8) The nature of the arrangement of teeth
Spot stage:
On the surface of the enamel there is a dull, matte white chalky spot with clear boundaries. Sometimes it can turn yellowish or dark brown (depending on diet). Morphological changes occur in the tooth enamel. The process (with a white spot) is reversible; it is also possible to stop development (especially with a pigment spot) or transition to superficial caries.
◊ Focal dis- and demineralization of the surface layers of enamel.
◊ Expansion of interprismatic spaces (enamel permeability increases sharply, which creates even more favorable conditions for the penetration of microorganisms).
◊ The boundaries of the prisms are unclear (this is clearly visible under polarizing microscopy); some of them disintegrate in the form of amorphous detritus.
◊ Deep layers of enamel are intact.
Surface spot stage
. Characterized by an increase in demineralization and destruction of the enamel with the formation of a cavity in it. Enamel-dentin junction, dentin preserved. Progression of the process of enamel destruction. The outcome is remineralization (stabilization of the process), transition to middle caries.
◊ Demineralization and destruction, expansion and filling of the interprismatic substance with microflora.
◊ Displacement of enamel prisms, disruption of their ordering.
◊ Demineralization, destruction, random orientation of enamel prisms, detritus with microflora.
◊ In dentin - dead paths (thin stripes on the thin section), intratubular sclerosis (petrification) due to damage to the processes of odontoblasts.
● Stage of middle caries
(caries media). Macroscopically, a clear cone-shaped cavity is visible with destruction of the enamel-dentin junction and involvement of dentin. In the area of the cavity bottom, zones of softened, intact, transparent, reparative dentin are determined. The outcome is transition to deep caries, pulpitis.
◊ Zone of softened dentin (zone of decay and demineralization). Contains detritus (necrotic masses, microbes). Complete demineralization, dystrophic destruction of processes of odontoblasts, nerve fibers, collagen. Dentinal tubules are expanded and contain microflora.
◊ Zone of intact (unchanged) dentin. The structure is preserved, microbes are present in the dentinal tubules, and the organic contents are destroyed.
◊ Zone of transparent dentin. On the tooth section there is hypermineralization, compensatory peritubular (stenosis of the tubules, obliteration, atrophy of the processes of odontoblasts, nerve fibers) and intratubular (calcification of the periodontoblastic space, calcification of the processes of odontoblasts) sclerosis. This zone is absent in acute caries.
◊ Zone of reparative dentin (replacement, secondary, irregular). Dentin is uneven and poorly mineralized. Dentinal tubules are irregular or absent. Odontoblasts are fewer in number and disoriented. Parietal and intramural denticles are present.
● Deep caries
(caries profunda). A large cavity (cavern) is formed with clear, dense (with a slowly progressing course) or uneven, pliable (with rapid development) edges. The boundary between the cavity and the pulp may be disrupted (perforating caries). Microscopically, the layers of the bottom are determined: softened dentin, intact dentin and hypermineralized reparative dentin. The latter zones are usually unexpressed. The outcome is the development of complications: pulpitis, periapical periodontitis, odontogenic sepsis.
Clinical manifestations of deep caries
The clinical picture of deep caries is characterized by causal pain, mainly from temperature stimuli (more from cold). The boundaries of the absence of a pain reaction narrow: from 20-25° to 40-45° C. After removing the stimulus, the pain stops.
The cavities themselves in the cervical region are the most sensitive, since the dentin layer is thin, the entrance hole is wide, and irritants easily penetrate them. However, quite often hyperplastic gum grows into such cavities, which leads to the closure of the entrance to the cavity and “blurring” of the clinical picture.
In acute cases, a deep carious cavity on the chewing surface has undermined edges of the enamel, a lot of light softened dentin, the excavation of which is sharply painful. In a chronic course, the entrance hole to the carious cavity is wide open, at the bottom there is pigmented, slightly decalcified dentin. Painful sensations are not pronounced.
It should be noted that the clinical manifestations and diagnosis of deep caries are determined not by the absolute depth of the carious cavity from the surface of the tooth to its bottom, but by the distance from its bottom to the dental pulp, taking into account age-related deposits of secondary dentin and tertiary replacement. Therefore, the main criterion for making a diagnosis is the nature of the pain.
Causes
In the history of dentistry, about four hundred theories of the occurrence of caries are known. Among the recognized ones are chemical-parasitic, physical-chemical, trophic, but none of them fully explains the etiology of the disease. Today it is believed that pathology develops against the background of the interaction of a chain of internal and external factors. This happens when demineralization processes in enamel prevail over remineralization. It is believed that the development of caries is directly related to the microflora in the oral cavity, where streptococci live.
Origin of the disease
In order to understand the mechanism of the impact of pathology on a particular organism, one should consider the etiology and pathogenesis of caries, its classification and clinical picture.
From the introduction to the article, it became clear that caries can be classified as an individual disease, which completely depends on the human body, anatomical and genetic predisposition.
For example, it is a known fact that caries forms exclusively in places where nature provides an accumulation of microbial plaque and hard stone. For each person, due to the structure of the jaw and dentition, these places may differ.
Also, the lesion more often covers the chewing zone of the enamel - cariogenic microflora accumulates in the visible recesses created by flask fissures and the so-called “microbial plaque” appears.
