Description and causes of the disease
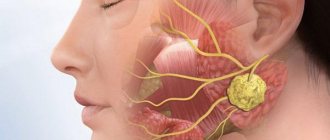
Cellulitis of the lower jaw due to inflammation of the tooth root
Phlegmon of the lower jaw is purulent inflammation in the fatty tissue. Outwardly it looks like a small red tumor on the right or left. Pain, signs of intoxication gradually appear, the temperature rises, and the lymph nodes enlarge. ICD-10 code for adenophlegmon of the submandibular region is K12.2.
As the disease develops, the infectious process spreads through the vessels inside the maxillofacial area. The soft tissues of the neck, pharynx, mediastinum, and esophagus swell, and the symmetry of the face is disturbed.
The causative agents of the pathology are staphylococci, streptococci, and in children - hemophilus influenzae. These microorganisms are classified as opportunistic. Active growth begins with a decrease in immunity.
High blood sugar increases the risk of developing cellulitis
Causes of the disease:
- advanced diseases of the oral cavity - cysts, periodontitis, periodontitis, osteomyelitis of the jaw;
- problematic wisdom teeth;
- injury to the sublingual area;
- diabetes;
- dermatological pathologies - boils, purulent rashes on the face;
- ulcerative form of stomatitis;
- exhaustion of the body;
- chronic diseases, allergies.
Cellulitis is an infectious, but not contagious disease.
Characteristic local signs of abscess, phlegmon of the temporal region
Complaints of pulsating pain in the temporal region, the intensity of which depends on the depth of localization of the infectious-inflammatory process: the deeper the purulent-inflammatory focus is located, the more intense the pain.
Objectively. There is asymmetry of the face due to swelling of the tissues of the temporal region, the severity of which depends on the prevalence of the infectious-inflammatory process and its localization: the more superficial the purulent-inflammatory focus is located, the greater the swelling of the tissues and the brighter the hyperemia of the skin above the inflammatory infiltrate. Palpation of the infiltrate causes pain. When the process is localized in the subcutaneous fatty tissue, the inflammatory infiltrate often does not have clear boundaries and can spread to neighboring anatomical areas (frontal, parotid-masticatory, zygomatic, eyelid area), while the inflammatory infiltrate with an abscess, phlegmon of the subgaleal, axillary retinal space at the top is strictly limited by the temporal region - the line of attachment of the temporal aponeurosis. With an abscess of the interaponeurotic space, the inflammatory infiltrate occupies the lower part of the temporal region and has a clearly defined border along the zygomatic arch. Dysfunction in the form of limited mouth opening due to inflammatory contracture of the temporal muscle can be observed with an abscess, phlegmon of the subgaleal cellular space and, especially clearly, when the purulent-inflammatory focus is localized in the axillary cellular space.
How does the disease manifest itself?
Swelling of the neck and redness of the skin due to phlegmon
Phlegmon has a characteristic clinical picture. The severity of symptoms depends on the type of pathology and the person’s immunity.
The main symptoms of phlegmon of the lower jaw:
- the tongue swells, moves worse, a gray-brown coating forms on the surface;
- slurred speech, impaired swallowing and chewing functions;
- increased salivation, heavy breathing;
- weakness, headache, other manifestations of intoxication;
- unpleasant putrid odor from the mouth;
- painful swelling on the face.
If the phlegmon is not deep, facial features are distorted, the nasolabial fold on one side is smoothed out, and the skin becomes very shiny. If the peripharyngeal area is affected, problems with breathing and chewing occur.
Cellulitis of the infraorbital, zygomatic and buccal areas, phlegmon of the orbit, treatment of phlegmon
1. Topographic anatomy of the orbit; infraorbital, zygomatic, buccal areas. The infraorbital region has the following anatomical boundaries: the inferior orbital margin, the alveolar process of the jaw, the base of the lateral walls of the nose, the zygomaticomaxillary bone suture. In the infraorbital region there are facial muscles, ... The boundaries of the zygomatic region correspond to the boundaries of the zygomatic bone: from above it approaches the lower edge of the temporal fossa and the edge of the orbit, in front to the infraorbital fossa, downwards - to the cheek, behind - to the parotid-masticatory region. The buccal region is enclosed between the laughter muscle, the masticatory muscle itself, the edge of the zygomatic arch and the edge of the lower jaw.
In the buccal area, under the skin and subcutaneous tissue, the fatty body of the cheek is located. Outside, it is enclosed in a fascial sheath that passes from the anterior edge of the masticatory muscle (parotid-masticatory fascia). Internally, it is limited by the buccal-pharyngeal fascia, which separates the fat body from the buccal muscle. The buccal-pharyngeal fascia covers the buccal muscle and behind it passes to the lateral wall of the pharynx. Below the buccal fat pad on the buccal muscle are the buccal artery, vein and nerve, as well as lymph nodes.
