In the article we will look at what an ulcer of the skin and mucous membranes that develops in different organs looks like. The presented photos will help to recognize the onset of the disease in order to begin treatment procedures as soon as possible. You will learn the reasons for their occurrence on the body, the main symptoms by which they can be recognized, and how ulcers are treated.
First, let's find out how this type of tissue damage differs from simple wounds and erosions. An ulcer is a deep, inflamed, non-healing defect on the surface of the skin or mucous membrane, the healing of which occurs with scarring, as tissue particles are irretrievably lost.
Ulcers can be the result of an infectious disease, mechanical damage to the integument, or occur after chemical or radiation exposure. Ulcers from varicose veins or other disturbances in the blood supply to the organ, as well as the innervation of the site, are common. If the ulcer does not heal within one month, then we are talking about a trophic ulcer. Most often, you can see what a trophic ulcer looks like on the lower extremities (feet and legs) of people suffering from impaired venous outflow. Irreversible processes on the skin lead to the fact that the protective function of this place is greatly weakened and is unable to withstand external influences.
Next, we’ll take a closer look at what an ulcer looks like in different places on the human body, how to recognize it at an early stage based on common symptoms, and how to treat it.
Ulcer on the walls of the stomach
The main cause of stomach ulcers is considered to be exposure to Helicobacter pylori. This is a bacterium that enters the stomach with food and multiplies quickly, causing harm to the mucous membrane. The ability of protective mechanisms decreases, and the mucus secreted by the stomach is no longer able to cope with pepsin and hydrochloric acid. Aggressive factors destroy the mucous membrane, which leads to the occurrence of ulcers. Another reason for the appearance of ulcers in the stomach is considered to be nervous shock, constant stress, which causes spasms of the muscles and, naturally, the blood vessels of the gastrointestinal tract.
As a result of impaired blood flow in the stomach, stagnation occurs; the aggressive environment of gastric juice corrodes the walls, which leads to ulcers. The disease can also appear as a result of other diseases - tuberculosis or diabetes, liver cirrhosis or hepatitis, lung cancer or pancreatitis, etc. Injuries to the stomach of a mechanical or chemical nature can also lead to ulcers of the mucous membrane, as well as some medications.
Signs and symptoms of stomach ulcers
Here we will look at the symptoms of a stomach ulcer with a detailed description. The disease itself can also occur without symptoms. Thus, you may not be aware of the problem.
Pain syndrome
The first is pain syndrome. It can occur both before and after meals. If there is a sharp cutting pain, then it is a perforated ulcer
.
If there are constant nagging pains that are relieved by eating, then this is a cardiac ulcer.
or fundus of the stomach.
The nature of the pain depends on the location of the disease.
Note!
Localization in the upper part of the stomach is very rare. However, in this case, the ulcers are of an oncological or acute nature.
If it is located in the middle part of the stomach, then such patients experience pain immediately after eating food. Food that enters the stomach stimulates the production of gastric juice. In addition, food mechanically irritates the ulcer.
As a result, pain occurs.
If the ulcer is located in the distal part of the stomach, pain occurs 2 to 3 hours after eating.
People who have duodenal ulcers most often complain of being hungry ( against the background of hunger
) or night pain. In such patients, eating food causes a decrease in the pain response.
During an exacerbation, headaches appear, which stop approximately an hour after eating. But in any case, pain in the gastrointestinal tract should lead you to see a doctor for examination.
Dyspeptic disorders
Other symptoms of stomach ulcers can manifest themselves in the form of dyspeptic disorders. May have very black loose stools
with an admixture of various components. It is very foul and has a specific smell.
Carefully!
If there is an admixture of blood, then there is gastric bleeding. This is a bad sign! It often develops in people who drink a lot of alcohol.
The main clinical manifestations of peptic ulcer disease are sour belching
and
heartburn
. It occurs against the background of a general increase in the acidity of gastric contents.
In this case, gastric contents enter the distal part of the esophagus. As a result, a person may experience an unpleasant sour sensation in the mouth.
In addition, very often ulcer sufferers are bothered by nausea
and
vomiting
. Such symptoms are not of any malignant nature.
Asthenovegetative syndrome
Well, the third complex is asthenovegetative syndrome. In this case, the person is weakened
and eats poorly. His appetite is impaired and weight loss is observed.
If there is pallor of the skin ( for example, pale palm
), a frequent thread-like pulse, weakness, dizziness or fainting appear - these are also signs of a stomach ulcer.
The latter are painless. Especially if you are taking pills.
Diagnosis of the disease
The doctor is able to see what a stomach ulcer looks like by performing a fibroesophagogastroduodenoscopy on the patient. This is a study during which a small camera is lowered into the stomach through a special tube and the entire mucous membrane with all the flaws is visible on the monitor screen. At the same time, the contents of the stomach are taken for analysis, checking for the presence of Helicobacter. The doctor also prescribes blood, urine and stool tests to detect blood impurities. The patient must undergo an ultrasound of the gastrointestinal tract, as well as x-rays with contrast or monitoring the pH of gastric juice, checking it for aggressiveness of the environment.