Caries forms exclusively in places where nature provides an accumulation of microbial plaque and hard stone
Also, the anatomical structure of the dentition (narrow spaces between teeth) contributes to the accumulation of food, and this, as is known, is a direct source of carious bacteria.
As for the anatomical predisposition, one cannot fail to note the density, quality and health of the enamel itself, and the possibility of forming an organic coating (pellicle) on it. The stronger and more resistant the enamel is to mechanical, temperature and taste stimuli that cause microcracks, the lower the chance of putrefactive processes occurring in it.
Interestingly, even the salivary glands and the qualitative composition of the secretion, as well as eating habits (chewing on one side, biting on a certain side of the teeth, uneven distribution of load due to installed dentures or implants) directly affect the chance of caries.
In addition to anatomical predisposition, there are other individual factors that increase the chance of developing the disease.
- Geographical feature. Scientists have found that in each state the chance of developing caries will be very different. For example, residents of North America and Bulgaria are most at risk, but Nigerians have nothing to worry about (only 2% risk of the disease). CIS countries mainly occupy a middle position (50-99% risk). What in the geography of a country can influence the development of dental diseases? First of all, these are climatic conditions that form the mineral composition of the soil (plant and animal food, respectively) and, most importantly, water.
It is a known fact that the fluorine content in running water directly affects the possibility of the appearance of so-called “holes” - the higher the microelement content, the lower the risk.
Geographical feature is one of the factors that increases the chance of caries development - Choice of profession. Many people, when choosing a place of work, do not think about the possible specific health consequences. Working in enterprises, plants and factories where various alkaline and acidic compounds are regularly used, there are chemical wastes, etc., the patient risks not only the health of his teeth, but also the health of the entire body as a whole. By the way, even the profession of a pastry chef increases the chance of putrefactive processes on the teeth.
- Age . The etiology of caries cannot ignore the fact that up to 2-3 years of life a child is practically not at risk of developing caries, while in adolescence the chance is more than 60%. Interestingly, after 40 years, this figure decreases again.
It should be noted that in childhood and adolescence the development of pathology is influenced by additional factors:
- changes in the endocrine system and hormonal levels associated with puberty;
- possible disorders of the liver and gastrointestinal tract;
- low levels of fluoride and calcium in the body;
- concomitant diseases of the oral cavity, as well as systemic ones;
- changes in the qualitative composition of saliva and enamel;
- dental pathologies (malocclusion, installation of braces, etc.).
- Sexual characteristic. The scientific community has recognized that women suffer from dental diseases more often than men, which is quite logical. Pregnancy, lactation and other serious changes in the female body (menopause) primarily affect the condition of teeth, hair, nails and other aesthetic indicators.
It is also impossible to hide the fact that women are much more likely to consume confectionery products, which sharply increase the chance of putrefactive processes on the enamel.
Other causes of the disease include the following:
- unbalanced diet (predominance of sweet, sour and hard foods that destroy enamel);
- illiterate and irregular oral hygiene;
- metabolic disorder;
- lack of certain micro- and macroelements, minerals, vitamins in orgasm;
- genetic predisposition to caries;
- features of the formation of the dentition during the period of formation, eruption, change, etc.
Pathogenesis of caries: mechanism of disease development
Streptococci form colonies in the oral cavity - so-called dental plaques. This process goes through three stages:
- Formation of acellular organic film on the surface of the enamel - pellicles. The process takes up to several hours. The basis of the film is glycoproteins and other proteins in saliva.
- Collection of microorganisms and epithelial cells on the surface of the pellicle with subsequent growth of bacterial colonies. Continues for several days.
- Formation of mature dental plaque.
Dental plaque includes up to 70% microorganisms and has a mesh structure with semi-permeable properties. Carbohydrates easily penetrate into it and have a destructive effect on the tooth.
How does enamel destruction occur?
When eating carbohydrate foods, the microflora of the dental plaque instantly absorbs saccharides. This leads to a “metabolic explosion” and a sharp increase in acidity. After half an hour, the acidic environment is neutralized by saliva, but when carbohydrates are reintroduced, the pH level under the plaque decreases again, which leads to damage to the enamel due to increased permeability.
Against the background of the formation of organic acids on the enamel, demineralization increases, and the microspaces between the crystals of enamel prisms increase. This promotes more intensive penetration of microorganisms and their metabolic products into enamel microdefects. A cone-shaped lesion is formed, which spreads into the depths of the tooth. After some time, the surface layer of enamel dissolves - caries progresses and can lead to the removal of a baby tooth if no action is taken.
How does tooth resistance affect pathological processes?
Resistance is the ability of a tooth to withstand external influences. It depends on many factors:
- type of enamel hydroxyapatite, correctness of the protein matrix, degree of mineralization of the matrix, interaction of mineral phases and protein;
- the presence of defects in the enamel, the regularity of its structure, an electrical charge on the surface that prevents or promotes the adsorption of microorganisms;
- relief of the enamel surface, depth and shape of fissures, nature of the pellicle;
- type of structure of the skull, jaws, bite, proximity of teeth and the size of the spaces between them, etc.;
- functioning of the salivary glands;
- nutritional characteristics and somatic health.
The structure of enamel is formed at the genetic level and depends on mineralization processes.
