Features of phlegmon, methods of its treatment and prevention
Cellulitis is a purulent inflammation of soft tissues, characterized by a fairly rapid spread in the area of muscles, tendons and fiber, as well as their impregnation with exudate. Phlegmon is characterized by localization in any part of the body, and in an advanced form, internal organs can be affected.
Staphylococci, streptococci, Pseudomonas aeruginosa can play the role of the main causative agents of purulent phlegmon of the neck, face, hand or other part of the body. Obligate anaerobes, which actively reproduce in conditions of complete absence of oxygen, can cause the development of a severe form of the disease.
Reasons for development
Cellulitis develops when pathogenic microflora penetrates the cellulose. The causative agents are most often staphylococci, streptococci, Proteus, Pseudomonas aeruginosa, Enterobacteriaceae, and Escherichia coli.
First, serous infiltration of the tissue occurs, then the exudate becomes purulent. Foci of necrosis appear, merging with each other, thereby forming large areas of tissue necrosis. These areas are also subject to purulent infiltration. The purulent-necrotic process spreads to adjacent tissues and organs. Changes in tissues depend on the pathogen. Thus, anaerobic infection entails tissue necrosis with the appearance of gas bubbles, and coccal pathogens result in purulent melting of tissue.
Microorganisms invade fatty tissue through contact or hematogenous routes. Among the most common causes of phlegmon are:
- Soft tissue injuries;
- Purulent diseases (boils, carbuncles, osteomyelitis);
- Violation of antiseptics during medical procedures (injections, punctures).
What is the difference between cellulitis and abscess
Inflammatory processes with the release of pus in tissues that are locked in a certain place under the skin are called abscesses. Non-localized inflammations with pus that appear under the skin - phlegmon. Have you heard about cellulite? When it is mentioned, they mean serous inflamed processes of fatty tissue, but without pus.
If these diseases cannot be distinguished, a puncture is used for diagnostic purposes, pus and tissue are taken. Bacteriological analysis will help determine the pathogen and its resistance to antibiotics. We have determined that phlegmon and abscesses are similar but different diseases.
The main cause of phlegmon is the division of pathogenic organisms. Staphylococci, streptococci, Pseudomonas aeruginosa, Escherichia coli and this is not the whole list.
Diffuse swelling of the neck appears only at the second stage of development. The infection settles in other organs. It then spreads through the blood into soft tissues. The cause of development is Staphylococcus aureus.
More precise reasons for the development:
- Dental disease in the lower jaw, along with a developed inflammatory process. For example, pulpitis, caries, gum inflammation, periodontitis.
- Infections of the respiratory tract and organs, inflammation in the throat and trachea. Especially when such inflammations become chronic, their treatment will require frequent use of antibiotics. The body will not be able to fight off the bacteria and it may end up in the neck.
- Inflammation of the lymph nodes in the neck.
- Various wounds on the neck, possibly boils, can be the cause.
- Common infectious diseases. The infection is transmitted through the blood to the neck.
- Purulent inflammation can descend from the oral cavity down the neck.
The beginnings, which as a result can turn into phlegmon on the neck - ulcers on the face or inflammation in the mouth, upper respiratory tract, osteomyelitis of the cervical vertebrae, wounds on the neck.
The appearance of tumors in the neck is determined by the following factors:
- The network of lymph nodes is well developed;
- Individual features of the structure of the cervical fascia.
Swelling of the lower jaw and chin forms on the neck. The tumor is initially dense and later acquires a lumpy appearance.
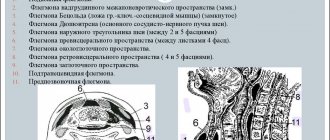
Types and locations of phlegmon
Taking into account the classification of phlegmon by anatomical location, the following types of pathology can be particularly distinguished:
- Serous – the initial form of phlegmonous inflammation. It is characterized by the formation of inflammatory exudate, as well as intensive attraction of leukocytes to the pathological focus. At this stage, a palpable infiltrate appears, as the fiber is saturated with a turbid gelatinous liquid. There is no clearly defined boundary between healthy and inflamed tissues. In the absence of timely prescribed treatment, a rapid transition to a purulent or putrefactive form is observed. The development of one form or another is associated with causative microorganisms that entered the entrance gate
- Putrefactive - caused by anaerobic microorganisms that emit certain unpleasant odors during their life processes. The affected tissues are brown or green in color, disintegrate into a gelatinous mass and emit a foul odor. This creates conditions for the rapid penetration of toxic substances into the systemic bloodstream with the development of severe intoxication, leading to failure of many organs.
