In modern medical practice, arthritis of the jaw joint is not so common, but this pathology requires special attention, as it can lead to negative consequences and complications, including disability. Treatment of jaw arthritis is a long, labor-intensive process that requires an integrated approach, sometimes including surgical intervention. This is exactly what we will look at in this article.
Arthrosis of the TMJ - what it is and why the diagnosis is dangerous
Arthrosis of the temporomandibular joint - consequences of the inflammatory process in the tissues of the joint and chronic microdamage.
Jaw arthrosis occurs as a result of destruction of the articular and cartilaginous surface of the lower jaw.
As the disease develops, the main functions of the mandibular joint, formed by the temporal bone and jaw, are disrupted.
As a result of arthrosis of the temporomandibular joint, the cartilaginous disc and masticatory muscles, located between the bones and regulating the movement of the jaw, lose their functional features - opening the mouth and grinding food becomes problematic .
If left untreated, the disease progresses, affecting periarticular tissues, bone frame, muscles and ligaments with dystrophy, which in advanced stages leads to disability.
Complications
Arthrosis of the temporomandibular joint leads to severe impairment of its functions. The problem is that patients often consult a doctor in the later stages of the disease. In this case, deformation of the maxillary joint is already observed. It often causes the development of synovitis and reactive arthritis. The inflammation may spread to the teeth or ears. A person's hearing decreases and periodontitis develops.
Due to the fact that movements in the joint are limited, the patient’s speech and chewing function are impaired. Eating often causes serious problems, since sometimes a person can only open his mouth a couple of centimeters.
As the pathology progresses, hearing problems, severe pain, and difficulty chewing food may occur.
Reasons for development
Arthritis and arthrosis of the maxillofacial joint cause thinning of the cartilage tissue. With increased load on the joint, cartilage tissue begins to be replaced by bone, subsequently limiting the mobility of the mandibular joint. The reasons for the development of this disease can be:
- age-related changes,
- lack of physical activity,
- hormonal disorders,
- genetic predisposition,
- metabolic disease,
- arthritis, osteoarthritis, bursitis and other inflammations of the joints of the extremities,
- infectious diseases,
- pathologies of the endocrine and nervous systems,
- injuries to the head of the mandible or increased load when chewing,
- malocclusion, missing part of the dentition,
- unfavorable environment.
Pain dysfunction
With uneven (one-sided) load on the joint, severe pain dysfunction occurs.
It is characterized by the appearance of constant aching pain. It usually radiates to the cheek, ear, and back of the head. The ability to open the mouth normally is usually impaired. Palpation of the masticatory muscles usually causes pain. Treatment of pain dysfunction is aimed primarily at eliminating its manifestations. This can be achieved through the use of analgesics and sedatives. Drugs with muscle relaxant properties are indicated. Sirdalud is most often used for this purpose.
Classification
Osteoarthritis of the jaw joint is usually classified according to the nature of the damage into deforming and sclerosing .
Deformation of the jaw is accompanied by compaction of the head, fossa and articular tubercle, as a result of which the mobility of the joint decreases.
Sclerosing pathology is diagnosed in degenerative-dystrophic processes on the surface of the bone.
Based on the nature of origin a primary and secondary disease is distinguished: the secondary one manifests itself against the background of concomitant diseases of cartilage and joints, the primary one occurs independently with the natural depletion of tissues after 50 years.
The development of osteoarthritis of the temporomandibular joint occurs in four stages:
- Initial deformation and narrowing of joint spaces.
- Lack of stability of the TMJ, severe symptoms of sclerosis of the mandibular bone and hardening of the cartilage.
- Limitation of mobility and chewing functions of the jaw, compaction of the articular fossa and head, progressive degeneration of cartilage and sclerotic changes in the bone.
- The formation of fibrous ankylosis, which means complete immobilization of the joint.
What are the symptoms of the pathology?
This disease develops over a long period of time. At first, the patient does not notice the changes that occur in the body. Among the earliest signs of degenerative changes in the organ are clicking and crunching sounds, and stiffness in the morning. During the day, such symptoms gradually disappear. In the future, pain is added to such stiffness: first when talking and chewing, and then at rest. Painful symptoms intensify when the weather changes, often in the late afternoon.
Subsequently, the function of the joint is gradually limited. This becomes noticeable when the range of motion in the joint is limited. The following symptoms are noted:
- poor mobility;
- facial asymmetry;
- change in jaw position when opening the mouth;
- numbness on the affected side;
- pain in the tongue;
- pain in the ears, eyeballs, head, sometimes hearing loss.
Upon palpation and auscultation, crunching and crepitus are detected. When palpating the pterygoid muscle, the patient usually does not feel pain. Often the patient cannot open his mouth wide; in rare cases, the width of the mouth opening is no more than 0.5 cm. Sometimes a person moves the lower jaw to the sides in order to open the mouth normally.
