What is pulpitis? ↑
Pulpitis is an inflammation of the pulp - the soft tissue located inside the tooth that supplies it with blood and innervation.
The peculiarities of the course of this disease, which distinguishes it from inflammation of other organs, lie in the anatomical structure of the tooth - tissue consisting mainly of blood capillaries and sensitive nerve endings is placed in a strong, enclosed space.
The objective state of the pulp at different stages of inflammation is difficult to diagnose; the causes and forms of the disease are different. Each classification is based on 1–2 main (from the point of view of its author) qualities of pulpitis, such as: the cause of inflammation, the severity of the process or morphological changes.
Dividing into groups (classification) of various stages and forms of pulp inflammation allows you to more accurately characterize the state of changes in tissues, plan adequate treatment and anticipate further dynamics both in case of successful treatment and in case of possible complications.
Video: what is it
By etiology ↑
Knowing the cause of the disease, it is easier to understand the further stages of its development. Among the main causes of pulpitis, the following four are distinguished.
Infectious
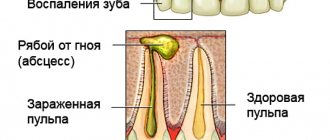
Photo: Infectious pulpitis
Infection is the main cause of most inflammation. As a rule, the infection penetrates to the pulp through the dentinal tubules from the carious defect.
Traumatic
Trauma means any mechanical damage to a tooth, either due to an impact (chip of hard tissue, crack or fracture) or during tooth treatment (accidental opening with a bur during the treatment of caries).
See photos before and after dental fluoridation. How is pulpitis treated? Find out in this article.
Retrograde
A type of infectious variant in which microbes appear in the dental cavity through the apical foramen - with the bloodstream or from an inflammatory focus in the periodontium.
Concrete
The cause of this inflammation of the pulp is the appearance of a hard formation, denticle or “dental pearl” inside the tooth cavity. They can be located both near the wall and directly in the thickness of the pulp.
Photo: Denticle
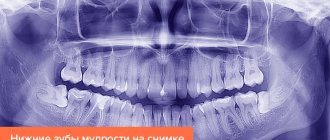
Denticles consist of an amorphous dentin-like substance. As a rule, the process of their formation is invisible to humans and they are found by chance during endodontic treatment of a tooth caused by other reasons, or on an x-ray.
But sometimes denticles can cause pulpitis, including in an intact tooth. A feature of the course of such inflammation will be alternating attacks that spontaneously arise and disappear.
With a long duration, there is a tendency to exacerbations in the spring and autumn periods.
However, we can consider the same classification from a slightly different angle:
- Physical impact:
- pulp burn (preparation during prosthetics or caries treatment);
- perforation of the tooth cavity during the treatment of caries;
- any injury accompanied by the chipping of a significant part of the tooth, especially accompanied by exposure of the pulp;
- denticles and petrificates;
- pathological abrasion of teeth.
- Chemical exposure (usually the consequences of complications of dental treatment):
- excessively long application of etching gel when filling with composite materials;
- insufficient leaching of acid gel;
- the use of antiseptics - too aggressive or with too high a concentration;
- toxic effect of filling material.
- Biological effects (infection):
- from a carious lesion;
- retrograde pulpitis - penetration of microbes through the apical foramen during periodontitis, osteomyelitis or sepsis.
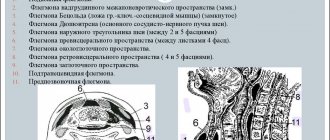
Etiology[edit | edit code]
Inflammation of the pulp is always caused by infection in the pulp chamber. This can occur in two ways: intradentally (through the crown of the tooth) and retrograde (through the apical (located at the top of the tooth) foramen). Most often, pulpitis is a complication of caries. Sometimes it can be the result of incorrect actions by a doctor (grinding a tooth for orthopedic constructions, low-quality filling materials, periodontal surgery, exposure to chemicals). Cases of retrograde pulpitis (that is, infection through the apical foramen of the tooth) have also been described.