Saliva
Saliva is the environment in which teeth are constantly present. Under favorable conditions, the processes of demineralization and remineralization occur harmoniously in it. If its composition is violated, a failure occurs. In combination with other cariogenic factors, changes in the composition of saliva provoke the formation of new lesions.
A change in the composition of saliva in an unfavorable direction occurs after taking sugar and easily digestible carbohydrates. To avoid this process, it is necessary to eliminate carbohydrates from the diet or get rid of dental plaque.
Other pathological causes contributing to the development of caries
The condition of the mother during pregnancy is of decisive importance for the health of the enamel. With toxicosis, carbohydrate metabolism disorders, gastrointestinal and thyroid diseases, chronic hypoxia, the mineralization of primary teeth in a child in the womb slows down.
Especially often, caries occurs immediately after teething in premature babies who are bottle-fed, as well as those who have suffered serious illnesses during the first year of life. The hardness of dental tissue depends on the state of the child’s digestive tract, the amount of fluoride in drinking water, and concomitant diseases during the first years of life.
Even the condition of the pulp affects the solubility of enamel. If the latter retains high functional activity, the enamel will remain hard. In turn, the condition of the pulp worsens after infectious diseases. In such children and adults, caries develops more often and more intensely, which is associated with a decrease in the immunological reactivity of the body.
Part 1. Treatment of dental caries using modern instruments and filling materials
Currently, there are prerequisites for revising some provisions of practical cariesology. This is due to the fact that, on the one hand, views on the etiology of caries have been formed, new filling materials with fundamentally different properties have appeared, and the provision of dental institutions with equipment, instruments, and medications has improved. On the other hand, the requirements for the quality of dental care provided to the population have increased. The widespread use of paid treatment has increased the dentist's responsibility for the quality of his work and created a material interest in improving his professional level.
At the same time, it should be noted that, unfortunately, the issues of preparation of carious cavities, properties and methods of using modern materials in most textbooks, manuals and manuals are absent or clearly insufficiently covered.
The monograph by A.Zh. Petrikas, “Operative and Restorative Dentistry,” published in 1994 and recently republished, is intended primarily for doctors with practical experience. Some of its sections are difficult to understand for students just beginning to study dentistry. In addition, its circulation quickly sold out, and this book is not available in the libraries of universities and medical institutions.
In the textbook “Therapeutic Dentistry” edited by prof. E.V. Borovsky (1997) paid more attention to the issues of etiology, pathogenesis, and clinical picture of various dental diseases. The issues of treating dental caries are considered schematically, from a general clinical point of view. Only 20 pages are devoted to modern filling materials and methods of their clinical use.
“Atlas of the phantom course of therapeutic dentistry” (Magid E.A., Mukhin N.A., Maslyuk E.E., 1997) is distinguished by good printing, clarity, and in-depth coverage of a number of issues of the phantom course (embryology, anatomy, dental histology, jaw system, equipment and equipment of the dental office). At the same time, it does not clearly cover some issues of tactics and techniques for preparing carious cavities; modern filling materials, adhesive systems, and the technique of their clinical use are incompletely described.
Of great theoretical and practical interest is the monograph by I.M. Makeeva, published in 1997, “Restoration of teeth with light-cured composite materials,” however, it is intended primarily for doctors with experience working with composites, and is intended rather to improve practical skills and deepen theoretical knowledge, and not for a student audience.
The issues of etiology, clinical picture and prevention of dental caries are covered quite fully and competently in the monograph by L.M. Lukin “Dental Caries” (1999), however, the issues of dental materials science, techniques for preparing and filling carious cavities are reflected in it, in our opinion, in insufficient detail.
Journal articles, although they contain useful information, cover only certain issues of cariesology. These publications are fragmentary in nature and, as a rule, describe the materials of one particular manufacturer.
In the first part of the book, the authors sought to highlight modern approaches to the preparation and filling of carious cavities. The main emphasis is placed on the properties and methods of using filling materials, both traditional and new ones that have just appeared on the Russian dental market. Some readers may have a question: “Why is little attention paid to the etiological aspects of caries?” The answer can be this: this book is a practical guide for doctors and dental students; treatment methods are presented precisely on the basis of modern understanding of the etiology and pathogenesis of dental caries; the latter are fairly fully reflected in articles, monographs and textbooks published not so long ago.
We are aware that many of our recommendations, especially those related to the technique of preparing carious cavities, will not immediately be clearly accepted by dental therapists, so we are ready for a constructive discussion, since we believe that our main goals coincide - to improve the quality of dental care , raise the prestige of a specialist - a dentist.
CHAPTER 1. DENTAL CARIES
Dental caries is a complex, slowly developing and slowly flowing pathological process in the hard tissues of the tooth, resulting from the combined effects of unfavorable external and internal, general and local factors, characterized at the beginning of its development by focal demineralization of the inorganic part of the enamel, the destruction of its organic matrix and ending, as a rule, destruction of hard dental tissues with the formation of a defect (cavity) in the enamel and dentin, and in the absence of treatment - inflammatory complications from the pulp and periodontium.
1.1. Etiology and pathogenesis of caries
The problem of the etiology of dental caries is, in principle, recognized as solved by most researchers. It is believed that the cause of caries is the microflora of the oral cavity. The microbial (infectious) theory has been comprehensively and repeatedly proven both experimentally and clinically. Other theories and concepts rather reflect the significance of certain links in the pathogenesis of this disease.