In addition, with active movements, patients feel very sharp pain. The condition worsens sharply, the temperature rises, and chills occur. With purulent mumps, further spread of the inflammatory process to the salivary glands and inner ear is possible. Characteristic symptoms of mumps and otitis occur.
Symptoms
Arthrosis of the TMJ in the initial stage is asymptomatic, so, most often, the disease becomes a chronic, difficult-to-treat form.
A characteristic feature of the pathology is a crunching or clicking sound when opening the mouth..
The patient complains of constant aching pain in the jaw, tinnitus, and stiffness of movements in the lower jaw after waking up.
The pain can intensify with hypothermia and increased load on the joint (chewing solid food, prolonged conversation). This fact forces a person to chew food on one side, despite the fact that the pain spreads to the entire joint when moving.
Chronic arthrosis of the jaw joint causes discomfort at the slightest movement of the jaw, clicking and crunching every time you open the mouth, and incessant pain.
What reasons can provoke the disease?
Arthrosis of the jaw joint is a chronic disease that is caused by destructive changes. Diseases, as well as pathological processes occurring inside the joint, can deform the maxillary joint. Pathology occurs for a number of the following reasons:
- chronic arthritis;
- malocclusion;
- partial edentia;
- improper prosthetics or dental fillings;
- post-traumatic syndrome (jaw injury);
- age after 50 years, since during this period the ability of cartilage to regenerate decreases;
- the period of menopause in women is caused by the cessation of the production of sex hormones involved in the metabolic processes of the osteochondral system;
- hereditary predisposition;
- constant load on the jaw due to the habit of chewing hard food.
A child may develop this phenomenon as a consequence of a congenital malformation of the jaw or bruxism - teeth grinding during sleep, causing pathological tooth wear. This leads to improper functioning of the joint. Often the cause of pathology in children is a traumatic factor.
Advice! When the first manifestations of the disease appear, you should consult a doctor to prevent the development of negative consequences.
Diagnostic methods
Comprehensive instrumental diagnostics in combination with anamnesis collection allows us to form a clinical picture and prescribe effective treatment methods.
Based on the initial examination, the doctor can determine the symptoms of arthrosis of the maxillofacial joint and prescribe treatment after confirming the primary diagnosis.
Degenerative-dystrophic processes become distinguishable already in the advanced stage of the disease, when the following signs are most manifested:
- facial asymmetry,
- inability to move the lower jaw,
- numbness of facial tissues,
- headache, tinnitus,
- compaction of cartilage and bones (diagnosed by palpation),
- pathological injuries,
- crunching sound when opening mouth,
- inflammation of the TMJ.
Arthrosis of the jaw joint - your dentist or orthopedist will tell you what it is and how to treat the disease.
Why the disease may develop
This pathology is of chronic origin. Arthrosis of the TMJ is caused by long-term degenerative processes in tissues. They are accompanied by impaired performance of the lower jaw. The problem is common. According to the latest data, signs of this disease occur in approximately half of patients after 50 years of age. In people over 70 years of age, this pathology occurs in 90% of cases, regardless of gender.
Arthrosis of the jaw is diagnosed most often in young women. The treatment of this pathology is carried out by specialists of various specialties - dentists, orthopedists, orthodontists, surgeons, traumatologists, physiotherapists.
Arthrosis of the jaw joint is a multifactorial pathology. Its causes can be both local and general. Local factors for the development of the disease include:
- chronic arthritis of the maxillofacial joint;
- bite pathologies;
- edentia (most often the absence of molars in the lower jaw);
- enamel pathologies;
- bruxism;
- improper installation of seals;
- errors in the process of dental prosthetics;
- injuries;
- a history of surgery on the jaw joint.
Among the common factors for the occurrence of such a disease:
- unfavorable heredity;
- disturbances in the functioning of the endocrine glands;
- vascular pathologies;
- systemic diseases;
- infections;
- in women - menopause and a decrease in the production of female sex hormones due to age-related changes;
- pathologies of bone tissue and cartilage.
The pathogenesis of this disease is associated with additional load on the joint part, which is above the limit of normal endurance.
This happens as a result of constant microtrauma, inflammation, and metabolic disorders in the body. The pathology of the masticatory muscles gradually develops. All of these processes provoke changes in the tissue nutrition of the articular part, and a loss of the elastic properties of its tissues occurs. The head of the jaw gradually changes its shape (becomes club-shaped, mushroom-shaped, hook-shaped). It diagnoses signs of osteoporosis.
Treatment of jaw joints
Treatment of jaw joint pathology requires an integrated approach, including physical therapy, medications, exercises, orthodontic services, diet, and in some cases, surgery.
Timely treatment plays an important role in recovery, since in advanced stages the function of the jaw joint is completely lost.