The patient will not be able to see what a stomach ulcer looks like, but will understand its presence in the body by the symptoms. These are painful sensations in the stomach, heartburn after eating, burning, nausea, excessive gas formation with belching, a feeling of fullness even after a small portion of food. With the disease, appetite decreases, there is a feeling of heaviness in the stomach, there is a disturbance in stool (there may be both constipation and disorders).
What can happen without treatment?
Gastric ulcers in the later stages cause severe pathologies that pose a real threat to the patient’s health. Immediate surgery is often required. When a section of the organ walls is completely destroyed, a perforated stomach ulcer occurs and the symptoms are so severe that the patient has to immediately go to the hospital or call an ambulance.
Penetration
It occurs if the walls of the stomach are completely destroyed and the bottom of the ulcer is another organ, mainly the nearby pancreas. At the same time, gastric juice, flowing out, has a destructive destructive effect on it, which contributes to the development of acute pancreatitis. The main symptom of this condition is unbearable abdominal pain, which has a girdling character. Plus a fever develops.
See also: Symptoms and treatment of chronic bronchitis in adults
Perforation
This is the appearance of a hole in the wall of the stomach through which its contents penetrate into the abdominal cavity. The incidence of this ulcer outcome is about 8% of the total number of patients with this diagnosis. The symptoms correspond to the clinical picture of peritonitis: severe pain, weakness, signs of intoxication. Perforated ulcers can be diagnosed only with abdominal x-rays.
Malignancy
Cells damaged by an ulcer can degenerate and provoke the development of cancer - stomach cancer. Fortunately, this complication is rare, occurring in no more than 3% of patients. An interesting fact is that duodenal tissue with a peptic ulcer never degenerates into a malignant tumor. But things are less positive with the stomach.
Symptoms of malignancy are the classic signs of cancer: severe weight loss, loss of appetite, pale skin. Patients often begin to refuse to eat meat. Later they are joined by nausea and vomiting, fever, and severe exhaustion of the body. Metastasis may occur.
Pyloric stenosis
Constant scarring of the ulcer leads to a narrowing of the pylorus, the narrowest part of the stomach. Therefore, eating food causes unpleasant consequences: heaviness in the stomach, nausea, vomiting, belching. In the later stages of the disease, the patient may refuse food altogether, which leads to exhaustion and dehydration of his body.
Bleeding
Occurs when damage to blood vessels occurs in the area of the stomach wall affected by the ulcer. This is a fairly common complication, occurring in 15% of patients. Symptoms include bloody vomiting and black stools (“melena”), the color of which is due to the interaction of blood and stomach acid. Associated symptoms: pallor, dizziness, decreased blood pressure.
Perforation of a stomach ulcer and other complications require qualified medical care.
How to cure a stomach ulcer
Look carefully in the photo at what a stomach ulcer looks like. The mucous membrane can be damaged in one or several places. If the ulcer bleeds or has penetrated the entire wall of the stomach, then surgery is prescribed. If the ulcer is not perforated, then treatment consists of several stages.
- Antibacterial therapy. The doctor prescribes at least two antibiotics from the tetracycline or penicillin group.
- Medicines that are designed to increase the protective properties of the mucous membrane, for example, De-Nol, which forms a film on the walls of the stomach.
- Antisecretory agents not only coat the mucous membrane, but also neutralize the effects of aggressive hydrochloric acid. At the same time, heartburn, gas formation and pain are significantly reduced. It could be Maalox or Almagel.
- Proton pump blockers block the increased production of hydrochloric acid, which corrodes the stomach wall. This is "Omez" or "Omeprazole".
- Additionally, the doctor may prescribe probiotics (“Linex” or “Bifiform”), “Valerian” provides a calming effect after meals, “Motilium” will improve the motor functions of the digestive organs, and “No-shpa” will relieve tension and spasms.
Treatment lasts for quite a long period. At the same time, a strict diet is observed, excluding alcohol, coffee, broths, flour products, canned food, seasonings, smoked meats and fatty meats and fish; fried foods and vegetables that cause gas formation (beans, legumes, radishes and cabbage) are prohibited. Fruits and vegetables must be cooked. And citrus fruits should be completely excluded because of the acid, which will negatively affect the mucous membrane.
Diet for stomach and duodenal ulcers
To increase the effectiveness of drug treatment and consolidate a lasting positive result, a special diet is prescribed for stomach and duodenal ulcers:
- Eating in small portions, five to six times a day;
- Food is boiled or steamed: in particular, meat should be well boiled over low heat;
- The optimal food temperature is not higher than 65 and not lower than 15 degrees;
- Food should not overload the stomach either mechanically or chemically, be processed with minimal secretion of gastric juice, and therefore should have a liquid (semi-liquid) and crushed consistency;
- The dietary menu should be balanced and include products of both animal and plant origin;
- Compliance with the drinking regime (clean, raw water in large quantities);
- Alcohol and cigarettes are prohibited.
What can you eat if you have a stomach ulcer?
Patients with stomach ulcers need a specific diet plan. First of all, there are two main requirements for the diet: products should not irritate the gastric mucosa, but at the same time they should fully meet the body's needs. You should eat at least five times a day, but portions must be strictly dosed so as not to stretch the diseased organ.
It is important that the cooked food is not too cold or hot; food should not be fried. The main cooking method is steaming.
