Due to smoking, exposure to ultraviolet rays and other factors, sarcoma of the jaw develops. The pathology has several varieties and is accompanied by pain, enlarged lymph nodes, and facial asymmetry. At the first symptoms of the disease, you should consult a doctor who will make a diagnosis, perform surgery, prescribe chemotherapy, and recommend folk remedies. The prognosis depends on the timeliness of treatment.
Why does oncology develop?
Osteogenic sarcoma of the jaw is formed from connective tissue due to a mutation in a tumor suppressor gene. This gene ensures the prevention of carcinogenesis - the process in which a tumor arises and develops. Most often, sarcoma forms in the cortical layer - the most durable shell of the bone. The main causes of pathology are the following factors:
- bad habits;
- jaw injuries;
- professional activities related to radioactive radiation and contact with pesticides;
- bone growth (exostosis);
- benign bone formations.
Causes
There are no scientifically substantiated reasons that directly cause this malignant formation. According to some theories, its appearance is associated with the period of bone growth. Clinical studies have shown a relationship with the growth of the patient under study and pathology. Most patients with osteosarcoma had heights above average for their age group.
Possible factors contributing to the development of pathology:
- Traumatic injuries to the jaws.
- Radiation by ionizing radiation in close proximity to its sources (X-ray machines, nuclear reactors, radionuclides). It is impossible to determine the time of development of sarcoma after irradiation. This may happen years later.
- In rare cases, the appearance of osteogenic sarcoma is associated with Paget's disease. In the presence of benign formations of bone and cartilage tissue (endochondroma, osteochondroma), the likelihood of developing osteosarcoma increases.
- The presence of pathologies such as deforming osteosis, bone exostoses, fibrous degeneration can lead to their degeneration into osteogenic sarcoma.
What are dental skyces and why are they installed?
Read an interesting article. Effective treatment methods for mandibular ameloblastoma are described on this page.
What are the types of jaw tumors?
Doctors divide malignant formations of the jaw joint into the types shown in the table:
| Type of tumor | Peculiarities |
| Ameloblastic fibrosarcoma | Occurs due to the degeneration of benign fibroma structures into tumor formation |
| Characterized by rapid growth and aggressive course | |
| Accompanied by severe pain | |
| Chondrosarcoma | Formed from cartilage tissue |
| Spreads metastases through the bloodstream | |
| Ameloblastic odontosarcoma | Type of fibrosarcoma |
| Affects tooth structures - dentin and enamel | |
| Hemangioendothelioma | Formed from the endothelium of blood vessels |
| The neoplasm covers soft tissues and maxillofacial bones | |
| Ewing's sarcoma | Occurs most often in children during the period of bone growth |
| The etiology of the bone lesion has not been established |
Description of jaw cancer
Jaw cancer is a malignant neoplasm that affects the upper or lower jaws and mucous membranes.
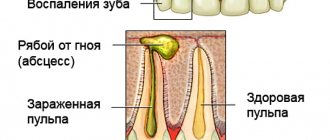
It is believed that men are more susceptible to the disease. Cancer of the lower jaw is more common than cancer of the upper jaw. The danger of the disease is that in the initial stages it is asymptomatic, and many patients seek qualified medical help too late, when the cancer has become advanced. The photo shows an image of the lower jaw, which is affected by sarcoma. Initially, the symptoms of the disease do not cause any concern in the person; outwardly, he looks quite healthy, despite the onset of development of the craniofacial neoplasm. As the pathology progresses, there is an increased division of cancer cells of the connective tissue of the periosteum, cortical bone and bone marrow, against which the tumor grows significantly. Painful sensations occur periodically and can be relieved with analgesic drugs.
Primary symptoms are similar to those of a cold and chronic fatigue. A person can be unsuccessfully treated for sinusitis, inflammation of the gums, and swelling of the upper eyelids for a long time, trying to relieve them with the help of folk remedies and medications. As a result, diagnosis and treatment of jaw sarcoma is carried out too late, when the chances of a favorable outcome are significantly reduced.