There are three main groups of factors causing pulpitis:
- Physical factors:
- overheating of the pulp, for example, when preparing a tooth for a crown or preparing a carious cavity without cooling;
- opening the tooth cavity during preparation of a carious cavity;
- traumatic fracture of the tooth crown with opening of the pulp chamber;
- denticles and petrificates - are slowly deposited in the pulp tissues, can irritate its nerve endings, compress blood vessels, disrupt microcirculation, cause swelling, discomfort, which facilitates the occurrence of pulpitis from the action of other factors;
- pronounced pathological abrasion of teeth, in the presence of concomitant diseases (diabetes mellitus, osteoporosis) slow down the deposition of tertiary (compensatory) dentin, which leads to opening of the pulp chamber.
- Chemical factors are always iatrogenic (caused by the actions of the doctor):
- failure to maintain the exposure of the etching gel, which is necessary for the adhesion of most composite materials and some glass ionomer cements;
- poor quality (incomplete) rinsing of the etching gel;
- the use of strong antiseptics in the medicinal treatment of the formed cavity in the treatment of caries;
- toxic effect of filling material.
- Biological factors - direct infection into the pulp chamber:
- as a complication of the carious process (including recurrent caries developing under a filling);
- penetration of microbes from the carious cavity through the dentinal tubules after preparation, when taking an impression under pressure (a very rare way);
- retrograde pulpitis - entry of microbes through the apical foramen during osteomyelitis, sepsis, through the lateral branches of the root canal, after curettage of deep periodontal pockets.
Downstream ↑
This classification is schematic and tracks only the main differences between the fundamental different forms of pulp inflammation.
Spicy
Acute pulpitis is characterized by vivid manifestations - severe throbbing pain of a paroxysmal nature.
Photo: Acute purulent pulpitis
Initially, after a short painful attack, there is a long period of pain subsiding. As inflammation develops, the attacks intensify and lengthen, and the light intervals between them invariably shorten. the reaction to probing, as well as hot water, is sharply positive.
Chronic
Chronic pulpitis is characterized by a sluggish course. Spontaneous pain is not severe and is relatively rare.
Photo: Chronic pulpitis
Reactions to external irritation are also not as pronounced as in the acute form. The tooth is most often discolored, has a significant defect with an area of exposed pulp, and the root canal orifices may even be accessible for inspection.
Exacerbation of chronic
Exacerbation of chronic pulpitis has the same subjective manifestations as acute pulpitis; the differences consist in the continuity of pain and irradiation along the trigeminal nerve. But externally the affected tooth looks like chronic pulpitis.
Classification of pulpitis according to ICD-10 (WHO) ↑
WHO offers its own classification of pulpitis.
- K04 - diseases of the pulp and periapical tissues.
- K04.0 - pulpitis.
- K04.00 - initial, pulp hyperemia. According to MMSI - deep caries.
- K04.01 - spicy. According to MMSI - acute focal pulpitis.
- K04.02 - purulent, pulpal abscess. According to MMSI, acute diffuse.
- K04.03 - chronic. According to MMSI - chronic fibrous pulpitis.
- K04.04 - chronic ulcerative pulpitis. According to MMSI - chronic gangrenous pulpitis.
- K04.05 - pulp polyp. According to MMSI - chronic hyperplastic pulpitis.
- K04.08 - another specified pulpitis.
- K04.09 - unspecified pulpitis.
- K04.1 - pulp necrosis (pulp gangrene).
- K04.2 - pulp degeneration (dentals, pulp petrification).
- K04.3 - incorrect formation of TV. tissues in the pulp (secondary or irregular dentin).
One of the distinctive features of this classification is the separation into a separate category of changes in the dental pulp that occur even before the appearance of independent pain, at the stage of deep caries.
This requires the doctor to use additional measures to influence the pulp when filling large cavities, for example, applying medical-isolating pads.
Types (classification) of pulpitis
In 1989, the MMSI proposed the following classification of pulpitis:
1. Acute pulpitis:
- a) acute focal pulpitis;
- b) acute diffuse pulpitis.
2. Chronic pulpitis:
- a) chronic fibrous pulpitis;
- b) chronic hypertrophic (proliferative) pulpitis;
- c) chronic gangrenous pulpitis.
3. Exacerbation of chronic pulpitis.
In Russia, the transition to ICD-10 was carried out in all health authorities and institutions in 1999.
The diagnosis is indicated according to ICD-10. In brackets you can indicate the corresponding form of pulpitis according to MMSI.