According to modern views, caries occurs as a result of the pathogenic effect of microbial “dental” plaque on tooth enamel. Without dwelling on the structure and metabolism of this dental formation, we will only note the most important point - when eating easily digestible carbohydrate food, it is fermented by the microflora of the “dental” plaque with the formation of organic acids. In this case, the concentration of acids on the surface of the enamel increases tens of times and becomes sufficient to dissolve its inorganic base - hydroxyapatite crystals. Subsequently, microorganisms destroy the organic enamel matrix.
In general, for the occurrence and development of caries, three conditions are necessary:
1) the presence of cariogenic microflora;
2) intake of easily digestible carbohydrates from food and retention on the surface of tooth enamel;
3) reduction of caries resistance (resistance to the effects of cariogenic factors).
It seems to us that it is in individual caries resistance that one should look for the answer to the question: “Why does dental plaque form in all people, but caries does not always develop in them?” Apparently, when caries occurs, a threshold effect occurs, at which the intensity of the cariogenic effect of the “dental” plaque exceeds caries resistance.
Caries resistance refers to the resistance of the body and dental tissues to the occurrence of dental caries. V.K. Leontiev (1994) cites a large number of factors influencing resistance to caries.
At the molecular level, the resistance of teeth to acidic influences depends on the type of enamel hydroxyapatite, inclusions of microelements in the composition of hydroxyapatite, the presence of vacancies in the crystal structure, the degree of enamel mineralization, the correct formation and laying of the protein matrix, and the interaction of the protein and mineral components of the enamel.
At the tissue level (tooth enamel), resistance depends on the regularity of the enamel structure, the presence and number of defects in it, the nature of the formation of enamel fibers and bundles, especially when they come to the surface, and the mosaic nature of the electrical charge of the enamel, which prevents or promotes the adsorption of microorganisms on its surface.
At the level of the tooth as an organ, resistance to caries is determined by the structure of the enamel surface, the formation of a pellicle on it (an acquired thin organic film that replaced the nasmite shell), its interaction with the tooth surface, the depth and shape of dental fissures.
Fissures are folds of enamel between the masticatory cusps. They may be more or less deep. Depending on this, “open” and “closed” fissures are distinguished. An extreme variant of a closed fissure is a flask-shaped one (Fig. 4).
In “closed” and especially in flask-shaped fissures, extremely favorable conditions are created for the formation and existence of microbial “dental” plaque. It is these areas of the teeth that are the “favorite” places for the development of carious lesions.
At the systemic level (dentofacial system), resistance to dental caries depends on the type of structure of the facial skeleton, jaws, bite and tightness of the teeth, the size of the interdental spaces.
At the organismal level, resistance to caries depends on the functioning of the salivary glands, the degree of rinsing and cleansing of the tooth surface with saliva, the influence of immunological and antimicrobial factors in it, and a number of psychological aspects (chewing laziness, life characteristics).
As E.V. Borovsky and V.K. Leontiev (1991) rightly point out, “... almost each of the above factors depends on the general condition of the body, its reactivity and resistance.”
At the group and population level, dental resistance to caries depends on the process of reduction of the human dental system, the adverse effects of individual factors of civilization (diet, cooking, introduction of carbohydrates).
It should be noted that a number of the listed factors create a genetic predisposition to dental caries (the degree of severity of reduction of the dental system, the structure of the jaws, teeth, bite, composition and structure of their tissues).
It should be remembered that the above factors of caries resistance act not only in childhood, but also in adults.
It seems to us that it is taking into account individual caries resistance that not only preventive measures should be taken, but also a plan for sanitation of the oral cavity should be drawn up, tactics for carious cavity preparation and filling materials should be chosen, the timing of control examinations should be determined, and a guarantee for the quality of treatment should be given.
1.2. Classification of caries
The most widespread and recognized among dentists are currently the classification of carious cavities according to their location (Black) and the classification of caries depending on the depth of the lesion.
According to Black, the following classes of cavities are distinguished:
Class I. Cavities located in the pits and fissures on the chewing surface of molars and premolars, the lingual surface of the upper incisors, and in the vestibular and lingual grooves of the molars associated with the chewing surface.
Class II. Cavities on the contact (proximal) surfaces of molars and premolars.
Class III. Cavities on the contact (proximal) surfaces of incisors and canines that do not require removal and restoration of the cutting edge.
Class IV. Cavities on the contact surfaces of incisors and canines that require restoration of the cutting edge.
Class V. Cavities in the cervical region of all groups of teeth.
Currently, American dentists identify another class of carious cavities.
Class VI. Cavities on the cutting edge of the front teeth and on the tops of the cusps of the lateral teeth.
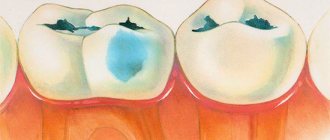
Topographic classification provides for four stages of caries (Fig. 5-8):
In our opinion, the classification that reflects the intensity of carious lesions (according to Nikiforuk, 1985) is also of practical interest, since it allows one to assess the severity of the lesion (“carious disease”) and outline an individual plan for treatment and preventive measures (Table 1).