The fatty body of the cheek has three processes - temporal, orbital and pterygopalatine. They are also covered with a capsule, but on the processes it is much thinner. The temporal process rises under the zygomatic bone, between the outer wall of the orbit and the anterior edge of the temporal muscle. In the anterior parts of the infratemporal fossa, the orbital process departs from the temporal process, which is directly adjacent to the membrane covering the inferior orbital fissure, and if there are defects in it, it directly passes into the retrobulbar fat. The pterygopalatine process departs there, which goes medially to the fatty tissue of the temporopterygoid space and penetrates with its inner part into the pterygopalatine fossa. It surrounds the maxillary nerve and the adjacent pterygopalatine ganglion. Through the pterygoid process, the cellular spaces of the face are connected not only with the outer, but also with the inner base of the skull, since it often penetrates through the inferomedial part of the superior orbital fissure into the cranial cavity and is adjacent to the wall of the cavernous sinus. All three processes of the cheek fat pad are in most cases separated from its buccal portion by a permanent fascial process running from the lower edge of the zygomatic bone to the upper jaw above the attachment of the buccal muscle.
Thus, the fatty body of the cheek connects with each other the tissue of the buccal region, interpterygoid, temporopterygoid space, subgaleal tissue of the temporal region, pterygoid fossa, and sometimes retrobulbar tissue.
2. The main routes of infection penetration into the orbit, infraorbital, zygomatic, buccal areas; spread of infection from the above areas. In the infraorbital region there are facial muscles, each of which has its own loose fascial sheath. Between the muscles there are thin layers of fatty tissue that pass into one another without fascial barriers, so ulcers in this area can spread to the buccal and zygomatic areas, and along the angular vein - into the orbit.
Primary abscesses in the zygomatic region are almost never found, but it widely communicates with all surrounding cellular spaces, and purulent exudate can move unhindered in one direction or another (the infraorbital, temporal, buccal and parotid-masticatory areas are included in the process).
The infection penetrates into the cellular spaces of the orbit: 1) along the angular vein of the face in thrombophlebitis; 2) from the side of the maxillary cavity through the posterior porous wall into the pterygopalatine fossa, and from there through the inferior orbital fissure into the orbit; 3) the infection penetrates through the same routes with odontogenic phlegmon of the infratemporal and pterygopalatine fossae; 4) from the “canine” fossa along the inferoorbital canal. The infection can penetrate into the buccal area as a result of the spread of pus from the infratemporal, pterygopalatine and temporal fossae. The specified spread of infection is facilitated by the communication of the listed cellular spaces through the fatty lump of the cheek. Along these same fiber pathways, the purulent process can spread in the opposite direction.
3. Clinic, topical and differential diagnosis, treatment of patients with phlegmon of the orbit, infraorbital, zygomatic, buccal areas. Operative access and drainage of purulent foci.
Abscesses and phlegmons of the infraorbital region The clinical picture of an abscess in the infraorbital region, like all superficially located ulcers of the face, is characterized by the presence of large swelling, rapid involvement of the skin in the process and significant spontaneous pain associated with compression and irritation of the inferior orbital nerve.
The opening of the abscess of the infraorbital region is carried out along the transitional fold of the mucous membrane at the level of 1-2-3 teeth, however, unlike periosteotomy, it is recommended to go upward into the canine fossa using a blunt method (hemostatic clamp) and move the muscles apart. In addition, it must be borne in mind that conventional drainage with a rubber or cellophane strip is sometimes not enough, since the abscess cavity, despite drainage, constantly continues to fill with purulent exudate. This is due to the fact that the drainage strip is pinched by the contracted facial muscles. To achieve complete drainage, you can use a perforated narrow rubber tube, and sometimes you have to open the abscess through the skin.
Abscesses and phlegmons of the zygomatic region Primary abscesses in the zygomatic region are almost never found, but it widely communicates with all the surrounding cellular spaces, and purulent exudate can move unhindered in both directions. Therefore, when an abscess transforms into phlegmon, the infraorbital, temporal, buccal and parotid-masticatory areas are included in the process. If surgical opening of an abscess of the zygomatic region is performed along the lower edge of the greatest protrusion of the abscess from the skin, then opening of the phlegmon most often has to be done depending on the spread of the abscess to adjacent cellular spaces. The most rational method is a wide incision along the projection of the lower edge of the abscess from the skin side with the simultaneous application of a counter-aperture in the area of the emerging spread of the process.