According to Gofung ↑
The most popular classification among dentists, reflecting the stages of the disease, based on significant differences in clinical manifestations, as well as morphological changes in the pulp during the inflammatory process.
Acute pulpitis
.
- Partial . Changes in the pulp during acute partial inflammation are reversible. If you consult a dentist in the first hours after the onset of pain, it is quite possible to treat the tooth while preserving the nerve, the so-called biological or conservative method.
- General . In acute general inflammation, diffuse inflammation is observed, covering the entire pulp. Since it is impossible to reliably differentiate general pulpitis from the initial stages of purulent destruction based on clinical signs, many doctors already at this stage give preference to surgical methods of treating the disease.
- General purulent. Since at this stage of development of the pathology, disturbances in the structure of the pulp are extensive and irreversible, the main method of treatment is vital extirpation. The doctor's special attention should be directed to preventing the occurrence of periodontitis and influencing the post-apical tissues in order to relieve the primary manifestations of the periodontal reaction.
Chronic pulpitis
- Simple.
- Hypertrophic. The first two forms of chronic pulpitis are the most favorable for treatment. They allow the use of any surgical techniques, including preservation of the root sections of the pulp.
- Gangrenous. The most destructive form of chronic pulp inflammation, preference should be given to extirpative treatment. Since in this form the saturation of the walls of the root canals with pathogenic microflora is maximum, treatment is recommended to be carried out in several visits. This will allow for a long-term antiseptic effect, reducing the likelihood of post-filling complications.
Treatment methods for initial pulp hyperemia
Recent research is aimed at finding effective means for direct or indirect pulp coating, affecting microorganisms and pulp tissue in order to restore its morphofunctional state...
Initial pulp hyperemia (K04.00) is characterized by 3 zones, which are identified when examining a tooth section in a light microscope:
Zone of decay and demineralization.
In the first zone, remains of destroyed dentin and enamel with a large number of microorganisms are visible. The dentinal tubules are dilated and filled with bacteria. Dentinal processes of odontoblasts undergo fatty degeneration. Softening and destruction of dentin occurs more intensely along the enamel-dentin junction, which is clinically determined by the overhanging edges of the enamel, a small entrance hole into the carious cavity. Under the action of enzymes secreted by microorganisms, the organic matter of demineralized dentin is dissolved.
Zone of transparent and intact dentin
In the second zone, destruction of the dentinal processes of odontoblasts is observed, where a huge number of microorganisms and their decay products are located. Under the action of enzymes secreted by microorganisms, the organic matter of demineralized dentin is dissolved. Along the periphery of the carious cavity, dentinal tubules expand and become deformed. Deeper are the layers of compacted transparent dentin—a zone of hypermineralization, in which the dentinal tubules are significantly narrowed and gradually transform into a layer of intact (unchanged) dentin.
Zone of replacement dentin and changes in the pulp
In this zone, pronounced morphological changes take place in the nerve fibers and pulp vessels; the changes are similar to acute inflammation, up to the complete collapse of the axial cylinders of the nerve fibers. According to the focus of the carious lesion, a layer of replacement dentin is formed, which is distinguished by a less oriented arrangement of dentinal tubules. On this basis, some authors call it “irregular dentin”. Light microscopy also reveals disorientation and a decrease in the number of odontoblasts in the area corresponding to the lesion.
To carry out full treatment of initial pulpitis, active proliferation at the border of the filling material and tooth tissue is necessary. Namely, the formation of replacement dentin, this dentin was called secondary.
Many researchers have studied the dentin of the bottom of a carious cavity, for example, T. Fusayama in his works proved that carious dentin consists of two layers: the outer (infected and not subject to remineralization) and the inner (partially demineralized and softened, uninfected and capable of remineralization when exposed to microelements contained in the medicinal pad).
Currently, indirect pulp covering with therapeutic pads is used to treat initial pulp hyperemia.
- There is a known method of treating initial hyperemia using zinc-eugenol paste. The advantage of this method is the pronounced odontotropic effect of the paste (i.e., the ability to stimulate the formation of replacement dentin) and its antibacterial activity. The disadvantages of this method are that the use of this method requires several visits, eugenol can cause an allergic reaction from the pulp, has an unpleasant odor, in addition, zinc-eugenol pastes are not adapted to modern composite materials.