It is important to understand that secondary arthrosis of the TMJ can be treated only after eliminating the root cause of bone degeneration - without this, there is no point in hoping for recovery of the jaw.
Let's consider what methods of treatment of arthrosis of the maxillary joint doctors have today.
Drug therapy
Deformation of cartilage tissue and bones leads to increasing pain syndrome, which bothers the patient due to the development of sclerosis and tissue inflammation.
To eliminate them, symptomatic treatment with non-steroidal anti-inflammatory drugs is provided. Ketorol, Ketoprofen, Ibuprofen, Nurofen and other drugs are suitable for these purposes; before taking, consultation with a specialist is required.
Physiotherapy methods for TMJ
The doctor may prescribe physical therapy in combination with other treatment methods or as the main means in the fight against pathology.
The problem is dealt with by electrophoresis, paraffin therapy, mud baths, infrared exposure, phonophoresis, laser therapy, and heating with medical bile.
The main goal of physiotherapy is to reduce the clinical manifestations of arthrosis arthritis and prevent further bone destruction.
Capabilities of orthodontists and maxillofacial surgeons
The success of treatment for arthrosis of the temporomandibular joint when contacting an orthodontist lies in the timely elimination of physical imperfections of the jaw that contribute to overload of the joint.
The main task of the doctor is to ensure a uniform load over the entire area of the TMJ.
The dentist performs teeth grinding, which ensures proper chewing of food and reduces wear on tooth enamel. If the dental crown is significantly damaged, the doctor makes and installs artificial crowns or dentures.
In case of congenital malocclusion, the help of an orthodontist in installing braces or mouth guards is required.
After 4-6 months of treatment carried out by the dentist, the patient is prescribed exercises to restore jaw function.
Principles of rational diet therapy
A diet for arthrosis and bursitis of the jaw joint is necessary to reduce the load on the masticatory muscles and restore metabolism.
exclude solid foods from your diet (crackers, raw foods, fruits, vegetables and root vegetables, nuts, etc.).
You should limit the consumption of foods with a purine base : mushrooms, legumes, meat and fish, alcohol, sugar, cocoa, coffee, smoked meats, marinades.
Particular attention in the diet is drawn to foods rich in healthy fats, proteins and vitamins: cottage cheese, eggs, fresh (but not hard) vegetables and fruits, lean meats and fish, cereals.
Surgery
A severe form of jaw arthrosis is treated by surgical removal of the interarticular cartilage and part of the head (or its complete removal and replacement with an implant). As a result of the operation, the natural position of the head is restored, the height of the tubercle of the articular tubercle increases and excessive mobility of the TMJ is reduced.
Traditional medicine - pros and cons
A frequent question to an orthopedist asked by patients: “How to treat the jaw joint with folk remedies at home,” does not have a place in the treatment of a complex stage of arthrosis, since folk remedies cannot be used to get rid of bone disease on your own.
ATTENTION ! Traditional recipes can contribute to a deterioration in health, so their use is not recommended by doctors.
Decoctions and herbal infusions can only be used as a preventive measure to strengthen the body's immunity and metabolic processes.
Treatment of traumatic arthrosis
This type of disease occurs as a result of severe injuries to this area. The main task of the surgeon is to achieve immobility of the joint. This can be achieved by applying a so-called sling bandage. It securely fixes the jaw and prevents sudden movements.
Wearing a sling bandage is recommended for 2 to 3 days if the patient develops arthritis of an infectious nature. The period of wearing a bandage for injuries of the jaw joint increases to 10 days. During this period, in order to avoid complications, it is recommended to eat only liquid foods.
If traumatic arthritis is accompanied by edema, the patient is usually prescribed drugs to stimulate impaired blood circulation in diseased tissues. To reduce the intensity of the inflammatory process, antibiotics are prescribed. Additionally, immunomodulators are recommended to improve the functioning of the nervous system.
Prevention
Since the pathology of the temporomandibular joint develops as a result of the destruction of bone and cartilage tissue, it is important to prevent these processes in the body.
Engage in physical activity regularly, make sure that the body receives all the necessary vitamins and minerals, avoid overstraining muscles and joints, hypothermia, and lack of sleep. Have your oral cavity examined by a dentist at least once every 6 months. Following simple recommendations will help maintain healthy bones.
Methods for diagnosing the disease
The sooner you start treating arthrosis, the greater the likelihood of a favorable outcome. The diagnosis is made on the basis of functional data and radiography. If the patient goes to the dentist, the complaints are analyzed, the oral cavity is examined, and the muscles and joints are palpated. The regularity of movements in the joint is carefully determined.
The main diagnostic method is radiography of the joint. With its help, the initial signs of arthrosis are detected. Computed tomography allows you to more accurately determine such changes in the joint. Additionally, the following examinations are carried out:
- arthrography;
- orthopantomography of the jaw;
- electromyography;
- rheography;
- arthrophonography;
- axiography.