- Purulent - pathogenic microorganisms and enzymes released from phagocytes lead to the digestion of tissues and their necrosis, as well as purulent secretion. The latter represents dead leukocytes and bacteria, and therefore has a yellowish-green color. Clinically, this form corresponds to the appearance of cavities, erosions and ulcers, which are covered with purulent plaque. With a sharp decrease in a person’s immune forces, the phlegmonous process spreads to muscles and bones with their subsequent destruction. The main diagnostic sign at this stage is the absence of muscle bleeding upon slight scraping.
- Anaerobic. In this case, according to the morphological characteristics, the process is serous in nature, but gas bubbles are released from the places of necrosis. Due to their presence in the tissues, a characteristic sign appears - mild crepitus. Hyperemia of the skin is slightly expressed, and the muscles have a “cooked” appearance.
- Necrotic. It is characterized by the appearance of dead areas that are clearly demarcated from healthy tissue. The border between them is a leukocyte shaft, from which a granulation barrier is subsequently formed, while necrotic areas can melt or be rejected. Such delimitation leads to the formation of abscesses that are prone to spontaneous opening.
The area where phlegmon occurs may vary. However, as practice shows, the following parts of the body are most often affected by this type of purulent lesion of fatty tissue (phlegmon):
- breast;
- hips;
- buttocks;
- back (especially its lower part);
- sometimes - the face and neck area.
Also, depending on the location of phlegmon, it is divided into the following types:
- Subfascial.
- Subcutaneous, which progresses directly into the subcutaneous fat layer.
- Intermuscular, which is usually accompanied by ongoing or progressive inflammatory processes in the muscle layer.
- Perirenal, accompanied or caused by kidney diseases - this is how pathogenic microflora penetrates into this area.
- Retroperitoneal (phlegmon of the retroperitoneal space), detected by conducting a general examination of the abdominal cavity when the patient frequently complains of pain in the abdominal area.
- Pararectal, located near the rectum and its origin is due to the penetration of pathogenic microorganisms through the walls of the rectum. The most common cause of phlegmon in this case is long-term constipation and intestinal instability.
Since the main reason for the appearance of phlegmon should be considered the penetration of pathogenic microorganisms into the tissues of adipose tissue, breaks and cracks in the skin, these places require special attention in case of any mechanical damage.
Diagnosis of phlegmon
For a qualified specialist, making a diagnosis in the case of damage to subcutaneous fat tissue usually does not present any difficulty. Usually, an examination with palpation is sufficient for this, during which the doctor detects the absence of clearly defined boundaries and a purulent core.
Diagnosing phlegmon that affects the walls of the abdominal cavity and internal organs can be somewhat difficult. In this case, various instrumental and laboratory tests are carried out, for which the patient is referred by the attending physician.
Symptoms
Phlegmon in acute forms develops quickly. Patients experience a significant increase in temperature above 40°C, which is accompanied by chills, headaches, thirst and dry mouth. Against the background of general intoxication, weakness and drowsiness are observed. Nausea and vomiting often occur. Blood pressure is increased, heart rhythms are disturbed. The number of urinations in the patient is reduced until they stop completely.
A lump with swelling appears on the affected area, it feels hot to the touch, and the skin becomes shiny. It is not possible to define clear boundaries of education. There is significant pain in this area, the lymph nodes located near the source of inflammation are enlarged. With the further development of the disease, the compacted areas tend to soften, forming purulent cavities, the filling of which sometimes independently breaks out through the fistula or spreads further through neighboring tissues, provoking further inflammation and the process of destruction.
The symptoms of deep phlegmon are more pronounced and appear in the early stages.
Treatment
At the first symptoms of phlegmon formation, you should immediately contact a surgeon or otolaryngologist. If respiratory problems develop, it is necessary to urgently call an ambulance, as there is a threat to life. Under no circumstances should you try to cure this disease on your own; the purulent process can spread to neighboring tissues so quickly that delay significantly reduces the chances of recovery.
Drug therapy
Exclusively medicinal treatment of phlegmon is usually prescribed in the early stages of the disease.
Meronem is a powerful antibacterial drug active against most microorganisms
During the entire period, it is necessary to take broad-spectrum antibiotics. The approximate time for using medications is 5–10 days. If after the expiration of the period no positive dynamics are observed, the drug is replaced.
The patient is also prescribed immunomodulators and medications to eliminate intoxication. Plenty of fluids are used and droppers can be placed to cleanse the blood (glucose, saline solutions).
Special enzyme preparations can limit the area of inflammation, restore blood circulation, improve metabolism, enhance the effect of antibiotics and eliminate bacterial waste products.