- For the treatment of initial hyperemia, a paste containing dimexide, etonium and aerosil was proposed, which in the early stages after treatment promotes reparative and regenerative processes in the dental pulp. The disadvantage of this method is that dimexide is a highly toxic drug.
- There is a treatment method using propolis paste, which contains 4% alcohol tincture of propolis, to which zinc oxide powder is added in a ratio of 1:3. The disadvantage of this method is the weak odontotropic effect of the paste, which cannot prevent the progression of the disease.
- But as therapeutic pads, preparations based on calcium hydroxide are still most often used - domestic (calmecin, calradent, calcesil) and foreign (daikal, life, septocalcin), which have pronounced odontotropic and remineralizing effects.
It is believed that their remineralizing effect is ensured by saturating the border zone with calcium and phosphorus ions; in addition, the high concentration of hydroxide ions provides a bactericidal effect.
Calcium hydroxide accelerates the processes of reparative dentinogenesis. The time period for complete normalization of the structural state of the pulp when using pastes based on calcium hydroxide exceeds 1 month.
However, therapeutic pads have a number of negative aspects:
- It has been clinically proven that the optimal pH level for a therapeutic pad should be neutral (7.0), and calcium-containing pads have a high pH level (8-11), which, on the one hand, ensures the bactericidal activity of the pad, and on the other, can cause a negative reaction with sides of the pulp - can lead to contact necrosis of the pulp, vacuolar degeneration, hyalinosis, as well as the formation of denticles and petrification, which leads to obliteration of the tooth cavity.
- A calcium-containing spacer placed at the bottom of a prepared carious cavity reduces the area of adhesion of the filling material to the dentin of the tooth, which impairs the fixation of the filling.
- Therapeutic lining based on calcium hydroxide can also blur the clinical picture, leading to asymptomatic pulp necrosis and further development of periodontitis.
Bonding systems do not have these disadvantages.
The use of the double bonding method for initial pulp hyperemia, when the thickness of the dentin between the pulp chamber and the bottom of the cavity is significant, the isolated use of universal adhesive systems of the latest generations is allowed, however, the exposure time of the conditioner on the dentin of the prepared cavity must be strictly observed, and the possibility of repeated bacterial contamination must be completely excluded, which achieved by complete removal of infected demineralized dentin.
The use of bonding systems implies double polymerization of the adhesive system after total etching, while the dentinal tubules are hermetically sealed with a hybrid layer, thereby creating a complete seal, preventing infection from entering the pulp and thus creating conditions for a compensatory reaction of the pulp.
Another advantage of bonding systems is that the use of bonds without a therapeutic pad simplifies and reduces the time of filling.
Adhesive systems ensure the formation of a strong chemical and mechanical bond between the filling material and hard tissues, but do not have a stimulating effect on the dental pulp.
However, some researchers believe that the use of one or several layers of adhesive is justified only in the treatment of superficial and medium caries, since even minor caries (for example, medium) is accompanied by round cell infiltration of the pulp, which can be morphologically classified as pulpitis. Only significant compensatory capabilities of the tooth make it possible to eliminate this undesirable reaction after filling. During initial hyperemia, the bulk of hard tissue in the area of local pulp damage is absent, which significantly reduces the possibility of a compensatory reaction.
A method has been proposed for the treatment of initial hyperemia with calcium-based drugs used for various diseases in the maxillofacial area associated with bone loss. In 1988, professors Georg Dietz and Peter Bartholomew proposed the bone-forming drug Osteoinductal for use.
This material is osteoinductive, that is, when treating initial hyperemia, it can be replaced by newly formed dentin as a therapeutic spacer. Its high antibacterial effectiveness has also been confirmed, but, in contrast to indirect coating of the pulp with therapeutic pads based on calcium hydroxide, due to the oil solution its alkaline pH value is reduced, which reduces the irritating effect of calcium, and, therefore, allows the drug to be used for the treatment of initial hyperemia.
There is also a method of pulp coating using MTA preparations due to its positive properties (good biocompatibility, antibacterial effect, moisture resistance, good sealing abilities).