A consultation with an orthodontist, endocrinologist, and rheumatologist is indicated.
This disease is differentiated from arthritis, dysfunction of muscles and joints, chondroma, osteoma.
Why the jaw joint may hurt, common problems and methods of treatment
A common problem that affects patients of all ages is pain in the jaw joint when chewing and opening the mouth.
Sometimes it is felt on one side (left or right), in other cases - on both. Soreness can radiate to the facial muscles, chin, cheekbones and neck, and be aching or sharp. Even a child can complain that his jaw joint hurts. Sometimes this happens if he opens a bottle with his teeth or cracks nuts.
The lesions can be one or more articular joints: maxillofacial, maxillary, temporomandibular. One way or another, the patient’s goal is to find out what pathology the symptoms in question are a sign of.
He needs to undergo an examination in order to quickly diagnose the pathology and select the optimal treatment regimen.
Trying to cure yourself at home with folk remedies and refusing to see a doctor, the patient only aggravates the symptoms that torment him.
Localization of the temporal articular joint relative to the jaw and destruction of cartilage tissue in arthrosis
Causes of pain
The causes of pain in the lower jaw and joints, according to their genesis, can be divided into several categories:
- Associated with pathologies (degenerative or inflammatory) of the cartilage of articular joints.
- Diseases and phenomena not related to joints, such as bruxism, runny nose, tumors, wisdom teeth erupting, wearing braces.
- Impacts and other traumatic injuries to bones and joints.
- The patient misuses the jaws - opening bottle caps with them, abusing chewing gum, etc.
Diseases of the jaw joints
Jaw diseases can occur as a result of an inflammatory process, which is most often caused by an infectious agent that penetrates the cartilage of the joint linings through the bloodstream or through an open wound.
The most common joint pathologies are:
- ankylosis - fusion of bones, causing immobility;
- arthrosis is a degenerative disease;
- arthritis - inflammation of the joint;
- neuralgic disorders;
- osteomyelitis.
Problem areas of the mandibular joint
Osteomyelitis of the lower jaw
This is one of the types of inflammatory diseases of the jaw. Its initiator is an infection that seeps into the bone tissue of the jaw through carious teeth. Standard symptoms are:
- Hyperplasia of the cervical lymph nodes.
- Pain in the temporomandibular joint, the bones of both jaws - often on both sides, but possibly only on one.
- Pain in teeth.
- Hyperthermia, febrile symptoms.
- An obvious increase in inflammatory markers observed when a patient with osteomyelitis is referred for a blood test.
The patient needs to visit the dentist. His diseased teeth will be removed and his mouth will be sanitized. If the patient develops purulent formations, they are removed surgically.
Dislocation of the jaw joint
Joint dysfunction syndrome and neuralgia
This syndrome is associated with intense tension in the mandibular joint. Its traditional symptoms are:
- pain while chewing food;
- Clicking or grinding sounds of the jaw moving.
Also, characteristic pain occurs with neuralgia affecting the glossopharyngeal nerve. Their characteristic manifestation is increased pain when palpating the affected area.
Treatment of these pathologies includes:
- taking analgesic drugs;
- creating peace for a sore jaw;
- injections of drugs that reduce muscle tone;
- use of cooling bandages.
Arthritis of the temporomandibular joint
This is an inflammatory process of joint elements, usually affecting cartilage pads and synovial fluid. Sometimes inflammation can spread to adjacent soft tissues. The disease accounts for about one sixth of all cases of dysfunction of the TMJ.
The disease, especially in its acute form, manifests itself with vivid clinical symptoms and, without proper prompt treatment, results in very unpleasant consequences: cartilage breakdown, its replacement with connective tissue formations, ankylosis, and deforming osteoarthritis.
Reasons for the development of the disease:
- The most common inflammation is caused by an infectious agent that enters the body through lesions on the skin or penetrates the joint tissue with the blood.
- Rheumatoid arthritis is associated with dysfunction of the immune system. Acquired heart defects often develop against this background.
- The disease can also develop after injury.
- Reactive arthritis due to a viral infection.
The symptoms of arthritis are very recognizable:
- sharp pain that intensifies when moving the jaw and opening the mouth;
- swelling;
- phenomena of fever.
Osteoarthritis and dislocation of the lower jaw
This pathology is rooted in the destruction of articular cartilage tissue. Its gaskets wear out, the gap between the epiphyses of the bones narrows, the bones begin to rub against each other, which creates a characteristic crunch when moving the joint.
The pain is aching, not acute, and manifests itself during movements (talking, chewing). The muscles of mastication may also hurt. The range of mobility narrows (it is more difficult to open the mouth or move the jaw from side to side), which is especially pronounced after sleep.