Abscesses and phlegmons of the orbit There are no primary phlegmons of the orbital region of odontogenic etiology. The clinical course of orbital phlegmon is severe: high temperature, severe intoxication, painful headaches as a result of compression of the nerves and penetration of toxins through the opening of the optic nerve into the cranial cavity. Chemosis develops quickly, the eyelids swell, exophthalmos and diplopia appear. With a significant spread of the abscess, disturbances in the mobility of the eyeball occur, and pain on palpation increases. Surgical opening of the abscess is performed along the lower outer edge of the orbit. After opening the skin (along a natural fold of skin 2 - 3 mm from the edge of the eyelid to avoid subsequent lymphostasis, the length of the incision is 3 - 4 cm), the fibers and fascia are passed with a bluntly curved hemostatic clamp to the posterior surface of the eyeball, i.e. pus is obtained up to the retrobulbar tissue, adhering to the lateral bone wall, and a perforated drainage tube (or half-tube) is inserted. In severe cases, it is necessary to resort to drainage of the retrobulbar abscess through the maxillary cavity. In this case, trephination of the maxillary cavity is performed using a typical intraoral approach, removal of the upper bone wall in its distal section and opening of the periosteum and fascia of the orbital floor. Until the phlegmon of the orbit is cured, the maxillary cavity is left open for daily washing. After 10-15 days, the burr hole on the side of the oral cavity is sutured tightly, and further drainage of the maxillary sinus is carried out through the natural anastomosis in the middle meatus. Yu.N. Rostokin et al. (1984) proposed a new approach. An arcuate incision 4–5 cm long is made at the anterior edge of the temporal muscle at the site of its attachment to the squama of the temporal bone. Cutting through the soft tissue layer by layer, they reach the bone and, moving along the large wing of the main bone, penetrate to the lower orbital fissure, opening the purulent focus.
Abscesses and phlegmon of the buccal region Phlegmon of the buccal region is superficial with a predominant localization of infiltrate from the mucous membrane or from the skin of the cheek. Less commonly, damage to the fiber of both layers is observed with simultaneous suppuration of Bisha's lump. The configuration of the face is dramatically changed due to infiltration, swelling of the cheeks and adjacent tissues: swelling of the eyelids, lips, and sometimes in the submandibular region is observed. The skin of the cheek is shiny and does not wrinkle; the mucous membrane is hyperemic and edematous.
The choice of surgical access depends on the location of the infiltrate. The incision is made either from the side of the oral cavity, passing it along the line of closure of the teeth, taking into account the course of the duct of the parotid gland, or from the side of the skin, taking into account the course of the facial nerve. After the purulent exudate has been evacuated, drainage is introduced into the wound.
4. Complications of phlegmon of the orbit, infraorbital, zygomatic, buccal areas. Forecast. Medical aspects of rehabilitation of patients with odontogenic phlegmons of the orbit, infraorbital, zygomatic, buccal areas. Long-term compression of the optic nerve by infiltrated tissues of the orbit can lead to its atrophy, i.e. loss of vision. The prognosis (orbital phlegmon) is always serious. If panophthalmitis develops, consultation with an ophthalmologist for orbital exenteration is indicated. The prognosis for timely treatment of a patient with phlegmon of the infraorbital region is usually favorable, but with the development of thrombophlebitis it is assessed as very serious.
Classification of the disease
Phlegmon of the upper jaw
Cellulitis of the jaw can be acute or chronic. In acute cases, the infectious process develops rapidly, pus begins to be released, and tissue necrosis develops. The temperature rises to 40 degrees, the seal on the skin pulsates, becomes hot, and the skin becomes glossy. When the formation softens, fistulas form.
In the chronic form, the neoplasm is bluish in color and dense. When palpated, severe pain occurs.
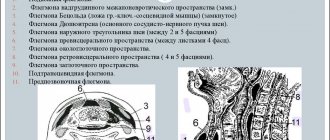
Classification according to topographic-anatomical principle:
- Phlegmon of the upper jaw. The infectious process covers the hard and soft palate, temporal, infratemporal, and infraorbital areas. It passes to the pterygopalatine fossa, zygomatic and orbital zone.
- Located near the lower jaw. The pathological process extends to the chin, buccal, and submandibular areas. Affects the salivary glands.
Odontogenic phlegmon - the infection penetrates into the soft tissue through damaged teeth and marginal periodontium. Osteogenic neoplasms are a consequence of odontogenic osteomyelitis.
According to localization, subcutaneous, subfascial, intermuscular, and interfascial formations are distinguished. By location – superficial and deep tumors. The nature of the inflammatory effusion is serous, purulent, putrid-necrotic.
Soft phlegmon is characterized by the absence of visible foci of tissue necrosis. Hard cellulitis has areas of rejection of dead tissue.
