How can you get a cold on the facial nerve?
The anatomical location of the facial nerve is quite confusing. It passes through the facial canal of the temporal bone and exits into the auditory canal. At this point it intersects with the intermediate nerve.
It is quite easy to get colds in the maxillofacial area. However, this disease is similar in symptoms to others. It is important not to self-medicate, but to consult a specialist in time.
The nervous system is complex. The skin and muscles are equipped with nerves that intersect with each other. When viruses damage the facial muscles of the face, neuritis or neuropathy of the facial nerve develops. Neuritis is inflammation of a nerve. Neuropathy is a disease that causes unilateral paralysis of the facial muscles.
Massage and gymnastics for the face
Massage is prescribed by a doctor to increase blood circulation in tissues and actively remove metabolic products. A course of massage helps speed up treatment. It should only be carried out by a specialist.
All movements during the session should be light, not strong. Shown:
- Stroking the neck, cheeks, forehead and back of the head;
- smooth rubbing of the lower part of the neck to the shoulders (until slight redness of the skin appears);
- slight vibration of the skin in the cheekbones and forehead;
- light massaging movements in the area of the brow ridges, nasolabial folds and nose.
Important! A massage therapist must have appropriate training to avoid causing harm to health through negligence.
Facial exercises are prescribed after the end of treatment in order to restore mobility to the facial muscles. The doctor should select exercises in such a way as to target specific facial muscles.
The set of exercises is quite simple, and the patient can perform them independently, using the schemes suggested by the doctor. They should be carried out without strong tension, calmly and alternated with complete muscle relaxation.
Example exercises:
- Bringing the eyebrows to the bridge of the nose and moving them back to their original position;
- folding the lips into a “tube” and returning to their normal state;
- clenching and unclenching of teeth;
- blow on a “feather”, “blow out a candle”, etc.
All exercises are done 5-7 times, with short pauses. They will help avoid stagnant processes and restore facial expressions.
Causes of the disease
Coldening the facial nerve means giving access to pathogenic microbes into the body. They disrupt the supply of nerves to tissues. Statistically, in 90 percent of cases, when a person cannot control the movements of the facial muscles during a cold and experiences pain, this is a sign of a cold facial nerve.
The causes of the disease are also serious lesions, such as:
- head injury;
- middle ear disease;
- hypothermia;
- lesions during pregnancy;
- diabetes;
- borreliosis;
- spinal paralysis;
- damage to the central nervous system;
- tumors;
- ischemia;
- stroke;
However, most facial nerve paresis occurs due to hypothermia. Therefore, during the cold season, you need to be especially careful about yourself, dress warmly, and avoid hypothermia.
Trigeminal neuralgia
In most cases, entrapment of the trigeminal nerve on the face is due to the following reasons:
- multiple sclerosis;
- hypothermia;
- malocclusion;
- muscle strain;
- vascular aneurysms;
- viral and bacterial infections.
If a person has a cold in the jaw nerve, the development of the inflammatory process will be signaled by:
- pain while chewing;
- numbness in the lower part of the face;
- increased salivation;
- involuntary contraction of the jaw muscles;
- skin hypersensitivity.
Types of disease
- Epidemic parotitis - in this case, intoxication of the body occurs due to viruses.
- Otitis – Otitis media leads to perforation of the eardrum, causing infection in the facial nerve.
- Hunt's syndrome - a herpetic rash occurs on the anterior part of the tongue and ear. Due to the penetration of microbes, the salivary glands become inflamed, resulting in compression of the facial nerve.
- Merkenson-Rosenthal syndrome is a rare type of neuritis that is hereditary.
Symptoms of facial nerve disease
If a person has a cold on the facial nerve, symptoms of the lesion appear in the form of unilateral or bilateral lesions. Often the affected part of the face (cheek, ear, chin) may become painful or numb. In 90 percent of cases, paresis is unilateral. The reason for this is that the temporal portion of the facial nerve is the most vulnerable.
Paresis (prosoparesis) is a decrease in voluntary movements of facial muscles. It has significant differences from paralysis. Paresis involves only partial impairment of muscle function.
The problem in diagnosing the disease is that paresis is not easy to notice (especially in mild forms of the disease). It only appears when a person speaks.
Paresis is divided into mild and severe. The mild form is characterized by minor changes in facial expressions in conversation. Severe paresis is a very indicative symptom of the disease. Such a defeat is expressed in the fact that the face turns into a mask. It is difficult for the victim to puff out his cheeks and close his eyes. Also, these movements are accompanied by pain.
Pathological synkinesis is divided into eyelid-labial and eyelid-frontal. In the first case, when the eyelid lowers, the corner of the mouth rises. In the second, when the eyelid droops, the forehead wrinkles.
The causes of paresis are:
- Fiber compression.
- Nerve damage.
The first reaction of neuritis is usually drooping of half the face and lacrimation
Paralysis is also observed in the following:
- it is difficult for a person to speak;
- the victim has difficulty swallowing;
- the patient experiences lacrimation and salivation;
- there is a lack of sensation of taste of food;
- there are painful sensations in the face that are shooting in nature;
- the corners of the mouth and eyebrows (on the right or left side of the face) are lowered;
- difficulty closing your eyes;
- the victim feels pain in the ear, jaw;
- asymmetry of the facial muscles occurs;
- it is difficult for a person to whistle and puff out his cheeks;
- Sometimes the patient experiences eye twitching.
Thus, the main symptoms are expressed in high or reduced skin sensitivity; facial pain; malfunction of the salivary and lacrimal glands; numbness; pain inside the face (usually aching or dull); problems with facial expressions (reflected on the part that is cold).