In advanced stages, facial asymmetry is also observed.
Pathologies of the temporomandibular joint
These include neuralgic pathologies:
- Trigeminal nerve - the jaw will always hurt on only one affected side.
- Superior laryngeal nerve. Pain occurs when yawning, blowing your nose, eating, and may be accompanied by hiccups or coughing.
- Glossopharyngeal - short attacks of pain in the tongue, which can radiate to the jaw, face or chest. Ends with copious secretion of saliva.
Bone fracture and its types
Fractures occur due to mechanical trauma caused by an external factor. The consequences of lack of treatment in this case may be loss of teeth, headaches, jaw deformation, problems with the innervation of certain areas. Fractures can be comminuted, closed or open. What to do if the patient receives this type of injury:
- Call an ambulance.
- While waiting for an ambulance, provide rest to the jaw and secure the maxillofacial joint with a bandage.
The patient will be taken to the clinic, where he will be examined, the type of surgical intervention required will be determined, and therapeutic measures will be organized to help eliminate discomfort (certain pills and injections).
Malocclusion
Improper teeth alignment can also cause jaw pain. Such a patient needs to visit an orthodontist, who will prescribe treatment that is relevant to the case.
Jaw injury with tooth displacement
Wearing braces and dentures
Oddly enough, pain when wearing braces is a positive sign, indicating that the teeth are shifting to form the correct bite. When wearing removable dentures, such a symptom is normal at the initial stage of addiction, but if it persists for a long time, you need to visit a doctor.
Wisdom tooth growth
Since the jaw shrinks somewhat with age, teething is sometimes associated with pain and swelling of the cheek and gums. In this case, it is important to take a pain reliever and visit a dentist.
Inflammatory processes
In addition to the previously mentioned osteomyelitis, these include:
- Boils are pustular formations on the skin, dangerous due to the penetration of infection and purulent masses into the cranial cavities.
- Cellulitis is a lesion of soft tissue. Not only the jaw can hurt, but also the space under it. Also associated with swelling and hyperthermia.
Tumors
The presence of a tumor formation in the jaw is always accompanied by severe pain. There are several types of tumors characteristic of this organ. Benign:
- Osteoid osteoma. For a long time it does not make itself felt by any symptoms, but in the mature stages the patient suffers from sharp pains at night, and he also develops facial asymmetry.
- Adamantioma is a hyperplasia of the jaw. The pain gets worse when eating.
- Osteoblastoclastoma. Here, soreness of the jaw is the earliest symptom, and later are trophic changes in the gums and soft tissues of the face.
Malignant tumors:
- Sarcoma is a lesion of areas of connective tissue with progressively increasing shooting pain.
- The osteogenic variant of sarcoma is bone cancer. On palpation, the pain diffuses to other areas of the face.
What to do if you have joint pain?
When a patient comes in, the doctor examines the jaws and takes functional tests. Next, the patient is sent for instrumental examinations: magnetic resonance imaging and x-ray of the jaw.
If an inflammatory process is suspected, a general blood test is also prescribed. The treatment program is based on the results of the analysis.
By correctly identifying the cause of the pathology, you can restore the functionality of the jaw in a short time and avoid serious complications.
Source: //LechiSustavv.ru/zabolevaniya-chelyustno-litsevogo-sustava/9813-bolet-chelyustnoy-sustav.html
Treatment with traditional methods
The goal of treating arthrosis of the jaw joint using folk remedies is to eliminate the symptoms of the disease and its causes. The most commonly used are ointments, compresses, and tinctures.
The best ways to treat arthrosis at home are as follows:
- A mixture of cranberries, honey and garlic is crushed using a meat grinder. Internal use of such a remedy significantly improves the nutrition of tissues affected by the disease, relieves inflammation and pain. It is advisable to take this mixture before eating.
- Before each meal, it is advisable to drink apple cider vinegar diluted with water. This medicine is very good at removing salt deposits in the body. A course of treatment lasting at least 1 month helps to normalize metabolic processes in the muscles.
- Treatment with beekeeping products gives a powerful anti-inflammatory and restorative effect. Using bee venom as a remedy helps activate the immune system and strengthen body tissues. Before using beekeeping products for medicinal purposes, you must make sure there is no allergy.
Before using folk remedies, it is advisable to consult a doctor.
What is arthrosis?
Arthrosis is a chronic disease that primarily damages articular cartilage. The pathology develops, involving the joint, ligaments and muscles in the process. The development of this pathology is due to a disruption in the processes of cellular formation. The basis is a primary lesion of cartilage with an inflammatory reaction.
The surface of articular cartilage consists of complex tissue, which includes collagen and proteoglycans. The joint experiences a load that is evenly distributed thanks to the collagen network. With the loss of proteoglycans, the network's resistance to external influences weakens. The articular cartilage first becomes thicker, then loosens, becomes thinner, and ulcerations appear in it.
