk, 1992). Centuries-old surgical practice has developed a general rule for the treatment of any purulent process - opening the source of inflammation and draining it (L.E. Lundina, 1981; V.G. Ivashchenko, V.A. Shevchuk, 1990). Complete drainage reduces pain, promotes the outflow of wound fluid, improves local microcirculation, which naturally has a beneficial effect on local metabolic processes, the transition of the wound process to the regeneration phase, reducing intoxication and interstitial pressure, limiting the necrosis zone and creating unfavorable conditions for the development of microflora (Yu. I. Vernadsky, 1983: A.G. Shargorodsky et al., 1985; D.I. Shcherbatyuk, 1986; Sh.Yu. Abdullaev, 1988). Thus, the principle “Ubi pus, ibi evacuo” in the treatment of patients with abscesses and phlegmons of the face is implemented: I. Opening a purulent focus by layer-by-layer dissection and stratification of the tissues above it. II. Drainage of the surgical wound in order to create conditions for the evacuation of purulent exudate.
Opening of a purulent focus.
The incisional drainage method of treating phlegmons and soft tissue abscesses is quite widespread to this day. It involves opening a purulent focus and open wound management in the postoperative period. The incisional drainage method is a classic one; in general, it determines the tactics in the treatment of acute purulent diseases of soft tissues and purulent wounds. Opening of the purulent focus is carried out by external access from the skin, or intraoral access from the mucous membrane. When choosing an operative approach, the following requirements must be observed : 1. The shortest path to the purulent focus. 2. The least likelihood of damage to organs and formations during tissue dissection on the way to the purulent focus. 3. Complete drainage of the purulent focus. 4. Obtaining an optimal cosmetic effect from the postoperative wound. During the operation of opening an abscess (phlegmon), the skin, mucous membrane, and fascial formations above the purulent focus are dissected; the muscles are cut off, peeled off from the place of attachment to the bone of the temporal, medial pterygoid and chewing muscles (m. temporalis, i.e. pterygoideus mcdialis, i.e. masseter) or using a hemostatic clamp, the muscle fibers of the temporal, mylohyoid and buccal muscles (m. temporalis) are pulled apart , T. mylohyoideus, T. buccalis). The exception is the subcutaneous muscle of the neck (m. platysma) and often the mylohyoid muscle, the fibers of which intersect in the transverse direction. which ensures the wound gapes and creates good conditions for the outflow of purulent exudate. Loose tissue located on the way to the purulent focus, in order to avoid damage to the vessels, nerves, and excretory flow of the salivary glands located in it, is stratified and pulled apart with a hemostatic clamp.
Drainage of a purulent focus.
After opening the abscess and phlegmon, a stream of antiseptic solution (sodium hypochlorite) injected into the wound under pressure using a syringe, evacuate (wash out) the purulent exudate. Then drainage is inserted into the wound. In clinical practice, in patients with abscesses and phlegmons of the face, drainage of a purulent wound is most often used : - using tape drainages made of rubber gloves; - using carbon adsorbents introduced into the wound in the form of granules. cotton wool, carbon fiber wicker products; - by wound dialysis; — intermittent or continuous aspiration of exudates from the wound using an electric suction, ensuring the creation of a constant vacuum in the wound-drainage system. In case of putrefactive-necrotic phlegmon, in order to reduce intoxication of the body, necrectomy is performed - excision of non-viable tissue. To speed up the cleansing of the wound from necrotic tissue, it is advisable to use local levomikol, sodium hypochlorite, as well as expose the wound to ultrasound, a magnetic field, and a low-energy helium-neon laser. Drainage of a purulent wound by dialysis, vacuum suction of exudate, the use of sodium hypochlorite, etc. are indicated in the first stage of the wound process - in the stage of hydration and cleansing of the wound. The appearance of granulation tissue in the wound indicates the onset of the second stage of the wound process - the stage of dehydration. At this stage of the wound process, it is advisable to use dressings (tampons) with various ointments that prevent damage to granulation tissue during dressing changes and have a positive effect on the course of the reparative process. To reduce the duration of the rehabilitation period and form a more delicate scar, after cleansing the wound of non-viable tissue, its edges can be brought together by applying a so-called secondary suture. Physiotherapy helps speed up the elimination of residual inflammation. reduce the likelihood of relapse of the infectious-inflammatory process and the occurrence of complications such as actinomycosis. Often, in order to reduce the time of treatment of postoperative wounds of patients with abscesses and phlegmons of the maxillofacial areas, it is more advisable for surgeons to perform secondary surgical treatment. Secondary surgical treatment of the wound, in the inflammation phase, involves, first of all, the elimination of all non-viable tissues, the removal of pockets, foreign bodies, and hematomas. It ends with a secondary situational suture, creating, if possible, a position in which the walls of the wound channel are in contact at all levels. At a later stage, in the regeneration phase, when the wound surface is cleaned and granulated with the formation of a protective granulation shaft in the peri-wound area, secondary surgical treatment can only consist of the application of a secondary situational suture. Finally, in the third phase of the wound process, during secondary surgical treatment of the wound, scar tissue is excised and a secondary situational suture is applied, bringing the walls and edges of the wound canal together until they touch. Thus, secondary surgical treatment of the wound ends with the application of a secondary situational suture. In the future, in the absence of complications and a new inflammatory process, the sutures are made airtight.
Surgical approaches on the face.
Based on the anatomy of the branches of the facial nerve, it is recommended to make incisions on the face, choosing “neutral” spaces between them.
Diagram of typical incisions on the face.
There are two methods of opening phlegmon of the maxillofacial area: extraoral and intraoral . The oral method is used in cases where surgery on the part of the oral cavity does not provide complete drainage of the cellular space or is impossible due to concomitant trismus of the masticatory muscles. The intraoral method is rarely used. Rules for making typical incisions on the face. 1. First, the skin or mucous membrane is dissected, and then the fascial formations above the purulent focus. 2. The muscles are cut off from the place of attachment, with the exception of the subcutaneous muscle of the neck and the mylohyoid muscle, the fibers of which are crossed in the transverse direction, which ensures the effect of a gaping wound and creates good conditions for the outflow of purulent contents. 3. Blunt advance to the purulent focus (digital or instrumental).
When compiling the article, materials from the book were used: Sergienko V.I. and others. “Operative surgery of abscesses, phlegmon of the head and neck,” 2005.