There is a known method for treating initial hyperemia, where 2% chitosan ascorbate gel with a degree of deacetylation of 95% and a molecular weight of 100-120 kD and zinc oxide in a ratio of 1:2 are used as a therapeutic pad.
Chitosan is a biodegradable, non-toxic, biologically active drug, biocompatible, anti-inflammatory, antimicrobial, antitoxic, antioxidant drug.
Stopping the growth of pathogenic microflora is explained by the fact that chitosan is able to agglutinate microbial bodies. The mechanism of agglutination is similar to the gluing of erythrocytes by polycations. The mechanism of selective binding of chitosan to polysaccharide receptors on the cell membrane of a bacterial cell provides a bacteriostatic effect on almost any type of microbe. Chitosan causes binding of free microbial toxins. The antimicrobial effect of chitosan is enhanced by combining it with ascorbic acid and adding an additional hydrogen proton to the chitosan molecule. The use of a paste based on chitosan ascorbate in the treatment of initial pulp hyperemia provides an anti-inflammatory, bactericidal and odontotropic effect on the pulp, resulting in the deposition of replacement dentin at the bottom of the carious cavity, which isolates the dental pulp from the effects of microflora.
And yet, the severity of tissue changes in the pulp depends not only on the virulence of microorganisms and the action of toxins, but also on the state of reactivity of the pulp and the body as a whole. Therefore, success in the treatment of the inflammatory process in pulp tissues depends on factors such as the physiological characteristics of the pulp, the general condition of the body, the age of the patient, the development and localization of the carious process, the virulence of microorganisms of the carious cavity, the anatomical and topographical features of the tooth cavity and root canals.
Recently, there has been an obvious trend in the treatment of initial hyperemia without the use of therapeutic pads, which is associated with a number of their disadvantages, despite the fact that the use of calcium-containing agents in the treatment of initial hyperemia is more conducive to restoring the level of mineral metabolism and stimulating reparative processes in dental tissues in comparison with the isolated use of adhesive systems, which, unlike calcium-containing preparations, are aimed only at ensuring complete sealing, thereby providing the pulp tissue with the opportunity for a reparative function.
MMSI classification ↑
In fact, this is the same Gofung classification, to which exacerbation of chronic pulpitis is added in separate points, and the features of the inflammatory process in a previously treated tooth are also taken into account.
- Spicy:
- serous;
- focal purulent;
- diffuse purulent.
- Chronic:
- fibrous;
- gangrenous;
- hypertrophic.
- Exacerbation of chronic pulpitis:
- exacerbation of fibrous;
- exacerbation of gangrenous.
- Condition after partial or complete removal of the pulp.
During exacerbation of fibrous pulpitis, such extensive destruction does not occur as during exacerbation of gangrenous pulpitis. In the second case, the likelihood of periodontal complications is much higher.
The tooth is more likely to actively resist the sealing of the canals, exhibiting severe pain when a temporary filling is applied. This is explained by the dominance of anaerobic microflora, which feels comfortable when isolated from the external environment.
Often, removing part of the pulp (amputation) does not eliminate inflammation. This can happen either due to an incorrect diagnosis (error in assessing the real condition of the pulp), or due to a decrease in resistance or a violation of the treatment technology.
In these situations, complete extirpation of the pulp helps, and if it is impossible to pass through the root canals, repeated mummification of their contents, for example, using the resorcinol-formalin method.