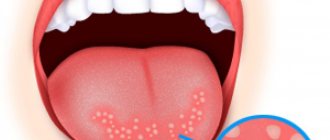
Arthrosis causes damage to the articular cartilage
Osteoarthritis of the jaw occurs in the joint that connects a person’s lower jaw to his skull. The mandibular joint makes active movements up and down, right and left and back and forth. The pathological process reduces the range of motion in any direction.
Bursitis of the knee joint: symptoms, treatment and photos
Knee bursitis is a very unpleasant disease. It occurs as a result of the development of inflammatory processes in the joint capsule. The most common cause of this disease is injury or heavy physical activity, which results in the release of large amounts of intra-articular fluid from the synovial membrane of the knee joints.
- Bursitis of the knee joint: photos, causes
- Symptoms of knee bursitis
- Diagnosis of knee bursitis treatment
- Treatment of knee bursitis Local treatment
- Traditional methods to alleviate the condition
- Surgery
In this way, the body reacts to remove too much tension in the joint and minimize the negative effect of the resulting injury. But there comes a time when the volume of intra-articular fluid exceeds the permissible limit, as a result the body is no longer able to process it. This leads to its accumulation in the cavities of the synovial membrane. The consequence of this is the development of bursitis of the knee joint, which is characterized by its own symptoms and certain treatment methods are used.
Bursitis of the knee joint: photos, causes
Not in every case it is possible to detect the causes of bursitis. There are patients who develop this disease without serious reasons. The most common factors that cause the development of this disease are:
- Injuries and damage to the knee joint.
- Sprain of a joint caused by excessive tension;
- Significant physical activity exceeding the permissible limit.
- Inflammation of the joints, leading to the development of characteristic diseases, such as gout.
- Penetration of infection.
The location of the inflammatory processes largely determines the type of bursitis:
- Patellar or suprapatellar bursitis. It is most often found in patients who complain of inflammation of the patellar bursa.
- Popliteal or infrapatellar bursitis. A condition in which inflammatory processes affect the popliteal bursa.
- Baker's cyst. A situation that results in damage to the synovial bursa located in the lower inner part of the knee joint.
There are also two additional types of this disease:
- Serous bursitis. A condition in which inflammation of the synovial bursa is noted, not associated with the activity of microbes. As a rule, it is caused by injury or sprains.
- Purulent. In this case, the cause of the disease is the penetration of pathogenic microorganisms into the cavity of the bursa, as a result of which pus begins to form. Most often, the path to the synovial bursa for bacteria opens through wounds and cracks in the skin.
Depending on the nature of the disease, acute and chronic bursitis are distinguished. This, in turn, determines the symptoms of the disease, as well as the method of its treatment.
Symptoms of knee bursitis
Knee bursitis can be identified by its pronounced symptoms.
- Inflammation and pain, which is acutely felt when you press on the area next to the joint.
- Significant stiffness or limited range of motion in the affected joint.
- Signs of redness or swelling in the affected joint.
- Feeling of weakness in the muscles.
- Weakness, malaise, decreased performance.
- Increased temperature in the area of infection.
- A general increase in body temperature, which is often observed with infectious bursitis.
If the bursa is subjected to prolonged mechanical stress, chronic knee bursitis may develop against this background. During the course of the acute form of the disease, the main symptoms will be associated with inflammatory processes in the walls of the bursa.
Diagnosis of knee bursitis treatment
The specialist chooses treatment based on the results of the examination, but first he has to find out the cause of the disease. When prescribing various diagnostic procedures, the doctor needs to make sure of the aseptic nature of the inflammation of the disease. This can be done by puncturing the bursa.
- If the test results revealed a clear liquid, then it follows that aseptic inflammation occurs.
- If pus is detected, it can be assumed that bursitis was caused by pathogens.
- It is not difficult to identify a Baker's cyst, since it usually occurs in a characteristic location - the popliteal fossa.
- If there are signs of popliteal bursitis, it is often necessary to resort to a group of instrumental diagnostic methods - ultrasound, arthrography, radiography of the knee joint.
In principle, identifying this disease is quite simple. If an experienced doctor is involved in this, then you can get a picture of the disease based on the results of a general examination and palpation examination.
Treatment of knee bursitis
When confirming the diagnosis of knee bursitis, the doctor is required to propose a program of therapeutic measures that should remove all causes of inflammation and reduce its severity. This problem can be solved by including the following activities in the treatment program:
- Rest for the joint;
- Treatment with medications;
- Physiotherapeutic procedures.