Rice. 5-8. Caries in the spot stage. Superficial caries - focal demineralization, carious cavity of the enamel without the formation of a cavity within the enamel, Medium caries - carious, Deep caries - carious cavity within the enamel, cavity within the enamel and superficial layers of dentin and copulpar dentin
Table 1. Classification of caries according to the intensity of damage to the dental system (Nikiforuk, 1985)
| Severity of defeat | Affected teeth | Affected surfaces |
| Class I. Very weak caries | 17 | occlusal pits and fissures |
| Class II. Weak caries (ordinary caries) | 67 67 | occlusal fossae and fissures and occlusal |
| Class III. Average caries | 567 | occlusal and contact |
| 567 | ||
| Class IV. Severe caries (extensive caries) | 1234567 | proximal and occlusal and/or incidentally cervical 123567 |
| 4567 | ||
| 567 | ||
| Class V. Very severe caries (extremely common caries) | 1234567 | contact 1 2 3 and/or cervical 1234567 |
| 1234567 | ||
| 1234567 |
Stages of caries depending on etiology
Like any pathology, caries has several stages of development. The first is characterized by the appearance of small spots on the surface of the tooth; in the absence of treatment at this stage, caries enters the superficial stage, when the lesion affects the enamel. This is followed by moderate and deep degrees of illness.
Spot stage
The etiology of caries at the stain stage is the leaching of minerals, resulting in damage to the enamel. When contacting a dentist at this stage, caries treatment takes place quite quickly. But it is worth remembering that the onset of the carious process is difficult to notice due to the invisibility of the spots and the absence of pain, so experts recommend visiting the dentist 1-2 times a year as a preventive measure. To diagnose pathology at the initial stage of development, a specialist stains the surface of the teeth with a blue substance, which makes it possible to detect the resulting lesions.
Superficial stage
In the absence of treatment, as well as failure to comply with the rules of oral hygiene, the carious process progresses and enters the superficial stage. At this stage, irreversible processes of tooth decay on the surface begin.
Deep stage
If the disease is ignored at this stage, then superficial caries quickly turns into deep caries, characterized by damage to dentin. At this stage, patients complain of pain when eating cold or hot food. With deep caries, the damage reaches the nerve endings of the tooth, in which case the sensitivity of the teeth increases, severe discomfort and pain are felt. It is not uncommon for a patient to go to the dentist only for deep caries, when there is severe tooth decay and softening of the dentin.
Principles of treatment
Today there are two main approaches to caries treatment:
- without the use of boron (preparation);
- with preparation, when the affected tissues are drilled out.
The first approach is also called conservative therapy or invasive treatment. Its use is suitable for the treatment of initial forms of caries, as well as in the presence of a cavity.
The approach to treatment using the preparation method has several stages:
- First, the oral cavity must be prepared for the procedure. It may be necessary to remove plaque and tartar from the tooth and have all teeth professionally cleaned.
- Use of anesthesia if necessary. This is most often local anesthesia, but there are cases (panic fear of small children, multiple lesions of the teeth in the oral cavity, etc.) when general anesthesia is used.
- Then they move directly to preparation. Damaged tissue is removed from the cavity formed by caries and treated with special medications. In this way, it is possible to create conditions under which the growth of bacteria under the filling and its loss are prevented.
- Next, the cavity needs to be formed so that it can hold the filling well. Sometimes it needs to be given a special configuration so that the filling compound does not fall out. But most modern composites do not require such mechanical retention, since they are able to contact the tooth chemically.
- Insulation padding may be required. This is especially important when treating deep-stage caries. Thus, the nerve has an additional effect that protects against germs and inflammation. The gasket prevents the filling material from irritating the nerve.
- Application of a filling. First, the doctor selects its color, then isolates the diseased tooth from the rest of the oral cavity using cotton swabs or rubber dams, then applies the composite in layers. To do this, they often use such auxiliary tools as a matrix to create a gap between the filling and the adjacent dental organ, wedges that form an ideal contact point, and a retraction thread to correct the gums near the working area.
- At the final stage, processing is done. The filling is adjusted according to the bite to prevent tooth injury, pain and discomfort. They also do grinding and polishing so that there are no burrs left on the surface, plaque does not accumulate, and the filling has a natural shine.
Read also Emergency help for toothache
Preventive measures
Due to the individual characteristics of the body, the independent process of saturation and restoration of enamel and tissues is much stronger than the process of demineralization. The main cause of carious destruction is incorrect, poor-quality and untimely cleaning of the mouth and teeth, both by children and adults.
To avoid future dental problems, you need to learn how to properly brush your teeth without damaging your gums. During the procedure, the movements of the brushes should be smooth and circular, starting from the gums. A prerequisite is brushing your teeth in the morning and evening, this will remove food debris and prevent the proliferation of microbes in the oral cavity.
Modern methods of treatment
There are many new techniques for treating caries if the disease is not advanced. They seek to eliminate the causes of the disease, stop development and resist further damage.
The main advantage of new technologies is the removal of only affected tissues without affecting healthy ones. At the same time, treatment occurs without boron; instead, various methods of influencing the affected areas are used. The most common new techniques are: laser application, infiltration, air abrasion and ozone exposure. Using such methods, you can not only cure the disease, but also prevent it.
If the disease is already quite advanced and has entered a deep stage, high-quality treatment of the cavity using special preparation modes is simply necessary, as well as the installation of gaskets under the filling.