Opening an abscess, phlegmon of the maxillofacial area
The frequency of development of abscesses and phlegmon of the maxillofacial area of the head is due to the high prevalence of chronic focal odontogenic and tonsillogenic infections, as well as infectious and inflammatory lesions of the skin and oral mucosa. Based on data on the localization of the infectious-inflammatory process in various anatomical sections, zones, regions, as well as spaces of the head and neck, their systematization is built. From the description of the topographic-anatomical structure of the areas of the face, the perimandibular and adjacent areas of the neck, one can see the complexity of their anatomy. There are many cellular spaces, numerous lymph nodes and vessels scattered throughout all areas of the face, an abundant network of arteries and veins with rich innervation of these areas.
The basic principle of treating inflammatory diseases is opening the source of inflammation and draining it. Complete drainage reduces pain, promotes the outflow of wound fluid, improves local microcirculation, which naturally has a beneficial effect on local metabolic processes, the transition of the wound process to the regeneration phase, reducing intoxication and interstitial pressure, limiting the necrosis zone and creating unfavorable conditions for the development of microflora.
The incisional drainage method of treating phlegmons and soft tissue abscesses is quite widespread to this day. It involves opening a purulent focus and open wound management in the postoperative period. The incisional drainage method is a classic one; in general, it determines the tactics for the treatment of acute purulent diseases of soft tissues and purulent wounds.
Opening of the purulent focus is carried out by external access from the skin, or intraoral access from the mucous membrane.
During the operation of opening an abscess (phlegmon), the skin, mucous membrane, and fascial formations above the purulent focus are dissected; the muscles are cut off, peeled off from the place of attachment to the bone of the temporal, medial pterygoid and chewing muscles (m. temporalis, i.e. pterygoideus mcdialis, i.e. masseter) or using a hemostatic clamp, the muscle fibers of the temporal, mylohyoid and buccal muscles (m. temporalis) are pulled apart , T. mylohyoideus, T. buccalis). The exception is the subcutaneous muscle of the neck (m. platysma) and often the mylohyoid muscle, the fibers of which intersect in the transverse direction. which ensures the wound gapes and creates good conditions for the outflow of purulent exudate. Loose tissue located on the way to the purulent focus, in order to avoid damage to the vessels, nerves, and excretory flow of the salivary glands located in it, is stratified and pulled apart with a hemostatic clamp.
Diagnostic methods
Before treatment, an abscess must be differentiated from other diseases of the jaw.
If signs of phlegmon appear, you should contact your dentist. The doctor will conduct an examination, collect anamnesis, prescribe tests and necessary studies.
Diagnostic measures:
- General blood analysis. During a severe inflammatory process, the leukocyte number shifts towards young cell forms, and the ESR increases.
- Blood chemistry. Specific markers of the inflammatory process appear, enzymes that are formed during tissue breakdown.
- Bacteriological analysis of purulent contents to identify the type of pathogen and assess sensitivity to antibiotics.
- Ultrasound, CT.
It is imperative to carry out a differential diagnosis of phlegmon from osteomyelitis, cysts, abscess, and other dental or systemic diseases.
Phlegmon of the peripharyngeal space - presentation
The presentation was made by a student of the 9th group of the 5th year of the Faculty of Dentistry Lokshin Sergeevich Moscow 2020 Phlegmon of the peripharyngeal space
A purulent process in the peripharyngeal space can occur as a complication of acute, less often chronic, tonsillitis. Odontogenic sources of infection in this space are large molars of the lower and sometimes upper jaw. Often the peripharyngeal space is affected when infection spreads from under the mandibular triangle, sublingual, retromandibular areas, as well as the pterygomandibular space.
Periopharyngeal space
Boundaries of the peripharyngeal space: inner muscular layer of the pharynx; external medial pterygoid muscle and deep pharyngeal part of the parotid salivary gland; anterior interpterygoid fascia and inner surface of the medial pterygoid muscle; posterior lateral fascial processes running from the prevertebral fascia to the muscular layer of the pharynx.
The styloglossus, stylopharyngeal, stylohyoid and surrounding fascia muscles divide the peripharyngeal space into anterior and posterior sections. In the anterior section of the peripharyngeal space there is loose and fatty tissue, in its upper section the pterygoid venous plexus is adjacent. In the posterior part of the space there are the internal carotid artery, internal jugular vein, IX, X, XI, XII cranial nerves, and lymph nodes. In addition, in some patients the superior cervical sympathetic ganglion is located here. The fiber located in the peripharyngeal space communicates with the fiber of the pterygopalatine fossa and the temporal, sublingual regions, and submandibular triangle.