Photo: Pulp removal (extirpation)
Treatment
Treatment of acute pulpitis is aimed at relieving inflammation of the pulp and, if possible, restoring its normal functioning. Analgesics are prescribed to relieve pain. In case of aseptic acute serous pulpitis in young people, it is possible to preserve pulp tissue using a conservative (biological) method. After mechanical and medicinal treatment of the carious cavity using non-irritating antiseptics, antibiotics, proteolytic enzymes, a therapeutic anti-inflammatory and regenerating paste is applied to its bottom with the placement of a temporary filling for 5-6 days, and subsequently - the final filling of the tooth in the absence of complaints from the patient. In some cases, it is possible to use physical procedures - laser therapy, fluctuarization, apex phoresis. Acute serous-purulent and purulent pulpitis lead to irreversible changes and loss of the functional ability of the pulp, which requires its removal: partial (amputation) or complete (extirpation), which is performed under local conduction or infiltration anesthesia (vital) or after the use of devitalizing agents (devital ). Vital amputation (pulpotomy) is aimed at preserving the viability of the root pulp and is indicated for acute focal pulpitis of multi-rooted teeth and accidental exposure of the pulp. The tooth cavity is opened, the coronal and ostial pulp is removed, dentin-stimulating paste is applied to the stump and the pulp chamber is sealed. Vital extirpation (pulpectomy) consists of thorough medical and instrumental treatment of the root canals with complete removal of necrotic pulp and restoration of the tooth with a filling. Devital pulp extirpation is carried out in case of acute diffuse pulpitis with preliminary application of a devitalizing paste containing arsenic or other compounds to the exposed pulp (in single-rooted teeth for 24 hours, in multi-rooted ones - for 48 hours) and placement of a temporary filling. Complete removal of the pulp, treatment of root canals with their filling and application of a permanent filling is carried out at the next visit. The results of endodontic treatment are controlled radiographically.
Classification of pulpitis in children according to Vinogradova ↑
Professor Vinogradova is a recognized leader in the field of pediatric dentistry. It clearly divides pulpitis of temporary and permanent teeth into separate groups.
This is dictated by differences in the course of these inflammatory processes, due to the specific structure and relative position of the teeth. In particular, the apices of the roots of temporary teeth may either not yet be formed or may already be missing in the process of their resorption.
The choice of treatment methods for primary teeth is also greatly influenced by the undesirability of complete endodontic root canal passage due to the risk of damage to the permanent tooth germ.
Acute forms
Acute pulpitis of temporary teeth:
- Acute serous. The peculiarity of the initial stages of pulp inflammation in a temporary tooth is that:
- due to the high permeability of dentin, significant changes in the pulp are observed already at the stage of average caries;
- focal forms almost immediately turn into diffuse ones, and therefore are not separated into a separate classification group.
- Acute purulent. Acute pulpitis in a temporary tooth also tends to quickly cover the entire pulp and earlier than in a permanent tooth it can become chronic, because:
- permeable dentinal tubules promote the release of exudate from the inflamed pulp, reducing the severity of inflammation;
- caries proceeds more actively and the pulp is exposed faster, allowing exudate to escape;
- wide apical openings allow exudate to escape, quickly involving periodontal tissue in inflammation.
- Acute pulpitis involving periodontal tissue or regional lymph nodes.
Acute pulpitis of permanent teeth:
- acute serous partial pulpitis (possible in teeth with a formed root);
- acute serous general pulpitis;
- acute purulent partial pulpitis;
- acute purulent general pulpitis.
With any acute inflammation of the pulp of a temporary tooth, there is a greater likelihood of inflammation spreading into the interroot space than with a similar process in a permanent tooth.
This is explained by the greater permeability of dentin, especially in the root junction area. In turn, this can lead to disturbances in the formation of the permanent tooth germ - changes in the timing of eruption and a decrease in resistance after eruption.
Find out how to treat stomatitis at home in a child. What to choose: fluoridation or silvering of baby teeth? Recommendations in this article.
Why did pain appear after treatment of pulpitis? The answer is here.
Chronic forms
Chronic inflammation of the pulp in temporary teeth can have several features:
- often occurs as a primary inflammation of the pulp, bypassing the acute phase;
- may be asymptomatic;
- quickly involves periodontal tissue in inflammation.
Chronic inflammatory processes are divided into a calm stage and an acute stage.
- Chronic temporary and permanent teeth:
- simple chronic pulpitis.
- chronic proliferative pulpitis.
- chronic proliferative hypertrophic pulpitis.
- chronic gangrenous pulpitis.
- Chronic aggravated temporary and permanent teeth. Most often, chronic simple pulpitis leads to exacerbation, which can occur without exposing the pulp. Other forms of chronic pulp inflammation worsen less frequently, since there is an opportunity for the outflow of the resulting exudate.
By origin
The next classification of pulpitis is by origin.
Infectious
Inflammation of the tuft inside the tooth, which develops as a result of contact with microorganisms and the destructive effect of the toxins they release. The classic variant of infection of the pulp with its further inflammation is the penetration of microbes deep into the carious cavity through the dentinal tubules, and less often the impact on the exposed nerve.