Dental treatment in Podolsk is very diverse. There are a large number of dental ailments, and in each case, treatment must be individual - proportionate to the situation, age, aesthetic requirements, etc. At the same time, dental treatment must be reliable - so that there is no worry and pain in the future; durable - so that all types of restorations last a long time and do not break; and of course, painless and comfortable. Dental treatment involves man-made recreation of the normal shape of teeth, their color, the density of contact with their fellow teeth, so that food debris and other axioms of dentistry do not get stuck between them.
If at the same time it is possible to preserve the dental nerve, then it is important to carry out manipulations that prevent the occurrence of secondary caries.
Such manipulations include:
- Careful preparation with a bur, taking into account the anomaly of the dental organ.
- When processing the bottom of the cavity, use tips with high speed and low speed alternately to eliminate the risk of opening the pulp chamber.
- The use of caries detectors, which help to recognize tissues affected by caries.
- Air-water cooling that protects the tooth from overheating.
- The use of therapeutic pads made of calcium hydroxide.
- Use of insulating gaskets.
- Treatment technique in several visits, during which the effect of medicinal drugs is monitored.
Treatment without boron
You can cure caries without using a drill using the following new developments:
- Remineralizing therapy is used when it is necessary to restore the crystal lattice of the enamel and fill it with minerals. It consists of a combination of local (treatment of the dental surface with special gels containing fluoride, calcium and phosphorus) and systemic (consumption of fluoridated salt, milk, tablets containing fluoride) measures.
- ICON technology is one of the most promising methods for treating primary caries in the spot stage. It is often used for patients who wore braces, and after they were removed, demineralized areas remained on the teeth. This is a kind of infiltration, when a special component, under the influence of a lamp emitting ultraviolet rays, helps the tooth surface acquire its original color. In this case, polymer-based liquid gets into damaged areas of the crystal lattice, and micropores become clogged.
- The ART technique is a non-invasive treatment method. In this case, instead of boron, excavators are used (tools used to scrape off infected tissue). After this, filling is carried out using glass ionomer cement. This technique is not particularly effective. Since it can be quite difficult to remove caries manually and there is a huge risk that cariogenic bacteria will still remain under the filling, which will subsequently lead to secondary caries.
Read also Endemic fluorosis - causes, symptoms, treatment, prevention
In addition, the first stages of tooth decay can be treated through ozone treatment, air abrasion and laser.
Sandwich technique
A good dentist knows that if you use several materials at once when filling, you can achieve the most reliable result. Often two or three materials are used at once, combining the positive aspects of each.
The sandwich technique is based on this approach. Its advantage is that it is possible to compensate for all the disadvantages of modern light fillings (they can become deformed and shrink, do not have an anti-caries effect, have insufficient biocompatibility) by adding glass ionomer cements to the filling. Composites and compomers, amalgams and composites are also often combined.
Glass ionomer cement liners can be applied in the following ways:
- lack of contact of the gasket with the edges of the cavity and oral fluid (closed sandwich);
- covering one wall with a gasket and having contact with the environment of the oral cavity (open sandwich).
Sandwich technology allows you to:
- Reduce the risk of secondary caries due to prolonged release of fluoride from the medical pad.
- Reduce shrinkage of the composite filling.
- Improve the color of the filling and bring it closer to natural.
- Suppress the proliferation of cariogenic bacteria.
- Treat cervical and subgingival defects, especially when dental root is affected by caries.
Ozone therapy
Treatment with ozone involves the use of its bactericidal properties.
This is a German development that is widely used in pediatric dentistry. In this case, they do not use boron or anesthesia, and often they do not even put a filling. This process occurs without pain, without noise and without injury. A special preparation converts oxygen into ozone, which is sent through the bowl to the damaged area. As the gas leaves the tooth, it is converted back into oxygen. As a result, in 20-40 seconds, ozone removes all bacteria that cause caries. Healthy tooth tissues do not change in any way, because due to their high stability, they can withstand ozone exposure and do not oxidize. Ozone does not cause allergic reactions.
At the final stage, remineralization is carried out using a special composition.
Ozone therapy is used in the treatment of caries in the spot stage in patients of any age. In the CIS countries, this method is not widespread due to the high price of the equipment.
Air abrasive method
This method involves mechanical treatment of areas affected by caries with special sandblasting devices, which are also used for professional cleaning of the oral cavity.
This is an American development, in which a kind of air flow containing impurities knocks out particles affected by caries. Initially, this admixture was quartz sand; now aluminum oxide, which is colorless and non-toxic, is used for this purpose. So, soft, affected tissues are removed, and healthy ones remain in their original position.
Secondary caries is practically excluded with this method. This process is painless, safe and does not require anesthesia. There is no noise or vibration, and the tooth does not heat up.
Read also Bleeding gums: causes and treatment
Air with impurities is supplied pulsed for 5-10 seconds.
The disadvantages of this method are that it can cause increased tooth sensitivity later, cannot be used in hard-to-reach areas where the tip cannot penetrate, and in rare cases may still require preparation and placement of a composite.
Infiltration
This method was invented in Germany and is a chemical-mechanical treatment without boron.
It can only be used to eliminate initial caries or those that have arisen on teeth after braces. A special gel is applied to the affected area, which can break down the affected parts of the enamel. Then it is dried with ethyl alcohol and a stream of air, and then treated with polymer resin.