Clinic of phlegmon of the peripharyngeal space Pain when swallowing, often difficulty breathing, deterioration in general health, the appearance of chills and other symptoms of intoxication. At the angle of the lower jaw there is a deep infiltrate that is painful on palpation. In some patients, swelling occurs in the temporal region. Mouth opening is limited due to grade III inflammatory contracture of the medial pterygoid muscle. Examination of the oral cavity is difficult. A wide spatula is inserted between the teeth of the upper and lower jaws and, turning it, the pharynx is examined. The mucous membrane of the pterygomandibular fold and soft palate is hyperemic and edematous, the uvula is sharply shifted to the healthy side. The infiltrate spreads to the side wall of the pharynx, which bulges significantly, swelling to the mucous membrane of the sublingual fold, tongue, and posterior wall of the pharynx. When diagnosing phlegmon of the peripharyngeal space, it should be taken into account that the process often develops when infection spreads from the submandibular triangle. If there is a restriction in mouth opening or an increase in pain when swallowing, the oral cavity and pharynx should be carefully examined.
Diagnostics It is necessary to differentiate parapharyngeal phlegmon, first of all, from purulent-inflammatory processes of the pterygo-maxillary space and peritonsillitis. You should also keep in mind phlegmonous tonsillitis. Any of these diseases can cause diffuse swelling, spreading to the peripharyngeal space and adjacent areas of soft tissue, especially the soft palate. The anatomical and topographic differentiation of the closely spaced slit-like spaces is illustrated.
Diagnosis Anamnesis of the disease, in particular the source of infection, is essential for differential diagnosis. Odontogenic infection in most cases causes damage to the pterygomaxillary space, and tonsillitis causes peritonsillitis. Complete reduction of the jaws, trismus of the third degree, indicates the localization of the process in the pterygo-maxillary space. If it is possible to perform a palpation examination, then the localization of the abscess is established more accurately.
Treatment Treatment comes down to opening the abscess. Due to the anatomical features of the posterior part of the parapharyngeal space, which contains large vessels and nerves, the depth of the intramural incision should not exceed 0.75 cm; further deepening into the tissue should be done bluntly. As a precaution, it is better to wrap the scalpel blade in cotton wool, leaving the end free within 0.75 cm. This is all the more appropriate since it is necessary to operate without sufficient anesthesia and a sudden, sharp movement of the patient can lead to unexpected injury to neighboring tissues. With the rapid development of the phlegmonous process and the low effectiveness of the incision from the oral cavity, it is necessary to urgently resort to an external incision. This path is next. Through a skin incision at the angle of the lower jaw, they penetrate to the medial surface of the internal pterygoid muscle and from here, in a blunt way, adhering to the named muscle, they easily reach the source of phlegmon. Having received pus, the wound is drained. If there are no special contraindications, it is useful, along with surgical intervention, to use heat in the form of inhalations or rinses. At the first signs of an inflammatory process in the parapharyngeal space, treatment with penicillin and other antibiotics is used, continuing it after surgical opening of the purulent focus until a favorable outcome occurs.
The main stages of the operation of opening phlegmon of the peripharyngeal space using the submandibular approach.
Drug and physiotherapeutic treatment
Cellulitis of the lower jaw is treated surgically
Treatment methods for phlegmon are determined taking into account the stage of inflammation. At the initial stages of the disease, it is enough to undergo a course of antibacterial therapy. It is imperative to identify and treat diseased teeth or carry out extractions and eliminate dental pathologies.
Medications:
- broad-spectrum antibiotics, take every 3-4 hours, how much medication you need to take, your doctor will tell you;
- rinsing the mouth with sulfonamide preparations, Sollux, Furacilin - procedures should be carried out only with the help of a rubber bulb;
- non-steroidal anti-inflammatory drugs;
- antihistamines;
- streptococcal toxoid;
- detoxification agents;
- analgesics, injections with 1-2% Promedol solution.
- vitamin complexes, adaptogens.
Additionally, it is necessary to consume more plant foods, dairy and fermented milk products. Food should be liquid and high in calories. You should take good care of your oral cavity.
For phlegmon, oxygen therapy is prescribed to relieve pain and prevent the spread of the purulent process to healthy tissue. Effective physiotherapy - UHF, phonophoresis with Dimexide, laser therapy.
Traditional methods
Saline mouth rinse for sore gums
Cellulitis is a disease that cannot be treated at home. Consultation and constant monitoring by a doctor is required. Traditional methods can be used to speed up the recovery process.
Recipes:
- Pour 1 tbsp. l. clove buds 200 ml of water, simmer over low heat for 3 minutes after boiling. Leave in a sealed container for an hour, strain. Make lotions with the solution on the affected areas or take 30 ml orally 3-4 times a day.