When choosing the most effective treatment methods for knee bursitis, it is necessary to proceed from the nature of the disease. If an aseptic form of inflammation of the synovial bursa has been identified, then during treatment it is necessary to follow a number of recommendations:
- Creating conditions under which the knee will be at rest;
- Reduce inflammation with ice compresses;
- Prescribing anti-inflammatory and painkillers;
- Taking muscle relaxants that effectively remove spasm of muscle tissue and blood vessels;
- Aspiration of synovial fluid. It is prescribed in cases where a large amount of fluid has accumulated in the bursa.
If the diagnostic results revealed a septic form of the disease, then treatment is reduced to taking antibiotics. At the same time, it is necessary to remove the bursa pus using the aspiration method; also in this form, drainage of the joint capsule is indicated.
Local treatment
To eliminate unpleasant symptoms, you can use a wide variety of anti-inflammatory ointments:
- voltaren emulgel;
- traumeel;
- diklak;
- DIP relief;
- chondroxide;
For external use, compresses prepared from dimexide and 0.5% novocaine solution are indicated. These components are taken in a ratio of 1:3:
- A gauze napkin must be dipped into the prepared mixture, and then a compress is applied to the affected area;
- You need to put a film on a napkin, and wrap the area with a scarf or towel on top.
It is necessary to keep these compresses on the joint for no more than half an hour, otherwise there is a danger of severe burns.
Traditional methods to alleviate the condition
During the time that doctors have known about this disease, many traditional medicine recipes have been accumulated that can effectively relieve the symptoms of knee bursitis. Among them, we can distinguish a group of folk methods that best help alleviate the patient’s condition:
- Cabbage compress. Helps relieve joint inflammation and pain. The compress is prepared as follows: you need to take a leaf, clean it of coarse veins, soften it with a rolling pin so that the juice appears, after which the cabbage leaf is placed on the site of inflammation, which must first be lubricated with honey. Next, the affected area should be wrapped with film and a scarf on top. Honey is necessary here so that cabbage juice can penetrate to the maximum depth and exhibit its antiseptic properties. The combination of cabbage juice and honey is very effective because it perfectly draws out the fluid with the infection. These compresses last for about 4-8 hours.
- Celery tea. With regular use of this drink, you can not only improve immunity, but also remove existing inflammation. The recipe for its preparation is as follows: you need to take one tablespoon of celery seeds, add a glass of boiling water to them, then let the mixture brew for 1.5-2 hours. The finished product must be filtered. Take the drink twice a day, the course duration is 14 days.
- Lotions with propolis. To prepare the product, you need to take 10 grams of propolis, add half a glass of 40% vodka to it, after which the mixture is left to infuse for 5 days. Lotions are made from this mixture, which are stopped when the swelling subsides.
- Ice cubes, which must be tightly wrapped in a bandage before placing on the affected area, can help cope with an exacerbation of the disease.
Preventive actions
Prevention of such a disease comes down to certain measures:
- improving the quality of nutrition;
- increased physical activity;
- fight against bad habits;
- thorough oral hygiene;
- timely correction of bite defects, sanitation of the oral cavity;
- regular visits to the dentist.
Osteoarthritis of the jaw joint is a fairly common disease. It responds well to treatment in the early stages. If the disease is neglected, the results of therapy will not be as good.
Everyone has the power to prevent disease. It is very important to visit your dentist regularly to treat possible joint dysfunction. In advanced cases, the patient is recommended to undergo surgical treatment to restore the joint. Modern medical technologies make treatment simple and painless.
Diagnosis of TMJ arthrosis
A disease such as TMJ arthrosis has been well studied and also has clear rules and diagnostic methods necessary for further treatment. The basis of diagnosis lies in the data obtained as a result of a medical examination. Also in diagnosis, an external examination of the patient by palpation of the affected side plays a significant role. The full picture of the disease is revealed by the results of tests and instrumental examinations. To treat arthrosis of the TMJ and establish a diagnosis, you must consult a dentist. It is during the dental examination that any dental anomalies (bad bite) are detected and the general condition of the teeth and dentures is assessed. The main indicator of TMJ arthrosis during a dental examination is traces of pathological abrasion of tooth enamel.
After a preliminary examination, the dentist prescribes an x-ray examination. It is based on its data that the nature of the pathological process of the joint will be established. The presence of stage 1 TMJ arthrosis in a patient is indicated by a slight narrowing of the joint space, and the disease is also indicated by the growth of bone osteophytes. The second stage is diagnosed by indicators such as osteosclerosis, destruction of cartilage tissue.
In the second and third stages of arthrosis of the TMJ, an X-ray image of the patient indicates a clear deformation of the bone and a decrease in the ligamentous apparatus, and contracture is formed. Additional diagnostic methods include computed tomography and blood tests, which are necessary to identify the inflammatory process.
General therapy
Treatment of arthrosis of the maxillofacial joint depends on the degree of tissue deformation. Advanced forms are eliminated promptly by removing the joint disc and the head of the jaw. If necessary, transplantation is performed after excision of the head.