The patient is allowed to use:
- Slimy soups made from cereals, semolina, rice and oats;
- Lean meat (chicken, turkey or veal);
- Liquid mashed porridges;
- Eggs in the form of an omelet or soft-boiled;
- Kissels, compotes;
- Honey can be used as a dessert;
- Among dairy products, you should give preference to cottage cheese and cream, but with a low fat content.
What not to eat if you have a stomach ulcer: list of foods
Lard, salted fish, and sausage are not recommended even during remission. Lard is a difficult product for the stomach. Patients are wondering whether jellied meat is allowed for peptic ulcers. During an exacerbation, the dish is contraindicated. It is worth considering in detail what you should not eat if you have a stomach ulcer.
Below is a list of prohibited foods that are not recommended to eat if you have a stomach ulcer:
- Nuts and seeds have a mechanically irritating effect on the stomach wall and are strictly contraindicated for intestinal and stomach ulcers. Walnuts are strictly not recommended.
- Mushrooms are extremely difficult on the stomach and are not recommended for consumption even in remission.
- Spicy seasonings - garlic, ginger, pepper - are strictly contraindicated. Herbs are full of irritating properties and stimulate gastric juice. Tomato and nut sauce are contraindicated.
- The diet of an ulcer should not include raw vegetables with coarse fiber, which irritate the mucous membrane mechanically and chemically. During the acute period, do not eat tomatoes, garlic, turnips, onions, raw cabbage, or vinaigrette.
- Grapes are contraindicated for duodenal ulcers; they have a high content of sugar and active acids. It is not recommended to drink grape juice during an exacerbation of an ulcer. In the acute period, pomegranate is excluded, the fruit is sour, which will negatively affect the condition of the mucous membrane. During the remission stage, it is permissible to drink diluted pomegranate juice to restore hemoglobin. Cranberries are harmful for stomach ulcers, just like lemon.
- Fatty, heavy dishes such as dumplings, shish kebab, fried pork and lamb cutlets are strictly contraindicated for stomach ulcers; liver and lard are prohibited.
- In the acute period of an ulcer, you should not try dried fruits. Dried apricots or prunes are harmful and injure weakened mucous membranes. But during the period of remission, prunes with honey prevent constipation and restore body tone.
- If you have a stomach disease, avoid fatty foods, sausages, liver, caviar, and lard. Butter can be used in small doses to season soups or porridge.
It is important for the patient to adhere to a diet and not eat prohibited foods. Spending a long time in the fresh air, as well as spa treatment, will be beneficial. On the recommendation of a doctor, a long course of antisecretory drugs may be prescribed.
Ulcers in the duodenum
What does a duodenal ulcer look like? Exactly the same as the stomach. The symptoms of the disease are also similar, as are the causes of the disease. Treatment is carried out according to the recommendations of a gastroenterologist. It is necessary to follow a strict diet, as the following complications are possible:
- bleeding from the ulcer site;
- perforation, that is, the ulcer passes through the entire wall of the intestine;
- penetration, when the ulcer spreads to nearby organs;
- Pyloric stenosis, in which the opening between the stomach and intestines becomes narrow, preventing food from passing from one organ to another.
To avoid ulcers of both the stomach and duodenum, preventive measures must be observed. Lead a healthy lifestyle, eat right, avoid stressful situations, do not drink alcohol, do not smoke. Follow a daily routine, refuse tedious work, and do not go on the night shift. Be sure to follow a strict diet so that the ulcer does not develop into a chronic form.
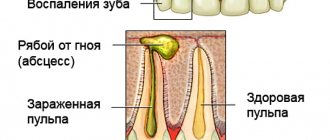
Ulcer with a white coating in the mouth
If ulcers appear on the mucous membrane of the mouth or gums, this may indicate not only the appearance of dental disease, but also many other infectious diseases, including syphilis and HIV. Many people have seen what mouth ulcers look like. In the photo below you can take a closer look at it.
Such ulcers have rounded outlines, inflamed borders and a white coating on the wound itself. Its presence in the mouth brings discomfort while eating, drinking, and talking. A person experiences pain, increased salivation, general weakness, loss of appetite and even an increase in body temperature, the causes of which are:
You can see what an ulcer looks like in the mirror. If such an ulcer cannot be cured at home, then you need to consult a specialist and identify the root cause of the disease. For treatment, medications are used based on the examination results. These may be antifungal or anti-inflammatory, antihistamine or antiviral medications. If a herpes virus is found, then antiherpes substances are prescribed. A complex of vitamins and minerals will also help. A good help in complex treatment will be folk methods - herbal decoctions: chamomile, sage or eucalyptus. Local anesthetics in the form of ointments and sprays will reduce pain. After treatment, you need the doctor to check what the ulcer looks like and whether there is any improvement in a positive direction.
Glossitis and methods of its treatment
Small ulcers under the tongue that become inflamed and a white coating are all signs of glossitis. This disease often occurs after diphtheria, scarlet fever or measles. In this case, complex treatment in combination with drugs against such infections is necessary . In fact, such wounds in the mouth are also a type of stomatitis.
The causes of the disease can be very different.
Therefore, treatment methods vary. In any case, it is advisable to always seek medical help without relying on self-medication.
If an ulcer appears under the tongue, what it is and how to treat it are the main questions that a person asks himself when encountering such a disease for the first time. In many cases, acute respiratory viral diseases or influenza give rise to the development of glossitis.