- Mix 50 g of St. John's wort and 25 g of propolis, chop, pour in 150 ml of vodka. Place in a dark place for 14 days, strain. Rinse your mouth with tincture 4-5 times a day.
- Boil 10 g of birch buds in 200 ml of water for 20 minutes. Use the strained broth for compresses or take 1 tbsp orally. l. 4 times a day.
With submandibular phlegmon, any warming procedures are prohibited. Under the influence of heat, pathogenic microorganisms actively multiply, an abscess may open, and the local pathological process will spread to healthy tissue.
Method of operation for opening phlegmon of the axillary space of the temporal region
With phlegmon of the axillary space (Fig. 22, A):
1. Anesthesia - anesthesia or local infiltration anesthesia accompanied by premedication.
2. An arcuate skin incision above the upper line of attachment of the temporal muscle to the temporal bone (Fig. 22, B).
3. Using a hook, pull the lower edge of the wound down, isolate, bandage and cross the large branches of a. et v. temporalis superficialis (Fig. 22, C, D).
4. Cross the temporal aponeurosis and temporalis muscle along lin. temporalis superior (Fig. 22, D).
5. Peeling off the temporal muscle from the place of its attachment to the temporal bone with a raspatory, they enter the axillary tissue space, open the purulent-inflammatory focus, and evacuate the pus (Fig. 22, E).
6. A tubular drainage is inserted into the axillary tissue space, allowing for washing, irrigating the wound with antibiotics, enzymes, and performing vacuum drainage (Fig. 22, G).
7. Aseptic cotton-gauze bandage with hypertonic solution, antiseptics.
Did you like the article? Share with friends
0
Similar articles
Next articles
- Abscess, phlegmon of the eyelids
- Abscess, phlegmon of the infraorbital region
- Abscess, phlegmon of the mouth area
- Abscess, phlegmon of the nose area
- Abscess, phlegmon of the chin area
Previous articles
- Abscess, phlegmon of the middle vault
- Methods of conduction anesthesia in the head and neck area
- Treatment planning for patients with acute odontogenic infection, taking into account the prognosis of the disease
- Principles of surgical treatment of patients with abscesses, phlegmon of the head and neck
- Topical diagnosis of abscesses, phlegmons of the head and neck
Surgery
After surgery, the doctor prescribes antibiotics
Surgical intervention is necessary in advanced stages of phlegmon, when foci of necrosis are present. During the operation, the abscess is opened and cleansed, and the surrounding areas are sanitized. Local or general anesthesia is used.
Typical incisions for adenophlegmon of the submandibular triangle should be made along the natural folds. Be sure to take into account the cosmetic contours of the face, the location of the facial nerves, arteries, and vessels.
Operation stages:
- Using a scalpel or electric scalpel, the mucous membrane, skin and underlying tissue are cut down to the fascia.
- Fabrics delaminate.
- In case of putrefactive-necrotic lesion, necrectomy is performed - dead tissue is excised.
- They drain the wound - install tubes, rubber strips or a catheter. The wound is washed.
- The edges of the wound are sutured and a sterile bandage is applied.
After the operation, bandages are applied 1-2 times a day and the wound is cleaned. After eliminating the signs of the inflammatory process and reducing the temperature to subfebrile levels, primary delayed or secondary sutures are applied. The rehabilitation period is 1-2 months. After discharge from the hospital, you must follow all doctor's recommendations.
Sometimes plastic surgery is required after surgical treatment. Indications: changes in the shape and size of the tissues of the face and neck that cannot be eliminated by other methods.
Phlegmon of the submandibular triangle
Phlegmonous inflammation in the submandibular triangle is more common than in other perimandibular spaces. In accordance with the anatomical and topographical features of this area, the process occurs here either in the form of adenophlegmon, or as a diffuse purulent lesion of the tissue.
Topographic anatomy. In the center of the submandibular triangle is the submandibular salivary gland with adjacent regional lymph nodes and the external maxillary artery and anterior facial vein passing here. The anatomical boundaries of the triangle are expressed quite clearly. Its outer border is the lower edge of the body of the lower jaw, the other two sides are represented by the anterior and posterior bellies of m. digastrici. On top, the triangular space is covered with the mylohyoid muscle; below, the following are located in layers: skin, subcutaneous tissue with m. platysma and the superficial layer of the cervical fascia.
The submandibular bed itself with the salivary gland and lymph nodes and vessels enclosed in it (a. maxillaris externa, v. facialis anterior) is limited from below by the superficial layer of the own fascia of the neck, going from the body and large horn of the hyoid bone to the edge of the lower jaw, and from above - by another its leaf, integral with the fascia that covers the mylohyoid and hyoglossus muscles (m. mylohyoideus m. hyoglossus). The salivary gland is separated from the lymph nodes by its own capsule.
