The most common dental pathologies are caries and pulpitis. They can provoke serious and often irreversible consequences. When the first signs of a problem appear, you need to rush to the dentist to undergo a thorough examination. Diagnostics using modern equipment helps prevent various problems. Caries pulpitis is a completely different disease, although it has many similar symptoms. Often, caries ends with the process of inflammation of the pulp; it is therefore a harbinger of advanced pathology.
- The disease starts with the removal of all mineral components, and then the destruction of these compounds, first in the enamel, and then in the dentin. Carious lesions steadily penetrate first into the enamel, then into the dentin. The result is complete decomposition of tissues and the appearance of cavities in them.
Differences between pulpitis
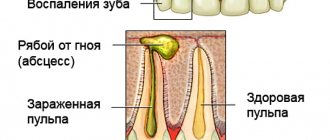
What fundamentally differs from caries is pulpitis – inflammation of the pulp. This term refers to the internal tissue that fills the canals of the tooth. It contains vessels with nerves and special connective tissue. All these components provide the nutrition required for hard tissues from the inside.
The disease develops after infection penetrates through the crown of a tooth or a hole that appears at the top of its root. Some biological factors can influence the problem:
- the development of a complication that provokes deep caries, since pulpitis is the result of an untreated primary disease,
- penetration of microbes from the caries cavity through the dentin tubules.
Physical provocateurs can also provoke pulpitis:
- overheating of the pulp due to tooth drilling,
- necrosis of pulp areas,
- crown fracture.
Additionally, chemical factors influence the occurrence of pulpitis:
- reaction to the anesthesia being performed,
- poor-quality treatment of dental tissues before filling the cavity,
- toxic effects of filling material.
Periodontitis
If a person “endures” pulpitis and does not see a doctor, and this, unfortunately, happens, then periodontitis . This disease is characterized by the complete death of the pulp and the spread of the pathological process into the tissues surrounding the tooth. A typical complaint during this period is pain when biting on a tooth. At the stage of pulpitis and periodontitis, the only possible help is endodontic treatment. It consists in removing the inflamed pulp (or its decay products) from the root canals. Root canals are thoroughly cleaned both mechanically and medicinally. After which they are hermetically filled with a filling material, most often gutta-percha. Taking painkillers without endodontic treatment is a symptomatic treatment that only causes harm. As a result of this approach, quite serious complications, such as osteomyelitis, can develop.
Distinctive symptoms
How can you reliably distinguish caries from pulpitis? The symptoms of these pathologies are similar, differing only in some parameters. The following parameters are similar:
- pain at the site of injury,
- reaction to the appearance of a stimulus: temperature, mechanical or chemical,
- the appearance of darkening on the enamel.
What is the fundamental difference between caries and pulpitis? These pathologies differ in the following parameters:
- Carious pain is mild and aching in nature. With pulpitis, this syndrome is acute, occurs in attacks, and significantly intensifies at night.
- With caries, if the provoking factor is eliminated, the syndrome goes away quickly. In a situation with pulpitis, when the nerve is inflamed, discomfort is felt for at least half an hour.
- Unpleasant carious sensations are localized at the site of enamel damage. When the pulp is affected, wandering pain syndrome occurs anywhere.
Among children, any disease progresses much more rapidly than in adults.
For children, pulpitis produces unpredictable symptoms and can become complicated, revealing signs of general poisoning.
Toothache
Let’s take a closer look at how to distinguish the condition of pulpitis from the problem of caries based on painful sensations. With the latter pathology, discomfort occurs only due to external influences. It is provoked by sweets, sour foods, air or water of different temperatures. When the problem penetrates deeply, when the cavity bottom is too thin, discomfort is noticeable during meals - it is caused by compression of the pulp at the time of chewing food.
But the main difference between caries, as opposed to pulpitis, is that in case of the first problem, it is enough to eliminate the cause of the irritation and the pain will immediately subside. But with pulpitis the matter is more serious. With such a disease, even eliminating the cause of the irritation does not relieve the pain - the tooth still aches for a long time. Moreover, the pain syndrome often starts spontaneously, even in the absence of external influence.
How else can we determine whether a patient has caries or pulpitis? You can understand the difference in pathologies if you analyze your nighttime well-being. Caries does not interfere with sleep, and when the diseased tooth has already entered the pulpitis phase, the patient often suffers from night pain.
Enamel color
Both pathologies are characterized by the appearance of characteristic pigmentation on the tooth surface, which, upon instrumental examination, reveals a certain softening of the enamel in this area. Often, already at the phase of superficial caries, all enamel layers are involved in this destructive process. Although usually the defect in caries is limited, it does not leave the boundaries of the enamel layer.