The main advantages of this method are the absence of pain and the short duration of the procedure (15-20 minutes).
But infiltration can only be used on the smooth surface of the dental organs or between them. In addition, the affected area should have smooth edges and a wide entrance.
With a high-quality infiltration procedure, the patient can forget about caries for many years.
Laser treatment
The main advantage of laser treatment of caries is the absence of preparation. The tissues of carious areas are softer, so the laser can remove them and also disinfect them.
This method can be used for hypersensitive teeth, in childhood and for pregnant women.
The sterility of the procedure is explained by the absence of contact between the laser tip and the dental organ.
The cost of such treatment is quite high, because the equipment itself is expensive. Only highly qualified doctors wearing special protective equipment should work with such devices. If the laser damages soft tissue, the wound takes a long time to heal.
Etiology of caries
Currently, significant progress has been made in studying the etiology and pathogenesis of dental caries. The generally accepted mechanism for the occurrence of caries is the progressive demineralization of hard dental tissues under the influence of organic acids, the formation of which is associated with the activity of microorganisms. Soft plaque, dental plaque, replete with microorganisms, prevents the entry of essential macro- and microelements from oral fluid into the enamel, disrupts the balance between enamel and saliva, and thus slows down the restoration of tooth enamel.
Normally, in the oral cavity, the processes of re- and demineralization of enamel are in a state of equilibrium, and only in the presence of cariogenic factors is a shift in equilibrium towards demineralization observed. Poor oral hygiene, abundant plaque and tartar, inflammation and bleeding of the gums are clinically recognized as a cariogenic situation, which can lead to the occurrence of multiple carious spots, gingivitis and periodontitis. Practice has shown that the process of demineralization of enamel does not always end with the formation of caries; it is enough to eliminate the cariogenic situation and complete restoration of tooth enamel can be observed due to the active entry of mineral components into it from the oral cavity.
The oral cavity is an ecological niche in which a large number of different types of bacteria and viruses constantly grow in both practically healthy people and patients. Qualitative and quantitative characteristics of the bacterial landscape of the oral cavity show a state of dynamic equilibrium both between the various members of a given microbiocenosis and with a complex of local immunity factors. Most infections begin with the mucous membranes and include an obligatory stage - colonization of the epithelium, the key episode of which is the fixation (adhesion) of opportunistic and pathogenic bacteria. At the same time, representatives of the normal flora are either completely destroyed or their number sharply decreases, which once again convincingly confirms that the prevention of caries and periodontal diseases through teaching oral hygiene remains fundamental, since the role of dental plaque in the occurrence of caries is beyond doubt and has long been proven.
It is under the plaque that the pH of the environment changes in an acidic direction to a critical point (pH = 4.5), which causes the process of focal demineralization of the enamel. Poor oral hygiene, an abundance of soft plaque, humidity and thermostat temperature of the oral cavity, as well as a large amount of nutrients lead to increased activity of alkaline and acid phosphatase, acidification of the oral fluid due to waste products of microorganisms and their rapid reproduction.
It should be noted that the microbial landscape in the oral cavity changes dramatically, dental plaque and dental plaque negatively affect both the hard tissues of the tooth and the periodontium, therefore special attention should be paid to oral hygiene in early childhood and during the child’s growing up stages. Only optimization and intensification of oral hygiene will solve the problem of de- and remineralization of tooth enamel.
The incidence of dental caries is associated with the nature of the population's diet, the level of solar radiation, fluoride content in the environment, age, gender, and various climatic and geographical conditions. Significant risk factors for caries have been identified that create conditions for its development: pathological pregnancy, acute infectious and chronic systemic diseases, radioactive radiation and intensive x-ray therapy, hetero- and autosensitization of the body, anti-infective vaccinations and other influences affecting the immunological state of the body. To a large extent, the incidence of dental caries depends on oral care and its hygienic condition.
Complicated caries in children
In children and adolescents, complications, like the caries that precede them, develop at lightning speed. This is due to insufficient mineralization of enamel in childhood and the tendency of young patients to infectious diseases caused by streptococci - sore throat, bronchitis, measles and scarlet fever.
Advanced forms of caries in children lead to:
- the development of its circular shape, when, starting from the neck of the tooth, decay spreads around its crown, and over time the tooth breaks off;
- spread of infection along the surface of the crown (planar caries). In this case, the tooth completely darkens, the child complains of aching pain;
- acute and chronic pulpitis;
- infection of the rudiments of permanent teeth, resulting in multiple caries after their eruption.
Caries clinic
Stain stage (macula cariosa), or carious demineralization. Demineralization of enamel upon examination is manifested by a change in its normal color in a limited area and the appearance of matte, white, light brown, dark brown and even spots with a black tint.
Clinical observations show that a white carious spot (progressive demineralization) turns into superficial caries due to disruption of the integrity of the surface layer or into a pigmented spot due to a slowdown in the demineralization process. This is the process of stabilization. It should be understood that stabilization is temporary and sooner or later a tissue defect occurs at the site of the pigmented spot.
To determine the depth of damage to tooth tissue, the choice of method and the prognosis of the treatment, the size of the carious spot is important. The larger the area of the lesion (spot), the more intense the course of the pathological process and the sooner it will end with the formation of a visible lesion. If a brown carious spot occupies 1/3 or more of the proximal surface of the tooth, then, regardless of the data of the clinical examination (history, probing), damage to hard tissues of the type of average caries occurs under such a spot.