Therefore, in the fight against the disease, it is necessary not only to treat the affected areas of the oral cavity, but also to help the body cope with the infection faster and strengthen the immune system. Gastrointestinal problems can also show up on the tongue.
Therefore, it is always advisable to treat stomatitis taking into account an integrated approach: undergo an examination, if necessary, undergo tests
The source of infection in the tongue can be untreated caries, tartar, or periodontitis. In this case, the best prevention is to maintain oral hygiene and timely visits to the dentist.
Read also: Brown coating on the tongue
Sometimes a strange sore under the tongue is discovered after incorrect installation of an orthodontic structure, crown or bridge. An incorrectly performed dental prosthetic procedure can lead to injury to the gums or tongue.
By contacting a specialist, you can easily select the appropriate treatment method, taking into account all the characteristics of your body. Of course, a proper diet and the absence of bad habits will help reduce the risk of inflammation of the mucous membranes of the oral cavity.
Tumor-like formation on the tongue
Smoking and drinking alcohol contribute to the accumulation of heavy metal salts in the organs. This provokes irritation and opens the “gate” for infection.
Lack of vitamins and a decrease in the body's defenses sometimes contribute to the vulnerability of the mucous membranes of the oral cavity. Without paying attention to your health, a person may one day discover ulcers on or under the tongue.
Preventive actions
To minimize cases of stomatitis and other oral ulcers, you need to follow the rules of hygiene - use a high-quality toothbrush, monitor your oral health. Strengthening the body's immunity as a whole will help by eating fruits and vegetables. Nutrition should be balanced, containing all the vitamins and minerals the body needs.
Irrigators are considered an effective method of cleaning the oral cavity from food debris. Under strong pressure of water, you can open all the gaps between the teeth, preventing both stomatitis and periodontal disease of the gums.
Skin ulcers
The human epidermis has the ability to quickly recover from damage. But there are cases when rehabilitation processes slow down significantly or stop altogether. Places where necrotic tissue falls off and new ones do not grow turn into non-healing skin ulcers. How such a lesion looks and develops in stages can be seen in the figure below.
The tissues in such places do not recover for a long time, and ulcers on the skin cause a lot of inconvenience. Slow skin regeneration depends on the weakening of the human immune system and the presence of inflammatory processes. And the ulcers themselves become entry points for many bacteria. Infections quickly enter the circulatory system and spread throughout the body.
Why do ulcers appear under the tongue?
An ulcer under the tongue occurs due to an inflammatory process of an erosive nature. An abscess can be caused by various factors. It is very important to identify the cause that provoked the disease. After all, this is the only way the doctor will be able to prescribe effective treatment to the patient.
The most common causes of mouth ulcers include:
Leukoplakia under the tongue - the spot cannot be removed
Development of stomatitis
It can be of three types, namely candidal, aphthous and herpetic. The second option is more common. This stomatitis is chronic, so it cannot be completely cured. Therefore, from time to time the patient will experience a sore under the tongue and in other parts of the oral cavity.
Mechanical damage to the oral mucosa
This reason is often explained by the appearance of ulcers on the frenulum of the tongue in a child. He may get hurt on cutlery or scratched by candy. Simply biting your tongue is enough to create a wound on it.
Frenum injury - rupture
Just one microcrack can cause serious inflammation in the mouth. It develops into an abscess due to the active activity of bacteria. Within a few hours, the first symptoms of the disease will begin to appear in a child or adult. If you do not provide first aid to the patient, the infection will spread throughout the entire oral cavity.
Hematoma on the frenulum after trimming
Somatic disease
Often a white sore is one of the symptoms of a dangerous disease that affects the human immune system. These diseases include tuberculosis and HIV. Ulcers will begin to appear due to poor personal hygiene, as well as decreased immunity.
Read also: Blackness in the language of reason
Varicose veins under the tongue with inflammation
To find out why ulcers appeared under the tongue in an adult or child, you need to ask the patient about his health and find out if he was injured several hours before the onset of the inflammatory process.
Causes
- Various injuries associated with both mechanical damage to the integrity of the skin and electrical, thermal or radiation exposure.
- Ulcers on the skin can occur from tumors, for example, sarcoma or lymphogranulomatosis.
- In case of blood flow disorders, anemia, blood diseases, as well as scurvy or diabetes mellitus, side effects in the form of skin ulcers are possible. What ulcers on the legs look like can be seen in a patient with varicose veins.
- Infectious skin lesions.
- Progressive paralysis.
- Diseases associated with changes in the structure of the walls of blood vessels, for example, Raynaud's disease or syphilitic aortitis.
Treatment of external ulcers
Having examined what the ulcers look like in the photo, the patient can consult a doctor in time and begin treatment. First of all, a series of hygiene measures are carried out. The surface of the skin is cleaned of purulent secretions, and compositions or ointments that draw out the purulent contents are applied to the wound. Bandages need to be changed several times a day.
Traditional methods have a good effect on skin condition:
In combination with hygiene and cleansing procedures, you need to increase your immunity. For this purpose, vitamin preparations are prescribed.
If external treatment methods do not help get rid of the ulcer, then surgery is recommended. During the operation, dead skin is cut off and the deep defect is filled with a graft.