Signs of the disease also differ depending on the phase. In the acute course of the disease, the lesion can be very visible, in this case the degree of facial distortion is very large.
Secondary symptoms
If the trigeminal nerve is inflamed, then along with unbearable pain the patient may experience other manifestations:
- swelling and redness of the eyelids;
- uncontrolled, increased salivation;
- tearing eyes;
- violation of taste buds;
- numbness of the face;
- sleep problems;
- weakness and chills;
- muscle spasms;
- facial asymmetry;
- pallor and redness of the skin;
- dry or oily skin;
- rashes and itching on the skin of the face;
- headache;
- painful tic on the face;
- distorted facial expressions and grimaces;
- increased body temperature;
- insomnia, irritability, anxiety.
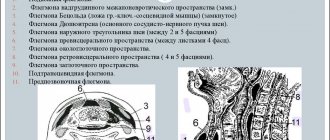
In the following image you can see how the face changes with facial neuralgia:
Diagnostics
When the facial nerve is blown, at the first signs of the disease you need to consult a doctor, preferably a neurologist. Otherwise, the person may become increasingly worse. The diagnosis is often visible from the person's face. It's skewed, only one half moves. The asymmetry of movements of the left and right sides of the face is also visible.
Based on the patient’s story about how the facial nerve hurts, as well as on the visual picture, often an experienced doctor can make a diagnosis without additional examinations.
But since the cause of the development of facial neuritis is of great importance, the doctor often prescribes tests. After all, tumors and inflammation can be factors in the development of the disease, and the disease can also be a symptom of a stroke.
When making a diagnosis, the doctor also needs to determine the nature of the damage, i.e., the depth of the paresis.
What tests does the doctor prescribe:
- Complete blood count (finger prick). Together with other symptoms, this analysis may indicate meningitis, otitis media and other long-term illnesses.
- MRI. Very accurate method. Detects tumors, signs of heart attack, inflammation of the membranes of the brain, abnormal development of blood vessels.
- CT. A CT scan can also reveal certain symptoms that cause neuritis. These are tumors, brain hematomas, symptoms of a stroke.
- Electroneurography (study of the speed of an electrical signal that travels along a nerve), electromyography (study of electrical impulses arising in muscles).
Treatment methods
Self-medication is unacceptable here. When the doctor discovers that the facial nerve is cold, treatment usually begins without delay. For greater effectiveness, it is comprehensive.
Usually the doctor prescribes medications, including:
- Pharmaceuticals.
- Decongestant medications (they relieve swelling).
- Diuretics (remove excess moisture, dilate coronary vessels).
- Drugs that increase the sensitivity of nerve tissue.
- Substances to maintain muscle tissue in tone (preventing infection).
- Vasodilators (allow you to saturate the tissues with oxygen).
- Painkillers (relieve pain).
When is surgery used?
The help of a surgeon in treating the disease is needed only when other methods do not help. This happens infrequently, because with timely treatment the disease is well treated.
If surgery is prescribed, the surgeon’s actions involve destruction of the facial nerve. Special drugs are injected into the site of nerve damage to reduce its sensitivity and susceptibility.
Nerve fiber decompression is performed in difficult cases. During this, the doctor changes the position of the arteries located near the nerve. After this procedure, the discomfort does not go away immediately, but only after a few months.
Surgery should be resorted to only in extreme cases. It has negative features:
- Not every patient can tolerate general anesthesia;
- After the operation, a scar remains.
Neuritis of the facial nerve in a child
The causes of damage to the facial nerve in a child can be as many as in an adult: hypothermia;
- inflammation of the middle ear;
- damage to the facial nerve itself.
A reliable symptom of the development of the disease is the skewing of the mouth in the healthy direction when trying to bare teeth. Treatment of the disease in younger patients depends on its etiology, but usually recovery occurs within 2-3 weeks. In some cases (when the cause is a serious illness), more time is required.
During therapy for fever, antipyretics are prescribed. In the acute phase of neuritis, anti-inflammatory and vasoactive medications are also prescribed. During the remission phase, exercises may be prescribed, which the child performs first with a doctor and then with a parent.
Symptoms of neuralgia
When the facial inflammation occurs, the functions of the muscles of the forehead, eyebrows, cheeks and jaw are disrupted. The most painful parts are the chin and the area around the eyes. As a rule, neuralgia appears on one side of the face, but in rare cases a bilateral form occurs.
The sensations may vary, but there are common manifestations that indicate inflammation of the facial nerve: burning-twitching pain in the nasolabial triangle, which lasts from a few seconds to 2-3 minutes. Then the pain subsides, but quickly spreads to other parts of the face nearby.
Important! With facial neuralgia, inflammation most often affects only one half of the face.
During an attack of sharp spontaneous pain, a person suddenly freezes in place and is unable to move further. The skin first turns pale and then may turn red. The first response is to rub the affected part of the face with the palm of your hand. Sharp pain can radiate to other parts of the head: teeth, ear, scalp.
As a result, the following symptoms may appear:
- lacrimation;
- burning in the place where the pain was most intense;
- increased salivation and uncontrolled drooling;
- spots on the skin or redness;
- reduction of pain when pressing;
- deformation of the lips when opening the mouth;
- eyelids do not close completely;
- the person does not fully move his lips (cannot fold them into a tube and kiss);
- pain does not bother you at night;
- may appear near the ear.
All these symptoms complicate normal activities: eating, brushing teeth, speaking loudly, etc.
For everyone who suffers from facial neuralgia, the sensations are individual. Common features are the appearance of pain and distortion of facial expressions.