A carious lesion is distinguished by a brown or gray spot with a rough bottom. In a situation with chronic caries, pigmentation is noticeable, a certain compaction of the affected areas, their edges are smoothed.
How to determine the disease in the clinic
Only a dentist can accurately distinguish all the existing differences, who uses various diagnostic techniques for this. Caries can be detected even by visually examining the dentition with a dental mirror or various probes.
The dentist also uses ultraviolet light, laser or cold light to illuminate the diseased tooth. The staining method has proven itself to be excellent - this is how tissues are checked for the presence of carious lesions. Caries indicators are used, the most common of which are Caries Marker detectors or the Evicarie indicator.
To diagnose pulpitis, other research methods are needed. These include electroodontometry, which makes it possible to identify the threshold of sensitivity to an electrical impulse in the pulp. The principle of operation of this method is based on the fact that the nerve endings are irritated by a weak current. Thermometry is also recommended - this is the name for diagnostic measures in which they check how the tooth reacts to contact with water of varying degrees of cooling or heating. With pulpitis, the resulting pain persists for a long time, despite the elimination of the influence of this factor.
How to distinguish the two diseases?
Due to the fact that during caries the nerve of the tooth remains unharmed, its clinical picture is less severe than with pulpitis. The manifestation of certain signs of these diseases depends on the intensity of the pathology. In the chronic stage, the clinical picture is characterized by mild symptoms, which allows a person to postpone a visit to the dentist to a later date.
In the following table we consider the main differences in the symptoms of these two diseases.
| Signs of pathology | Caries | Pulpitis |
| Toothache | Painful sensations of aching or tingling nature in the affected tooth do not arise spontaneously. Pain occurs when eating sweets, sour, hard or sticky foods, brushing teeth or exposing the tooth to temperature irritants. In this case, the discomfort goes away immediately after stopping contact with the irritant. | It occurs regardless of the presence of any irritants and is pulsating or dull in nature. Lasts more than 10 minutes, radiating to the temple, jaw or ear area. Pain can only be relieved by taking a painkiller. In the chronic form of the pathology, pain in most cases occurs, as with caries, but with pulpitis it will torment the person for a long time |
| Enamel color | White spots first appear on its surface, which change color from yellow to dark brown as the disease progresses. | Dark grey |
| Cavity size | With superficial caries, a small defect is noticeable on the protective shell of the tooth, increasing as the pathology develops | Deep |
| Night pain | None | Often appear and cause insomnia |
| Body temperature | Doesn't rise | Depending on the type of pulpitis, it can reach 37.5, 38 degrees |
| In both cases, pathologies are characterized by the presence of an unpleasant odor from the mouth and inflammation of the gums | ||
With pulpitis, there is also an increase and pain in the regional lymph nodes, as well as swelling of the cheek in the area of the diseased tooth, especially after waking up.
The clinical picture of caries in comparison with pulpitis does not cause much discomfort in humans, but in the absence of the necessary treatment it will worsen, leading to the development of serious complications.
Treatment
Caries therapy
The procedure for treating not only caries, but also pulpitis is apparently quite simple, although this applies to the situation when the patient discovered the problem on time and immediately visited the dental clinic. The main steps in the treatment of caries: examination, then identification of lesion points, high-quality cleaning of the cavity, grinding of its walls, introduction of an antiseptic, after filling and final grinding of the filling. The detailed procedure diagram looks like this:
- First, the dentist examines the entire oral cavity to identify teeth damaged by caries.
- Next, using a drill, the dentist removes tissue that cannot be restored.
- The entire cavity, especially its walls, is thoroughly polished. This is necessary to ensure that any microscopic crack is closed.
- When the carious cavity is completely prepared, antiseptic agents are placed into it.
- Treatment with bactericidal medications is completed by inserting a gasket onto the surface of the bottom of the cavity.
- Then a filling is installed. Its material is a light polymer composition, a gypsum mixture with the addition of silver and fluorine.
- The final stage is grinding the hardened filling.
Pulpitis therapy
Therapy for pulpitis is more problematic.
The procedure is quite lengthy and has certain difficulties. The treatment mechanism requires high professionalism from the dentist, and the patient must scrupulously follow the rules of hygienic procedures for oral care. The treatment regimen looks like this:
- Performing an initial examination, the dentist identifies the area of pulp inflammation. At the same time, he checks for the presence of superficial caries.
- All affected, partially or completely destroyed tissues are carefully cleaned with a drill.