How to cure peptic ulcer
Treatment of patients is organized by a doctor. In the acute period, hospitalization may be required.
The following tasks are pursued:
- cleansing the body of Helicobacter pylori bacteria;
- prevention of complications;
- elimination of symptoms;
- providing conditions for rapid healing of the defect;
- decrease in acidity.
The male body often needs physical activity. With an ulcer, it should be minimal.
Even if the sick person is very athletic, rest should be maintained. Light gymnastics classes are possible.
There are three main aspects to successful treatment:
- taking prescribed medications;
- diet, including avoiding alcohol;
- lifestyle change.
Contraindications for stomach ulcers include avoiding alcohol and cigarettes. If there are no complications, surgery (resection) is not required. If you have a stomach ulcer, you should definitely take vitamins. They allow you to strengthen the body and speed up the healing process of the mucous membrane.
If the test results are positive for Helicobacter pylori, antibiotics are prescribed. The most active against these microbes are macrolides (Azitrox), penicillins (Amoxiclav) and nitroimidazoles (Metrogil).
To eliminate pain and heartburn against the background of increased acidity, antacids and proton pump blockers are used. The former normalize pH, and the latter inhibit the synthesis of hydrochloric acid.
Antacids include Gaviscon, Rennie, Phosphalugel and Almagel. The group of proton pump blockers includes Rabiet, Rabeprazole-OBL, Razo, Pariet, Hairabezol, Bereta, Noflux, Omez, Sanpraz, Nolpaza, Controloc, Epicur, Lancid, Lanzap and Peptazol.
During exacerbation, gastroprotectors are used. These include De-Nol and Venter. If a stomach ulcer is detected during pregnancy, then medications that are less toxic to the fetus are selected. The treatment regimen most often includes three or four drugs.
Ancillary medications include M-cholinergic receptor blockers. They suppress the synthesis of hydrochloric acid and pepsin. If there is a gastric ulcer, therapy includes the use of sedatives, antispasmodics, eubiotics, and prokinetics. These are symptomatic drugs.
Providing emergency care for stomach ulcers
You need to know not only whether a stomach ulcer is transmitted from a patient to healthy people, but also treatment methods if complications develop.
If you have symptoms of massive gastric bleeding, do the following:
- lay the patient down and elevate his legs;
- Avoid eating and drinking water;
- ensure complete peace;
- provide a basin in case of vomiting;
- place a heating pad or ice bag on your stomach;
- call an ambulance.
If a person needs to be lifted, a stretcher is used. This is a permitted way to move patients. After the ambulance arrives, drugs that are effective against bleeding are used (Dicinone, Aminocaproic acid). It is better to administer medications by injection. If necessary, Vikasol, Cryoprecipitate and plasma are used.
It is imperative to replenish blood loss. If complications develop, resection is required. During this procedure, part of the organ is removed. Resection is necessary for malignancy, perforation and gastric obstruction.
These are the three main indications for surgery. The entire stomach is not removed. Against the background of an ulcer, the peritoneum may become inflamed. In this case, laparotomy is performed. Aspiration is organized.
Other treatment methods
If there is a stomach ulcer, psychosomatics is of great interest to doctors. To reduce the frequency of exacerbations, you need to eliminate any stress.
Patients are advised to lead an active lifestyle. Folk remedies for this pathology are ineffective. You can drink some teas for stomach ulcers. It is recommended to use infusions and decoctions of flax seeds.
You need to know not only whether it is possible to play sports with a stomach ulcer, but also what the patients’ diet should be. Following a strict diet is the key to successful treatment.
The following are excluded from the diet of patients:
- spices;
- sauces;
- pickles;
- marinades;
- smoked meats;
- fried food;
- spicy dishes;
- canned food;
- mayonnaise;
- coffee;
- chocolate;
- cabbage;
- legumes
It is recommended to eat soups, cereals, vegetables, stews, lean meats, pasta, cereals, sweet fruits, steam omelettes, and fish. You can drink compotes, jelly, sweet fruit drinks, mousse.
There are three main aspects of the diet:
- refusal of prohibited products;
- adherence to diet;
- excluding alcohol.
During the remission phase, you can drink mineral water. If pregnancy and a stomach ulcer are detected, regular examination is required. With this pathology, it is very important to normalize weight. If you are obese, you need to think about how to lose weight. Not everyone knows whether people with stomach ulcers are accepted into the army. With frequent relapses, patients are released from service.
To prevent a person from needing resection in the future, all medical recommendations must be strictly followed. Self-medication is unacceptable. To normalize digestion, probiotics are included in the treatment regimen.
These include Linux. For nausea and vomiting, prokinetics are prescribed. With a stomach ulcer, a description of the main complaints to the patient is of great importance for subsequent treatment.
The prognosis for this pathology is most often favorable. Only an integrated approach to therapy can achieve healing. In case of complications, resection is required. If three or more exacerbations occur per year, then constant monitoring of the patient is necessary.
The most unfavorable prognosis occurs with malignancy. A very dangerous condition is when a stomach ulcer bursts. This complication poses a threat to human health.
What do ulcers look like with varicose veins?