The disease is more common in children and young people under 40 years of age.
ICD-10 code: C41.0 Malignant neoplasm of the bones of the skull and face and C41.1 Malignant lesion of the lower jaw.
Symptoms: how to recognize the disease?
The primary signs of the development of an oncological process are similar to other diseases, for example, sinusitis.
Sarcoma of the upper jaw in the early stages of development resembles other pathologies - sinusitis, gumboil, polypous formations. The disease manifests itself in a number of signs not only from the jaw joint, but also from other parts of the face - nose, eyes, nerves. The main symptoms are shown in the table:
| Facial department | Symptoms |
| Jaw | Unilateral enlargement of the jaw joint |
| Facial asymmetry | |
| Limited mobility | |
| Deformation | |
| Formation of purulent ulcers on the gums | |
| Displacement of the structures of the mouth and throat | |
| Pain of a pulling or shooting nature, not strictly localized | |
| Frequent spontaneous fractures | |
| Chewing and swallowing dysfunction | |
| Eyes | Protrusion of eyeballs |
| Double vision | |
| Deterioration of vision | |
| Increased tear production | |
| Swelling of the eyelids | |
| Nose | Loss of smell function |
| Feeling of stuffiness on one side | |
| The appearance of purulent discharge mixed with blood | |
| Nasal breathing disorder | |
| Deviation of the nose due to an increase in the size of the tumor | |
| Nerves | Facial and headache |
| Feeling of numbness in the jaw |
Symptoms of uterine sarcomas
The main problem in the treatment of sarcomas is, first of all, their late diagnosis. Patients in the post-Soviet space are often very inattentive to themselves: they do not attach importance to pain and intermenstrual bleeding, and may not appear at the gynecologist for years. The result is the detection of a tumor in the final stages, when even the most progressive therapy in the most prestigious clinic in the world may be unsuccessful.
The main insidiousness of sarcomas is the almost complete absence of symptoms in the early stages, as well as their similarity to some other less serious diseases of the female genital area. If you regularly visit a gynecologist, there is a chance that the specialist may be alerted by changes that do not bother the patient, and he will conduct the necessary examination.
What to do to detect sarcoma at an early stage.
The first stage begins with a few tumor cells that do not interfere with the function of the uterus, so there are no signs. It can be discovered accidentally in the event of a diagnostic curettage of the uterine cavity for another pathology. As a rule, a tumor is an incidental finding.
Subsequent stages of development can already cause changes in the body and disrupt the function of the organ.
The most characteristic symptom indicating a tumor process is uterine bleeding (metrorrhagia). It was noted by the majority of patients – 60%. Vessels are damaged for several reasons. As the sarcoma grows, it grows into blood vessels, damaging their walls, causing blood to leak out of the bloodstream. Massive bleeding is also observed when the tumor disintegrates in the final stages. Metrorrhagia does not always indicate sarcoma. They can also be caused by fibroids - a benign tumor or cancer. Bleeding may be so profuse that immediate hospitalization at the gynecology department may be required.
40% of women with uterine sarcoma complain of pain in the lower abdomen. They have a cramping, aching character. Pain is also a nonspecific indicator. It is often overlooked. Very often, sarcoma is combined with fibroids, so pain is sometimes attributed to growing fibroids. The occurrence of pain is associated with the growth of the tumor in size and compression of the nerve endings. The growth can stimulate uterine contractions, which can also be painful.
12% of patients noted the presence of vaginal discharge (leucorrhoea). Leucorrhoea is a discharge from the vagina, the color may vary, there may be blood impurities, the smell may be absent or appear in the last stages. This symptom also cannot be classified as nonspecific, since odorless and colorless discharge may be a variant of the norm. Leucorrhoea is often accompanied by infectious inflammatory diseases of the genital organs or sexually transmitted diseases.
Also, patients sometimes note an enlarged abdomen and a feeling of fullness in the uterus. The abdomen may enlarge as the tumor grows, especially if it is located on the front wall of the organ.