If the patient visits the doctor in a timely manner, he can avoid surgery. Scheme for gentle treatment of arthrosis of the maxillary facial joint:
- Taking anti-inflammatory and painkillers that are effective at any stage of the disease. Medicines of these groups are prescribed against tinnitus, migraines, and inflammation.
- Adding medications that nourish and renew cartilage tissue. They quickly restore processes that occur in the joint with disturbances.
- Restoration of teeth if they provoked a disease.
- Physiotherapy. It includes laser and microwave radiation, dynamic current therapy, ultrasound, and electrophoresis. Using these methods, inflammation is relieved and tissues are restored.
- Dieting. Gentle nutrition will help reduce the load on the joint. It is better to eat soft foods.
- Other advice from doctors. During therapy, the patient must protect himself from stress and nervous tension, otherwise bursitis will occur. It is recommended to give up chewing gum, long conversations, and other bad habits.
Pathology can be caused by a lump that appears in the ear area, under the jaw. The reasons for the development of arthrosis include a broken bite. In this case, the arthrologist writes out a referral to the dentist for the patient. If suspicions are confirmed, bite plates and braces are installed.
For mild cases of the disease, treatment is carried out at home. In severe cases, the patient is hospitalized. For any degree of damage to the jaw joint, the doctor’s task is to eliminate the disease itself and its symptoms. At an early stage, damaged tissue and cartilage can be partially restored. With a moderate course of the disease, doctors can achieve stable remission.
List of medications
List of medications
Doctors include drugs from different pharmacological groups in the treatment regimen for arthrosis. To relieve swelling and inflammation, taking NSAID medications is indicated. The patient is prescribed Ibuprofen and Ketorolac. A drug blockade is carried out. Swelling with inflammation contributes to pinching of the trigeminal and facial nerves. If the periosteum is inflamed and diagnostics reveals an infection, the patient is prescribed antibiotics.
To normalize metabolism, it is necessary to remove salt deposits. A lack of blood flow to the problem area will only worsen the situation, so vasodilators are included in therapy.
If radiological symptoms indicate initial degeneration, the patient is prescribed chondroprotectors, for example Chondroitin, Glucosamine sulfate. Due to their long-term use (up to 6 months), cartilage is restored. The maximum effectiveness of drugs in this group has been proven in mild cases of the disease.
To provide the affected tissue with microelements, the diet includes minerals, vitamins, and calcium supplements. To reduce the activity of the disease, hormonal corticosteroids are indicated. Medicines are prescribed to the patient in the form of ointments, injections, and tablets.
Folk remedies
Alternative medicine methods in the treatment of jaw arthrosis are used after consultation with a doctor. These include the use of tinctures, compresses, and ointments from medicinal herbs. Medicine prepared from 200 g of garlic, 500 g of cranberries, 1 kg of honey will help against arthrosis. The first two components are ground in a blender. It is recommended to eat 1 tsp per day. prepared composition.
Other effective folk remedies for the disease:
- For 2 tsp. Apple cider vinegar will require ½ cup of water. The solution is drunk on an empty stomach for 30 days. Therapy is repeated after 3 months. Using this recipe, you can wash salt deposits from the body, normalizing blood circulation in the tissues.
- Apitherapy is prescribed to activate the immune system. Bee venom is considered a powerful antibiotic that can cause a rush of blood.
- If pain in the nose occurs, it is recommended to prepare drops of celandine juice and honey. The ingredients are infused until a homogeneous composition is formed. The solution is instilled 2 drops into the nose.
- If severe noise in the ears occurs, it is recommended to prepare an ointment from a chicken egg. You can leave the product on your face until the morning.
- For 2 tsp. Apple cider vinegar will require ½ cup of water. The solution is drunk on an empty stomach for 30 days. Therapy is repeated after 3 months. Using this recipe, you can wash salt deposits from the body, normalizing blood circulation in the tissues.
- Apitherapy is prescribed to activate the immune system. Bee venom is considered a powerful antibiotic that can cause a rush of blood.
- If pain in the nose occurs, it is recommended to prepare drops of celandine juice and honey. The ingredients are infused until a homogeneous composition is formed. The solution is instilled 2 drops into the nose.
- If severe noise in the ears occurs, it is recommended to prepare an ointment from a chicken egg. You can leave the product on your face until the morning.
To prepare the tincture you will need St. John's wort, horseradish roots, mint, and celandine. Herbs take 5 g of each, crushed and poured with hot corn oil. The medicine is infused for 40 days. Then it is squeezed through nylon fabric. Propolis is added to the remaining oil.
The composition is infused for another 3 weeks. Separately, 100 g of turpentine is poured into a container, 20 g of crushed rosin is poured. The sealed container with the solution is kept warm until the rosin dissolves, after which the two compositions are mixed. The resulting product is used as a compress.