- Procedures are organized to ensure relief of the inflammatory process.
- Only after this the tooth cavity is filled, grinding the filling.
The most important stage in the treatment of pulpitis is the relief of inflammation. How competently this event is carried out directly affects the further condition of the patient. It is very important that the dentist completes all the required procedures, eliminates the affected areas, and thoroughly cleans the cavities. In addition, the patient must carefully monitor the condition of the oral cavity, always following the recommended hygiene measures.
Causes of caries development
The following reasons for the development of caries are identified:
- the presence of cariogenic microflora in the oral cavity;
- leftover food rich in carbohydrates;
- poor oral hygiene (soft plaque and tartar containing cariogenic flora);
- individual parameters of oral fluid, for example, saliva viscosity;
- genetic factor.
The mechanism of development of enamel demineralization (the release of calcium, fluorine, phosphorus ions from the enamel structure): cariogenic microorganisms (streptococcus sanguis, streptococcus mutans) are capable of fermenting carbohydrates to acids (in particular, lactic acid).
Further intake of carbohydrates leads to a local change in pH on the surface of the tooth enamel, reaching a critical level of 4.5 - 5.0. When a critical level of hydrogen ions is maintained for a long time, surface apatites dissolve in the least stable areas of the enamel (in the area of Retzius lines, interprismatic spaces), which leads to the penetration of acids into the subsurface layer of enamel and its demineralization. Less pronounced changes in the surface layer of enamel than in the deep layers are due to its structural features (the presence of a large amount of fluorapatites), as well as remineralization processes due to the constant supply of mineral components from the oral fluid. The continued formation of organic acids on the surface of the enamel leads to demineralization and a gradual increase in microspaces between the crystals of enamel prisms. As a result, conditions are created for the penetration of microorganisms into the formed microdefects.
What are the differences between deep caries and pulpitis?
There are certain differences between these pathologies that you need to be aware of. This is necessary in order to promptly differentiate these dental problems from each other, since their treatment requires a different approach. To understand the situation, we suggest considering a table indicating the characteristic manifestations of each of these pathologies:
| Deep caries | Pulpitis |
| Painful sensations are likely only after mechanical impact | Pain syndrome develops involuntarily, they can appear even in the absolute absence of any external factors |
| The pain goes away almost immediately after the influence of the irritant is eliminated | The pain syndrome has been bothering me for a long time |
| Deformation processes have not yet affected the pulp; only the enamel and dentin are affected | There are signs of pulp destruction |
Caries and pulpitis: differences and similarities
The most common diseases of the oral cavity are pulpitis and caries. Let's try to find the differences between these diseases.
During these pathologies, serious complications can occur that can lead to irreversible consequences.
Therefore, it is worth contacting a dentist at the first symptoms of these diseases; he will be able to conduct a thorough examination and perform the required treatment.
How to distinguish the two types of diseases
Attention! Many patients are interested in an important question - how to distinguish pulpitis and caries? What are the differences between these two types of pathologies? But one thing can be said with certainty: these two pathologies are very serious and dangerous. They can negatively affect the general well-being of the patient.
But it is still worth finding out the main distinguishing criteria of these two pathological processes:
- tooth damage. During caries, only the walls of the tooth are affected. At the initial stage, only a small spot appears on the surface of the enamel, which over time begins to slowly increase in size and darken. In this case, the nerve area remains unharmed, because dentin remains between it and the carious lesion. But be sure to consult a dentist when the first signs appear. With pulpitis, nerve endings are damaged. This pathological process is observed already at the third stage of caries; Caries is an infectious lesion of tooth tissues with their further destruction; if carious bacteria penetrate the tooth pulp, replenishing it, then caries develops into pulpitis.
- painful sensations. During a carious lesion, pain appears under external influence. Air, water, sweet and sour foods can act as irritants. If the disease has already entered the third form, then pain may occur when chewing food, because at this moment the pulp area is affected. In this case, when the irritating factor is eliminated, the unpleasant sensations disappear. Important! During pulpitis, pain is observed constantly. Even after tooth extraction, pain may continue for some time. With pulpitis, attacks of pain can occur independently without exposure to irritating factors;
- sleep problems. During a carious lesion, pain does not appear at night; this pathological process practically does not bother you. But with pulpitis, unpleasant sensations bother you even at night.
Symptoms
You can also distinguish between caries and pulpitis using some symptoms. The main signs of carious lesions and pulpitis are required. Caries is usually accompanied by the following symptoms:
- Manifestation of aching pain while eating hot and cold foods;
- There may be an unpleasant tingling sensation when drinking juices with high acidity, highly sweet carbonated drinks;
- With caries, discomfort may occur when chewing hard, crunchy food;
- When pressing on areas with darkening with special dental instruments, they are pressed, but the patient does not experience any unpleasant sensations.