Caries in the white spot stage is asymptomatic and is detected only upon careful examination.
Caries in the pigmented spot stage is also asymptomatic.
A carious spot should be differentiated from a spot with hypoplasia and fluorosis. Hypoplasia is characterized by symmetry of damage to the teeth of the same name, which is due to the simultaneity of their formation, development and mineralization. With fluorosis, there are multiple, both white and brown, spots that do not have clear boundaries, located on the surfaces of all groups of teeth. With a high fluoride content in drinking water, the size of the spots increases, and the nature of the changes is more pronounced: the enamel of the entire tooth crown may have a brown color. Fluorosis is characterized by endemicity of the lesion - it manifests itself in all or most residents of any region.
Superficial caries (caries superficialis). It occurs at the site of a white or pigmented spot as a result of destructive changes in tooth enamel. Superficial caries is characterized by the occurrence of short-term pain, mainly from chemical irritants - sweet, salty, sour. It is also possible that short-term pain may occur from exposure to temperature stimuli. This is more often observed when the defect is localized at the neck of the tooth - in the area of the tooth with the thinnest layer of enamel. When examining a tooth, a shallow defect (cavity) is discovered at the affected area; it is determined by the presence of roughness when probing the tooth surface. Often, roughness is detected in the center of a large white or pigmented spot. Significant difficulties arise when diagnosing superficial damage in the area of natural fissures. In such cases, dynamic observation is allowed - repeated examinations after 3-6 months.
Superficial caries must be differentiated from hypoplasia, erosion of hard tissue and wedge-shaped defect.
With hypoplasia, the enamel surface is smooth, non-softened, defects are localized at different levels of symmetrical teeth, and not on the surfaces of tooth crowns characteristic of caries.
Erosion of hard dental tissues is cup-shaped, its bottom is smooth and shiny. Erosion is often accompanied by hyperesthesia - increased sensitivity to mechanical, chemical and temperature stimuli. The history often reveals frequent consumption of juices, fruits and sour foods.
A wedge-shaped defect is localized exclusively at the neck of the teeth, has dense walls and a characteristic defect shape. Usually asymptomatic.
Average caries (caries media). With this form of carious process, the integrity of the enamel-dentin junction is disrupted, but a fairly thick layer of unchanged dentin remains above the tooth cavity. With average caries, patients may not complain, but sometimes short-term pain may occur from exposure to mechanical, chemical and temperature irritants, which quickly passes after the irritants are eliminated. When examining the teeth, a shallow carious cavity is found, filled with pigmented and softened dentin, which is determined by probing. In the fissures of the chewing surface, the cavity is determined by probing. In an intact fissure, the probe usually does not linger, since there is no softened dentin, and in the presence of softened dentin, the probe lingers, which is a decisive diagnostic sign.
Preparation of a carious cavity is usually painless or slightly sensitive, but in some cases, especially when manipulating the area of its walls, it may be accompanied by pain.
Medium caries is differentiated from a wedge-shaped defect, erosion, deep caries and chronic periodontitis. Medium caries is distinguished from a wedge-shaped defect and erosion by the same characteristics as in the differentiated diagnosis of superficial caries. This form of lesion is differentiated from deep caries based on the patient’s complaints and objective examination data (see below).
The similarity between average caries and chronic periodontitis is the absence of pain in the presence of a carious cavity. The difference between these two diseases is that cavity preparation during caries is painful, and during periodontitis there is no reaction to preparation, since the pulp is necrotic. In accordance with this, the reaction to external irritations is also different: in the case of average caries, the tooth reacts to temperature and chemical influences, and with periodontitis, there is no reaction to these irritants. On the x-ray, during caries, the periodontal tissue is not changed, and in chronic periodontitis there are destructive changes in the bone fabrics.
Deep caries (caries profunda). With this form of the carious process, there are significant changes in the dentin, which also causes complaints. Patients indicate short-term pain from mechanical, chemical and temperature stimuli, which goes away after the stimulus is eliminated. Upon examination, a deep carious cavity filled with softened dentin is discovered. There are often overhanging edges of the enamel. Probing the bottom of a carious cavity is painless. In some cases, signs of pulpitis may appear: aching pain in the tooth after removing the irritant, a feeling of awkwardness in the tooth. As a rule, the process has a chronic course (long-term).
Deep caries is differentiated from medium caries, acute focal and chronic fibrous pulpitis.
Deep caries differs from average caries in more pronounced complaints (short-term pain from all types of stimuli: mechanical, chemical, temperature), which depends on the depth of the carious cavity.
Deep caries is distinguished from acute focal and chronic fibrous pulpitis by the paroxysmal and longer-lasting pain from external stimuli expressed during pulpitis, as well as by the presence of spontaneous pain, without the influence of external stimuli. If it is impossible to determine the condition of the pulp, then a temporary filling is applied to clarify the diagnosis. After preparing the carious cavity and thoroughly drying it, it is filled with dentin for 10-14 days. In this case, you should not use medications, especially painkillers. The absence of pain during this period confirms the diagnosis of deep caries, and the appearance of aching, paroxysmal pain when the tooth is isolated from external influences indicates inflammation of the pulp.