Varicose veins are accompanied by destruction of the structure of blood vessels. As a result, the epidermis receives an insufficient amount of nutrients and oxygen. You can determine what leg ulcers look like by visually examining the limbs. If a constantly weeping wound appears, you should definitely consult a doctor, because varicose ulcers often develop into trophic ones. They can occur not only from varicose veins, but also from diabetes.
The skin in the affected area becomes burgundy, becomes inflamed, and begins to itch. You can see highly pigmented spots, bruises, and upon palpation you can feel lumps on the skin. These are all harbingers of the appearance of varicose ulcers.
If you have these signs and look at what the ulcer on your leg looks like in the photo, immediately rush to the doctor to start treatment on time, because these ulcers have a number of complications, such as damage not only to all layers of the skin, but also to muscle tissue, tendons and even bones .
Trophic ulcer: treatment and diagnosis
In addition to an external examination and examination of the patient’s complaints, general clinical tests are required. Also, to determine the depth of necrotic lesions, hardware types of diagnostics are used:
- USAS (angioscanning using ultrasound).
- Ultrasound of the lower extremities.
- Ultrasound Dopplerography - ultrasound and Dopplerography.
- Angiography with contrast.
- Intravascular ultrasonography (intravascular ultrasound).
Treatment is prescribed only after identifying the cause of the ulcer. This requires consultation with a surgeon, infectious disease specialist, therapist, phlebologist, and endocrinologist.
An advanced form of ulcerative lesion with purulent discharge and damage to the deep tissues of the dermis is subject to surgical treatment. Self-care at home for the affected area of skin is also important.
Pharmacotherapy and conservative treatment
Conservative therapy includes medications, anti-inflammatory and antibacterial ointments, physical therapy and elastic compression.
Venotonics, antispasmodics, and antibiotics are usually used (in the presence of a bacterial infection). Ointments and special wipes are used as local therapy, which accelerate tissue healing and prevent blood clotting disorders.
For varicose ulcers, elastic compression is required. It is carried out using compression hosiery selected by a doctor. With its help, it is possible to relieve swelling, improve blood circulation, and reduce pain. Non-elastic compression is also an option. These are special dressings impregnated with a medicinal composition - Una's dressing, zinc-gelatin dressing.
In the initial stages, physical therapy gives good results: ultraviolet radiation, laser therapy and vacuum therapy (VAC therapy).
Local wound care
Complete healing of an ulcerative wound is impossible without proper home care. To do this, you need to follow the following steps:
- Cleansing of necrotic tissue and rinsing with saline solution.
- Applying antibacterial ointment.
- Closure with a bandage.
You should choose a dressing material with your doctor. When healing an ulcer, a breathable material with a moisturizing composition is required. It protects the wound from drying out and reliably protects against bacteria and microorganisms.
For an infected wound, the bandage should be antibacterial. It absorbs secretions from the ulcer and helps reject pathogenic microorganisms.
Surgical methods
If conservative therapy does not help within 6 months, and the necrotic lesion worsens, surgical intervention is indicated. Surgery is also used for complications that threaten a person’s life (sepsis, gangrene).
The purpose of such treatment is to remove dead tissue, clean the wound and excise the focus of necrotic lesion. The following methods are widely used:
- Sclerosis of pathological veins.
- Phlebectomy.
- Open or endoscopic removal of affected veins.
- Skin transplantation for severe necrotic lesions.
For diabetic ulcers, the “virtual amputation” method is widely used. The surgeon performs a resection of the metatarsophalangeal joint and bone. At the same time, the integrity of the foot is preserved. This helps solve problems with excess blood pressure (excess weight) and eliminate the source of bone deformation.
Treatment of varicose ulcers
First of all, treatment begins with treating the ulcer site with antiseptics. This will slow down suppuration and bacterial growth. Treat wounds several times a day with Furacilin or Miromistin.
In order for the skin to regenerate faster, you need to use Lemicol. It will not only calm the inflammatory process on the skin, but also relieve irritation on the surface. This ointment effectively heals wounds.
Anti-inflammatory and bactericidal drugs and general-purpose vitamin complexes will help speed up recovery. It is important to strengthen the body’s immunity so that it actively participates in the fight against the harmful effects of microbes.
Venotonics are simply irreplaceable in the treatment of varicose veins. They promote vascular regeneration and prevent the formation of blood clots.
What does a trophic ulcer look like? Usually it is suppurating. Here the influence of Argosulfan is already necessary. This is a strong antibacterial drug that is used externally to combat ulcers.
Often ulcers with varicose veins constantly itch, causing an irresistible desire to scratch the sore limb. This can lead to harmful consequences. To reduce itching, you will need antihistamines such as Suprastin, Fenistil, etc.
Physiotherapeutic procedures such as laser or ultraviolet radiation are also used in treatment. During the session, the wound dries out and microorganisms die.
How to identify a trophic ulcer
Most trophic ulcers are associated with impaired blood flow. Most often they develop from venous ulcers and are localized either on the foot or on the lower parts of the leg. If a trophic ulcer appears on your leg (we will describe what the clinical picture looks like below), you should immediately consult a doctor for help, without leading to irreparable consequences or surgical intervention.
The process of formation of a trophic ulcer occurs gradually. The skin on the leg becomes purple and darkens, you can feel lumps and swelling. At the site of the future wound, the epithelium stretches and becomes shiny. Experts gave the process the name “lacquered leather.” Drops of lymphatic fluid appear on it. Even minor damage to the skin can lead to the formation of a wound.