Pulpitis is characterized by slightly different symptoms:
Inflammation of the lymph nodes in the neck is one of the negative signs of the development of pulpitis. An infection that affects a tooth spreads throughout the oral cavity and goes down through the body, leading to inflammation of the lymphatic system.
- If a person has acute pulpitis, then he may experience pain even without the presence of irritating factors. Unpleasant sensations may last for a long period;
- if there is pulpitis in a chronic form, then the patient may experience pain under the influence of chemical (temperature, acidity) and mechanical (chewing, pressure) factors. In this case, pain may continue after exposure for a quarter of an hour;
- With pulpitis, the patient often experiences enlarged lymph nodes. If pulpitis is not treated for a long time, the lymph nodes can become inflamed behind the ears and on the neck;
- the area of the cheek where the inflamed tooth with pulp is located becomes slightly inflamed. Swelling is severe in the morning;
- The person may have a slightly elevated temperature and may also have a headache.
How does a tooth hurt with pulpitis?
What kind of pain occurs if this problem bothers you? With this pathology, the patient experiences frequent pain, which complicates the patient’s life. Discomfort can also begin at night. The pain will be severe, sometimes even throbbing, and this is due to the fact that the most sensitive part of the tooth is damaged.
The initial stage is not accompanied by severe symptoms. There is a short-term pain that quickly passes. In acute pulpitis, there is constant pain of an acute nature. Discomfort appears due to exposure to any irritants. If you exclude the effect on the diseased area, then it gradually goes away. With constant intense irritation of the pulp, irreversible changes occur there.
During the acute form, pain sensations may occur such as: sharp, dull, pulsating, constant, localized or distributed, long-lasting and not so long-lasting. With purulent pulpitis, which is considered the main complication of acute pulpitis, there is a sharp unbearable pain, sometimes tearing, pulsating and gradually intensifying at night. It can radiate to the temple, ear or eye. Cold water can relieve the general condition.
With chronic pulpitis, painful attacks occur if any impact is applied to the diseased area. If you eliminate the irritant, the discomfort gradually disappears. At this stage, sudden pain, throbbing and dull, may appear. External stimuli will only worsen the condition. But it may not occur if the pulp is inaccessible to the irritant.
How long does a tooth hurt with pulpitis? The pain is constantly present and will even bother the patient for some time after the removal of the diseased tooth.
If no measures are taken, the inflammatory process will progress and lead to negative consequences and significant complications. Treatment will be carried out comprehensively, after a thorough examination of the oral cavity. If after the course the patient’s condition does not stabilize, the nerve is removed. Self-therapy should be completely excluded, as this can only further aggravate the situation and the general well-being of the patient.
Features of teeth in children
For a dentist, the characteristics of pain are the main diagnostic criterion; based on the child’s complaints, the doctor can suggest a certain diagnosis, be it caries, pulpitis or periodontitis. With other dental diseases, not only pain comes first.
The importance of pain as a diagnostic criterion can be explained by the unique structure of the oral cavity and teeth, especially when it comes to children.
Each tooth is covered with enamel - the strongest and at the same time the most fragile structure of the human body. The enamel does not have nerve endings, so when manipulating within its limits, no unpleasant, let alone painful, sensations arise. In children, the enamel is thinner and imperfect.
Under the enamel there is dentin - a strong base with a tubular structure, and these tubes are filled with liquid, which can act as an impulse transmitter. When dentin is exposed to temperature stimuli, for example, cold, heat, pain reactions are formed. Pain can also occur when exposed to chemical irritants, but such impulses can be transmitted by tubules that are located close to the pulp. The first painful area in the tooth is the so-called enamel-dentin boundary, the transition of enamel into dentin.
The most sensitive area of the teeth is the pulp, which is better known as the “nerve” of the tooth. Even close to the pulp, increased sensitivity appears, which is why even with deep caries pain appears when exposed to any irritant.
The dental pulp is a neurovascular bundle located in the tooth cavity. In children, this cavity is larger compared to adults, that is, there is less enamel and dentin.
Hemorrhoids kill the patient in 79% of cases
The pulp of the tooth fills not only the crown of the tooth, but also its roots, which extend into the internal tissues of the jaws. As the pathological process progresses from the crown to the pulp and to the root canals, the pain will only intensify, new characteristics will appear: intensity, duration, type, etc.