In addition to the above symptoms, one should be very wary of the appearance of such signs as long-lasting low-grade fever, weakness, exhaustion, loss of appetite, and sudden weight loss. These signs indicate the presence of a malignant neoplasm. It could be sarcoma or cancer.
Since the symptoms for the most part are not directly related to sarcomas and can accompany many other diseases of the genitourinary system, a woman is often initially suspected of having an infection. And only after the inflammatory infectious process is not confirmed, the search for oncological pathology begins. The result is wasted time. Treatment of uterine sarcoma abroad remains the last option to avoid unnecessary time and material costs.
How is diagnosis carried out?
Diagnosis of pathology is carried out using a number of procedures, including rhinoscopy.
Sarcoma of the jaw is determined by an oncologist. It is also recommended to consult an ophthalmologist and otolaryngologist. The doctor studies the medical history, conducts an examination, identifying external signs, palpates the tumor itself, establishing its size and consistency, and the surrounding lymph nodes to establish a diagnosis. Diagnostic methods are prescribed, such as:
- rhinoscopy;
- fiberoscopy;
- biopsy;
- radiography;
- scintigraphy;
- computed tomography or magnetic resonance imaging;
- Ultrasound of the eye orbit;
- blood test for tumor markers.
Features of the pathology
Sarcoma of the jaw bones is a tumor that forms during the process of increased division of malignant bone tissue cells. The disease can be diagnosed at any age. It is noted that it most affects young organisms 10-20 years old, when active growth occurs. The peak incidence occurs during puberty. Males get sick 2 times more often than women.
The percentage of metastasis in this pathology is small, unlike many other malignant tumors. Feature - the tumor is characterized by rapid growth. Already in the first stages, the patient may experience severe pain in the area where the formation is located. Sarcoma is prone to repeated relapses and is resistant to most methods of radiation and chemotherapy. Therefore, it often has a poor prognosis.
If osteogenic sarcoma is complicated by infection, this can lead to serious complications (blood poisoning, sepsis, death).
Treatment: which methods are effective?
Surgical intervention
Osteosarcoma of the jaw is eliminated radically by excision, including surrounding healthy tissue. Organ-preserving operations are practiced, which allow partially preserving the jaw and restoring its functionality. Then a metal-plastic implant or a donor bone site is introduced. If metastases occur, the affected lymph nodes are removed.
Chemotherapy
Chemotherapy uses include the drug Cisplatin, which helps destroy abnormal cells.
In combination with surgery, therapy is carried out with cytostatic drugs aimed at suppressing the growth and death of cancer cells. Sarcoma of the lower jaw or upper jaw can be cured with medications such as:
- "Cisplatin";
- "Etoposide";
- "Ifosfamide";
- "Adriblastin";
- "Methotrexate";
- "Carboplatin".
Home therapy
Many alternative medicine products are prepared from conditionally poisonous plants, so they should be used only after consulting a doctor and strictly adhering to the dosage.
Sarcoma of the jaw can be cured with celandine juice. Recipe:
- Take the whole plant along with the root, wash thoroughly, and pass through a meat grinder.
- Place the resulting mass on cheesecloth and squeeze out the juice.
- Let it brew in a cool place for 3-5 days, filter.
- Add medical alcohol to the resulting juice in the proportions of 1 liter of plant liquid per 300 ml of alcohol.
- Drink 10 ml 3 times. per day.
Traditional healers offer a remedy from hemlock, which you need to drink 1 r. in a day. The course begins with taking 1 drop. drug diluted 5 tbsp. l. plain water. The number of drops must be increased by one every day until you reach 40. Preparation:
Hemlock infusion is recommended by traditional medicine as an effective antitumor agent.
- Take 5 tbsp. l. flowers and leaves of the plant and chop.
- Add 0.5 liters of vodka and mix thoroughly.
- Let it brew for 21 days, shaking occasionally, and filter after the period has expired.
An effective remedy from peony root is prepared as follows:
- Take 10 tbsp. l. chopped plant, add 0.5 liters of vodka.