Gradually its size increases in both width and depth. The process is accompanied by unbearable itching, painful sensations, and an increase in body temperature is often observed. An infection gets into the wound and suppuration begins. Sometimes the whole body suffers from a trophic ulcer, resulting in a general infection, which can cause fatal consequences for a person.
Treatment
You already know what a trophic ulcer looks like in the photo. Let's consider methods of treating this skin pathology. First of all, the cause of venous insufficiency is eliminated in the patient. It is necessary to stop high blood pressure and swelling at the site of the ulcer, as well as the pathological return of blood flow through the veins first.
Laser and radiofrequency thermoagulation are considered modern and quite effective ways to establish proper venous outflow and remove sclerotization of damaged vessels.
After this, the doctor examines what a trophic ulcer on the leg looks like (photo at the beginning of the article) and prescribes venotonics and medications that enhance skin regeneration in this area. If the ulcer has a diameter of more than 6 cm, then the skin is transplanted with material from the thigh or from the anterior wall of the abdomen. In some cases, a fasciotomy is performed. Cutting muscle tissue allows you to relieve pressure inside the tissue, thereby facilitating blood supply.
Anti-inflammatory medications and physical therapy will help. Treatment with polarized light will help relieve pain, reduce itching, and speed up recovery. After the acute condition has been eliminated, the patient will be recommended elastic bandaging of the limb or wearing compression garments. This will relieve stress and improve the overall condition of your legs. To better disperse blood through the vessels, the doctor will advise you to take daily walks and increase physical activity. If your legs are tired, you need to put them on a raised platform, for example, while lying on the sofa, raise them on a pillow.
Ointments for the treatment of trophic ulcers on the leg
Local therapy should be aimed at the original cause, eliminating complications and preventing relapse. In order to achieve maximum effect in a relatively short period of time, various ointments are used to treat trophic ulcers on the leg, which may contain several active ingredients.
Treatment of trophic disorders also depends on the stage of development of the defect:
- 1st stage. During this period, pain and difficulty moving come to the fore, local and general temperature increases. At this stage, it is best to use ointments and gels with antibacterial and cooling properties, for example Levomekol, Algofin, Levosin and Actovegin. Initially, they are treated with drugs in which the concentration of the active substance is small. If the disease progresses, the dosage should be increased.
- 2nd stage. The second stage is characterized by the presence of discharge from the ulcer and the appearance of purulent discharge. The smell and amount of pus depend on the characteristics of the microflora that got into the wound. The ulcer acquires round edges; in the center there may be a lesion without inflammation. For more successful treatment, ointments with antibiotics or substances that have a bactericidal and bacteriostatic effect are used. Before starting treatment, exudate samples should be taken for culture, followed by determination of sensitivity to antibiotics.
- 3rd stage. At this stage, trophic formations do not begin to actively granulate. To improve the prognosis, it is recommended to use Betadine, Methyluracil-D, Vundekhil, Thiotriazolin. Therapy is aimed at maintaining homeostasis in the wound and preventing the addition of new bacteria.
- 4th stage. The ulcer becomes smaller, the edges come closer together, and a scar appears. The fourth stage lasts until the connective tissue completely covers the defect. During this period, ointments are used to promote regeneration.
The following types of ointments exist:
- painkillers;
- wound healing;
- antibacterial;
- enzymatic;
- antihistamines;
- anti-scar;
- vascular strengthening;
- antifungal (for immunodeficiencies).
There are other ointments that can be used in the treatment of trophic disorders of the lower extremities; the selection of agents should be carried out by a doctor, purely individually, taking into account clinical and laboratory data.
Ointments for topical use
Gels and ointments for trophic ulcers of the lower extremities are used in almost all surgical hospitals and clinics. This proliferation has led to the appearance of a large number of ointments with different trade names, but the active ingredient rarely changes.
The most effective substances and their trade names:
- Levomekol: active ingredients methyluracil and chloramphenicol. The ointment has pronounced osmotic, bactericidal and cooling effects. Must be used once a day. Levomekol is applied to napkins, after which the wound is closed. The dressing and napkins should be changed at least once a day;
- Betadine, the active substance is povidone-iodine. This drug is excellent for treating wounds of the lower extremities. Betadine has a wide spectrum of antimicrobial action. Apply the ointment only after cleaning the wound from pus and necrotic tissue. The course of treatment should not exceed 14 days;
- Sulfargin is an ointment for trophic ulcers on the legs, based on silver. It has very pronounced antiseptic and regenerative properties. Gram-negative bacteria are most sensitive to the drug. Apply the drug once a day, after cleaning the wound.
They also use ointments that contain only an antibiotic, for example, Oflocaine ointment. Local application of the antibiotic is much better tolerated by the body and has a lethal effect on bacteria upon direct contact.
Anti-inflammatory ointments
The group of anti-inflammatory drugs includes not only substances that block the arachidonic acid and COX cascade, but also drugs that actively fight microorganisms inside trophic wounds. As a result of the cessation of tissue alteration by bacteria, swelling and pain in the pathological area are reduced.
Anti-inflammatory and analgesic ointments for trophic ulcers can be used only after consultation with a doctor and the absence of hypersensitivity to any of the components of the drug.