In most cases, pulpitis occurs as a result of infection of the pulp by bacteria. Retrograde infection is possible - in this case, pathogens enter the pulp through an opening at the apex of the root.
Hematogenous infection (through blood) is the least common, since the body’s defenses normally manage to block the irritant.
Traumatic
In this case, a fracture or dislocation of a tooth acts as a trigger for nerve problems. Over time, an infectious stimulus is triggered, and the process begins to progress. The fact is that normally the pulp should be closed - that is, be in sterile conditions.
If the chamber is opened, opportunistic bacteria from the oral cavity penetrate into the pulp chamber of the tooth and trigger an infectious inflammatory process. Injuries include any mechanical damage (bruises, falls, etc.) and tissue injury as a result of improper treatment.
Concrete
Concrete pulpitis is of a non-infectious nature and is a consequence of problems with metabolism in the neurovascular bundle when it is compressed for a long time by denticles or petrificates - formations inside the tubules that can compress the vessels, thereby disrupting blood microcirculation. Edema forms, which eventually turns into pulpitis. The intensity of irritation can be different - the degree of pain also depends on it.
Medicinal (“chemical”)
Modern classifications usually do not classify this type of pathology as a separate category, but in practice this type is common. A chemical burn of the pulp can develop as a result of the use of ether, alcohol or other potent substances to treat the chamber, non-compliance with the technique of using filling materials, or the introduction of aggressive treatment formulas into the periodontal pocket (they can penetrate through the apical foramen or root cement into the pulp).
According to Platonov
Platonov's classification has been used since 1968. It is not without its shortcomings, but it is quite understandable, simple and accurate, since it considers not only the pathological processes themselves, but also their course, the nature of the localization of pain. According to Platonov, pulpitis is:
- sharp;
- chronic;
- aggravated chronic.
He also identifies such forms as gangrenous, fibrous, hypertrophic (they indicate processes occurring in the pulp).
According to Vinogradova
Classification according to T. F. Vinogradova for 1987 refers to
extended, used to make diagnoses in children and adults. The scientist noted that pulpitis can occur in different ways, and identified three forms - acute serous, acute purulent, acute with the involvement of periodontal tissues and lymph nodes. Chronic pulpitis, according to the classifier under consideration, is divided into simple, proliferative, hypertrophic, gangrenous. This division is not universal, but is still actively used by dentists when treating patients.
According to WHO
WHO has its own classifier of pulpitis - it was developed in the 20th century and is called ICD-10. The system is considered the most complex and has a translation into “simple language”. Disease groups:
- K04.00 – initial pulpitis, hyperemia of deep caries;
- K04.01 – acute focal process;
- K04.02 – purulent, pulpal pulpitis.
Many doctors use the common code K04.0. This group includes 9 forms at once - from chronic acute to unspecified and specified.
According to Gofung
Classification by E.M. Gofung (1927) is based on the idea that the basis of the various clinical manifestations of pulpitis is a single process - inflammation from the serous stage of pulpitis to the purulent stage in the acute form, and to proliferation with necrosis in the chronic form. Gofung divided acute pulpitis into general, general purulent and partial, chronic - into simple, gangrenous, hypertrophic. Some forms of the scientist do not meet general medical requirements (for example, partial pulpitis), the chronic simple form does not indicate the condition of the pulp, and aggravated pulpitis is not included in the classifier.
Secondary lesions
Pulpitis can be not only primary, but also secondary – such lesions develop under crowns and fillings. Therefore, if a tooth hurts severely after cleaning the canals, then it clearly requires a thorough diagnosis.
Even the most thorough treatment of the canals does not provide a 100% guarantee that the cavity will be sterile, and the doctor may be in a hurry or simply not fully comply with the technology during work. Therefore, pain and an unpleasant odor are characteristic symptoms that should definitely alert you.
Pulpitis of wisdom tooth
Most adults have “eights”; they begin to erupt after the age of 20, sometimes this process turns out to be very painful and long. The presence of a tooth under the gum tissue does not guarantee protection against infections and destruction of enamel - a wisdom tooth can erupt in a patient with extensive carious cavities. In most cases, treatment of wisdom tooth pulpitis is useless, and the eights are simply removed.