- Let it brew for 30 days, filter.
- Take 5 ml 2 times. per day.
Treatment of soft tissue sarcoma
The choice of treatment for sarcoma is determined by the degree of its malignancy, location and presence of metastases. For the treatment of low-grade tumors, treatment is predominantly surgical; in other cases, combined methods are used, including radiation and chemotherapy.
Surgery
The following types of operations are used in the surgical treatment of sarcomas:
- Wide local resection. In this way, low-grade small tumors located in the skin and subcutaneous tissue are removed.
- Wide excision. With this intervention, the sarcoma is removed within the anatomical zone, retreating from the edge of the tumor by at least 4-6 cm.
- Radical organ-preserving surgery. With this volume of intervention, the tumor is removed along with the muscle fascia and intact muscles, which are cut off at the site of their attachment. If blood vessels, nerve trunks and bones are involved in the process, they are resected with one-stage plastic surgery using a skin or musculocutaneous flap.
- Amputation or disarticulation is the removal of a limb or its disarticulation along the line of the joint space. Such interventions are carried out in cases of extensive, locally advanced, highly malignant processes involving the main blood and nerve trunks over a long distance, as well as bone structures and muscles.
During surgery, an urgent intraoperative histological examination is required. If there are malignant cells at the cutting edges and with the potential for radical removal of the tumor, reoperation is performed.
Radiation therapy
Radiation therapy is used as part of combined treatment in the preoperative and/or postoperative stages. In the first case, the goal is to reduce the size of the sarcoma and create conditions for radical intervention. In the second - the destruction of the remaining malignant cells. To ensure a uniform effect on the tumor, multifield irradiation techniques are used.
Preoperative radiotherapy
During preoperative RT, the boundaries of the irradiation fields (FI) should extend beyond the size of the tumor tissue by at least 3-4 cm. If the tumor is large, irradiation is performed within 10 cm from its edge until a total focal dose of 45-50 Gy is achieved. Then the software is reduced to the size of the tumor.
If the tumor is located on a limb, there is a possibility of developing osteoradiation necrosis, muscle contractures and edema. To avoid this, it is recommended to irradiate no more than 2/3 of the circumference of the limb, if possible. The minimum thickness of non-irradiated tissue in the forearm area is 2 cm, on the thigh 4 cm, and on the lower leg - 3 cm.
Postoperative radiotherapy
Postoperative radiation therapy is indicated in the following cases:
- High degree of malignancy of sarcoma according to histological examination.
- A non-radical operation is the presence of malignant cells at the cutting edges when reoperation is impossible.
- Opening the sarcoma capsule during surgery.
Postoperative RT begins no later than 4 weeks after the end of surgical treatment.
If preoperative RT was not performed, the radiation fields include the following areas:
- Tumor bed.
- Tissues that are located at a distance of 2 cm from the removed tumor.
- Postoperative scar.
Irradiation is carried out at a total focal dose of 60 Gy. If non-radical surgery was performed, the dose is increased to 70 Gy. Radiation therapy is carried out in a similar mode if surgical treatment is not possible.
Chemotherapy
Chemotherapy is widely used to treat high-grade soft tissue sarcomas. As with radiation therapy, it can be prescribed preoperatively and/or postoperatively. Neoadjuvant (preoperative) chemotherapy is designed to affect the tumor site, destroy micrometastases and create conditions for organ-preserving surgical treatment. For this purpose, 2-3 courses of chemotherapy are carried out with a break of 3-4 weeks.
Postoperative chemotherapy can be performed to destroy micrometastases or already visualized metastases. For this purpose, 3-4 courses of treatment are performed. In the chemotherapy treatment of sarcomas, various combinations of the following drugs are used:
- Doxorubicin.
- Etoposide.
- Vincristine.
- Ifosfamide.
- Dacarbazine.
- Cisplatin, etc.
The chemotherapy regimen will be determined by the morphological variant of the tumor and its sensitivity to previous treatment.