Names of ointments and method of their use:
- Levosin has an anti-inflammatory and analgesic effect. The product should be applied in a small layer 2 times a day. The duration of treatment is no more than three months;
- Liniment or Vishnevsky ointment. The main substance is birch tar, fat or castor oil. To use, apply a large amount of ointment to bandages or tampons, and then cover the wound with them;
- Metrogyl is an antiseptic and anti-inflammatory ointment. The product is applied 1-2 times a day. The duration of treatment should not exceed 10 weeks;
- Etonia is a good antiseptic and disinfectant. The course of treatment is up to 80 days. Use every 8 hours, applying a thin layer to the wound;
- Due to its composition, mephenate has an anti-inflammatory effect. The drug must be applied using a glass rod or a special spatula every 12 hours. Treatment should not exceed 14 days.
The effectiveness of any product must be carefully monitored. If there is no effect within 48 hours, the ointment against trophic ulcers should be replaced with another, more effective one.
Scarring and restorative ointments
Wound-healing ointments for trophic ulcers of the lower extremities promote the rapid growth of connective tissue with subsequent scar formation, and the task of such ointments is to enhance the vascularization of newly formed scars. Thanks to this effect, ulcers heal faster, and the likelihood of infection is reduced.
Solcoseryl ointment has a good wound healing effect. The drug is inexpensive and accessible. Solcoseryl consists of calf blood extract and has many positive reviews from patients and doctors. The spectrum of action is aimed at improving metabolic processes in the wound and capillaries. Apply every 8 hours, the course of treatment should not exceed two months.
If allergic reactions occur, the use of Solcoseryl should be suspended.
At the end of the 3rd stage and the beginning of the 4th, you can use Methyluracil ointment. The price ranges from 80 to 100 rubles. Due to its ability to reduce the amount of pro-inflammatory agents, the ointment has a beneficial effect on regenerative processes in the wound. Methyluracil combines well with ointment antibiotics and sulfonamides. To treat trophic lesions of the lower extremities, the wound should be smeared 1-2 times a day using approximately 8-10 grams of the drug. The treatment period is no more than 30 days. If rash or unusual symptoms occur, use should be discontinued.
Another representative of this group is zinc-gelatin ointment, or Voitenko paste. The medicine is prepared in a pharmacy. Gelatin ointment for the treatment of trophic ulcers on the legs should be used once every 24 hours, but not longer than two weeks. Storage should be in a cool room or refrigerator.
anthrax
This is a very dangerous infectious disease that is transmitted to humans from animals, both agricultural and wild. It is characterized by lightning-fast progression and hemorrhagic inflammation on the skin or internal organs; a carbuncle with purulent contents appears. Infection with anthrax can occur after contact with a sick animal, through fly flies or horsefly bites, or less commonly through soil or food. What anthrax looks like should be known to workers at farms and slaughterhouses, and to tanners at enterprises.
The clinical picture is characterized by acute manifestations - high fever, severe chills, enlarged lymph nodes. At the site of entry of the infection, a spot similar to an insect bite first forms. It hurts a lot, turns red-blue in color, and itches constantly. After a day, the spot turns into a papule, then into a vesicle with a diameter of several millimeters, which is filled first with serous and then with bloody fluid. When the inflated bubble bursts, an ulcer remains on the skin. Small vesicles appear on its external outlines, which expand the ulcer. This process lasts 2-3 weeks. A black scab (necrosis) forms in the center of the ulcer. Swelling and granulating ulcers appear. Fatty tissue under the skin is captured and the process ends with the rejection of the scab and the formation of a dense scar on the skin.
For treatment, in addition to penicillin antibiotics, anti-anthrax immunoglobulin is prescribed. Treatment should only take place in a hospital and under the strict supervision of a doctor. In order to prevent such a terrible infection, special measures are used on farms and large farms - animals are sanitized and vaccinated on time, and hygiene standards are observed. If contact with a sick animal does occur, you need to undergo preventive antibiotic therapy for 5 days.
The article examined in detail all types of ulcers; the photo shows how they look on the skin and on the mucous membrane of the stomach and oral cavity. Take care of yourself and don’t delay going to the doctor. After all, it is much easier to recover in the first days of the disease than from its advanced form.
Diagnostics
To confirm the diagnosis of gastric ulcer, the following research methods are required:
- Analysis for H. pylori . It is carried out in order to determine whether this bacterium is present or not. The test uses blood or stool samples, but a breath test is considered the most accurate. During this test, the patient drinks a liquid containing radioactive iodine. H. pylori breaks down this substance in the stomach. Then the patient exhales into a special bag and the resulting air sample is determined to contain radioactive carbon in carbon dioxide.
- Gastroscopy . During this procedure, the doctor inserts a thin tube equipped with a light bulb and a camera into the patient's mouth. By moving the tube further, the doctor assesses the condition of the gastric mucosa and the ulcer with his own eyes. If necessary, he may take a tissue sample from the edges of the ulcer (biopsy) and send it for histological examination.
- Radiography and fluoroscopy . Rarely carried out. The patient is asked to drink a barium suspension, after which a series of x-rays are taken, which will show the relief of the mucous membrane of the esophagus, stomach and duodenum.