Through the gap between the posterior edge of the mylohyoid and mylohyoid muscles, the submandibular triangle communicates with the sublingual region (with the maxilloglossal groove). The duct of the submandibular salivary gland, and sometimes part of the submandibular salivary gland itself, penetrates this gap. In front, the submandibular triangular space is adjacent to the submental region. Posteriorly it communicates with the peripharyngeal space. Along the way a. maxillaris externa and v. facialis anterior, the submandibular triangular space connects with the carotid space of the neck. In the circumference of the submandibular salivary gland there is a significant amount of loose connective tissue.
Clinic. The process begins with the appearance of a painful swelling in the submandibular triangle and often pain when swallowing. In some cases, the disease develops rapidly, in others all phenomena increase gradually or the process proceeds, sometimes intensifying, sometimes subsiding somewhat.
A dense, painful infiltrate appears in the depths of the submandibular triangle. The skin in the area of the triangle first loosely gathers into a fold, and then becomes more and more tense, turns red, and becomes pasty. Due to significant collateral edema, neighboring areas swell (Fig. 128). The face becomes asymmetrical. In the neck, swelling sometimes goes down to the collarbone and below. The submandibular and a significant part of the cervical lymph nodes increase in volume, their palpation is painful. The pain intensifies. Movement of the lower jaw is also painful. Trismus in some cases is barely pronounced, in others it reaches II-III degree. The latter is observed when the area of the maxillo-lingual groove is involved in the process.
On the part of the oral cavity, with phlegmon of the submandibular triangular space, there is usually only barely noticeable swelling and hyperemia of the mucous membrane of the sublingual region of the corresponding side, sometimes these phenomena are more pronounced, especially when the starting point of the purulent process in the area of the submandibular triangle is an abscess of the maxillo-lingual groove.
Adenophlegmon of the submandibular triangle is more characterized by slow development with gradually increasing and sometimes even subsiding pain, especially under the influence of treatment. Trismus with adenophlegmon is usually mild.
At the height of the development of phlegmon, the general condition of the patient is depressed. Sleep and appetite are disturbed. The temperature stays between 38-39°. After 3-5 days, a fluctuation is detected above the focus of pus accumulation. With adenophlegmon, fluctuation is more difficult to determine. Self-opening of phlegmon is delayed indefinitely with the risk of breakthrough into deeper areas.
Phlegmon can spread to the floor of the mouth, neck, parapharyngeal space and be complicated by thrombosis of the anterior facial and internal jugular vein system, lead to general sepsis or result in purulent mediastinitis with a fatal outcome.
In most cases, phlegmon of the submandibular triangle occurs as a result of odontogenic infection; This also includes difficult eruption of the lower wisdom tooth.
Often phlegmon accompanies osteomyelitis of the lower jaw.
Due to the fact that the submandibular lymph nodes are regional, infection is possible not only from nearby areas (teeth, periodontium), but also from distant ones (nose, lips, tongue, tonsils). As a result, adenophlegmons may develop.
Treatment. Surgical intervention for adenophlegmon is reduced to opening the bed of the submandibular salivary gland and the lymph nodes of the submandibular triangle. An incision is made into the skin and subcutaneous tissue, the subcutaneous muscle of the neck, dissection of the fascial sheet, and opening of the capsule of the affected gland. But such sequential, layer-by-layer incisions are possible only in the earliest, initial stages of phlegmon. When the purulent infiltrate reaches the subcutaneous muscle of the neck, the path of surgical intervention is determined by the focus of tissue softening and fluctuation.
The skin incision is made 1-2 cm below the edge of the lower jaw, so as not to damage the marginal branch of the facial nerve (ramus marginalis p. facialis). The length of the incision is on average 4-6 cm. If there is insufficient emptying of pus, the adjacent areas of the anterior and posterior poles of the submandibular salivary gland are examined with a finger.
For phlegmon developing in the cellular space of the submandibular triangle without purulent lesions of the lymph nodes, the direction and dimensions of the incision are the same as for adenophlegmon.
The changed outline of the submandibular triangle due to swelling of the infiltrated tissues makes it difficult to correctly select the incision site. In such cases, the guideline for making the cut is the line connecting the point on the border of the middle and upper third of the length m. sternocleidomastoideus with the upper edge of the thyroid cartilage.
You should remember about the possibility of injury to the external maxillary artery and anterior facial vein; however, for fear of damaging them, one should not refuse radical intervention. Stopping the resulting bleeding in heavily infiltrated tissues presents some difficulties, but this is quite surmountable.
Prognosis and prevention
If not treated promptly, swelling of the throat and death may occur.
In advanced cases, severe complications develop against the background of phlegmon - meningitis, sepsis. Pathologies can lead to disability or death. When the respiratory tract is affected, asphyxia develops, the person begins to choke due to swelling of the throat. Other complications are phlebitis of facial vessels, mediastinitis.
If treatment is started in a timely manner, the prognosis is favorable. In order to detect phlegmon in time, you need to visit the dentist every six months, and, if necessary, a dental technician.
Cellulitis in the maxillofacial area is a serious and dangerous disease due to the anatomical and functional characteristics of this area. Therefore, their treatment requires immediate hospitalization.
Abscess of the pterygomaxillary space
Abscess and phlegmon of the pterygomaxillary space
Relatively often, the cause of purulent lesions in this space is inflammatory processes in the area of the lower molars. Much less frequently, inflammatory diseases of the pterygomaxillary space and its upper section arise as a result of the spread of pus from the area of the upper molars. Sometimes the purulent process penetrates into the pterygo-maxillary space with an abscess of the posterior part of the sublingual region (from the maxillo-lingual groove), as well as with progressive phlegmon of the sublingual region, submandibular triangle, and floor of the mouth.
The pterygomaxillary space is limited externally by the ramus of the mandible, internally by the medial pterygoid muscle, superiorly by the lateral pterygoid muscle, and anteriorly by the buccal muscle attached to the hapbe pterygomandibularis. At the back, this space is partially covered by the parotid salivary gland.
The loose fiber that fills the pterygomaxillary space communicates in various places with the adjacent fiber spaces: through a gap along the posterior edge of the medial pterygoid muscle - with the retromandibular (posterior mandibular) and anterior sections of the peripharyngeal space, at the top - with the temporal, infratemporal and pterygopalatine fossae, at the bottom - with the submandibular region. Anteriorly, a fatty lump of the cheek penetrates into the upper section of the pterygomaxillary space, in the space between the upper jaw and the anterior edge of the lower jaw branch.
The picture of the disease during a purulent inflammatory process localized in the pterygomaxillary space is different depending on the rate of increase of inflammatory phenomena in the volume of tissues involved in the process. Sometimes, especially with an abscess, all phenomena develop slowly and gradually, over many days, limited to the pterygo-maxillary space. Often, within 2-3 days, the purulent process not only spreads throughout the entire tissue of this space, but also penetrates into neighboring areas.
Abscess of the hard palate
Local signs of a developing disease are progressive limitation of mouth opening, increasing pain when swallowing, enlargement and tenderness of the lymph nodes at the angle of the lower jaw. In subsequent
days, along with the increase in the listed phenomena, slight swelling and painful infiltration appear at the angle of the lower jaw. The lymph nodes located here seem to be fused with each other and the surrounding tissues and can be palpated less clearly. Swelling may also appear in the lower temporal region.
When the process is sluggish (and this sometimes happens as a result of prolonged use of antibiotics), the purulent focus seems to descend downward; in this case, we had to observe the appearance of a limited area of soft tissue softening at the angle of the lower jaw or slightly inward from it.
In the vestibule of the mouth, no changes are detected during inflammatory processes in the pterygomaxillary space. After slowly retracting the lower jaw with the instrument, it is possible to examine, often only with the help of a frontal reflector, the posterior parts of the oral cavity. There is hyperemia and swelling of the mucous membrane in the area of the pterygomandibular fold (plica pteriygomandibularis), as well as the anterior arch of the soft palate.
Surgical intervention for purulent inflammatory diseases of the pterygomaxillary space is carried out from the mouth or through the skin. The first way does not allow wide opening of the pterygomaxillary space and is indicated only for slowly developing limited purulent foci. An incision about 2 cm long is made parallel to the pterygomaxillary fold, slightly outward from it, through the mucous membrane, penetrating with a scalpel to a depth of 0.5-0.75 cm. If pus does not appear, then a grooved probe is inserted into the incision and, penetrating they are used to push the tissues apart into the pterygomaxillary space (adhering to the same direction as during conduction anesthesia at the mandibular foramen), revealing the purulent focus.
For phlegmon of the pterygo-maxillary space, especially in cases of rapid development of the disease, an incision is shown from the outside, in the area of the angle of the lower jaw, as with phlegmon of the parotid-masticatory region, but, having reached the bones in the area of the angle and base of the lower jaw with a scalpel, the lower part of the medial pterygoid is separated muscles from the bone and bluntly penetrate upward onto the inner surface of the branch of the lower jaw to the area where pus accumulates.