In case of blood poisoning, the following measures are prescribed:
- plasmapheresis, which consists in removing plasma from the bloodstream and purifying it of harmful substances;
- hemosorption is a disinfection method in which blood is removed from the vascular bed, cleaned by filters and returned back;
- Lymphosorption is a similar procedure, but it cleanses the lymph.
Blood purification is extremely important, as the infection often spreads throughout the body
Surgical intervention
Usually phlegmon is treated surgically. The surgeon determines the area where incisions of different sizes will be made. Pus is removed from the affected area, and surrounding tissues are cleaned. Subsequently, drainages can be installed for the unimpeded outflow of pathological discharge from the wound.
The operation is carried out with extreme caution, as there is a high risk of damage to blood vessels, nerves and other vital anatomical structures of the neck.
Elimination of phlegmon in the sublingual area
Folk remedies
Herbal remedies cannot replace surgical and drug treatment. Attempting to cope with the disease on your own will lead to a worsening of the condition. Most often, folk recipes can be used as an additional method of treatment during the recovery period and only with the approval of a doctor.
Tincture of propolis and St. John's wort
Propolis is famous for its anti-inflammatory properties and is often used for various infectious diseases.
- Grind three tablespoons of propolis and five tablespoons of St. John's wort.
- Add 150–200 ml of alcohol or vodka.
- Place the resulting mixture in a glass bottle, close it tightly and place it in a dark place for a week.
- Shake the tincture periodically.
- Strain, mix 50 drops with a glass of water.
- Rinse your mouth five times a day.
St. John's wort is useful for inflammatory processes
Clove compresses
Cloves have an antimicrobial, disinfectant and even anthelmintic effect.
- Pour three tablespoons of chopped cloves into a liter of boiling water.
- Leave to infuse for one hour.
- Strain, blot the cotton wool and apply to the inflamed area once or twice a day.
Cellulitis of the neck
Abscesses and phlegmons of the neck are classified as diseases whose course is unpredictable, and the consequences can be very severe and even life-threatening for the patient. In most cases, the source of pathogenic infection in phlegmon of the neck is inflammatory processes in the oral cavity and pharynx - pharyngitis, laryngitis, chronic dental caries and similar diseases.
Superficial abscesses and phlegmons of the neck most often arise above the deep cervical fascia and therefore they do not pose any particular danger, since they are easily accessible for surgical opening. Most neck phlegmons are localized in the chin and submandibular areas. The clinical picture for this type of phlegmon is as follows: the general temperature rises to 39 degrees Celsius, the patient experiences severe headaches, general weakness and malaise.
A laboratory blood test indicates an increased level of white blood cells. In the absence of timely treatment, phlegmon progresses and inflammation spreads to large veins of the facial area, and there is also a risk of purulent meningitis.
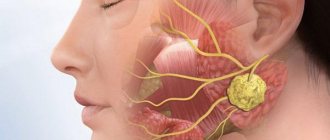
Characteristic local signs of abscesses and phlegmon of the buccal area
Superficial cellular space (between the skin and the buccal muscle) (Fig. 48, A):
Complaints of pain in the cheek area of moderate intensity, intensifying when opening the mouth and chewing.
Objectively. Sharply expressed facial asymmetry due to inflammatory infiltration of cheek tissue. The skin is tense and hyperemic. Palpation causes pain, fluctuation can be detected.
Deep cellular space (between the mucous membrane of the cheek and the buccal muscle (Fig. 48, B):
Complaints of pain in the cheek area of moderate intensity.
Objectively. Asymmetry of the face due to swelling of the cheeks. Her skin is of normal color. When examined from the oral cavity, swelling of the cheek is revealed due to infiltration, the mucous membrane above which is tense and hyperemic. Palpation causes pain. Sometimes fluctuation can be detected, and when the inflammatory process spreads to the anterior edge of the masticatory muscle (m. masseter), there may be some limitation in mouth opening.
Phlegmon of the hand
Occurs in the deep subcutaneous areas of the hand. As a rule, inflammation occurs as a result of purulent infection through scratches, wounds and cuts. There are the following subtypes of phlegmon of the hand: on the middle palmar area, on the eminence of the thumb and phlegmon in the form of a cufflink. Phlegmon of the hand can form anywhere in the hand space with subsequent spread to the back of the hand. The patient feels severe throbbing pain, the tissue of the hand swells significantly.
Why does phlegmon appear - the causes of the problem
Periandibular phlegmon is a serious complication that occurs due to the spread of infection in the tissues of the oral cavity. Most often, the following pathological phenomena are the prerequisites for the formation of a purulent neoplasm:
- periodontitis,
- cyst,
- flux,
- periodontitis,
- osteomyelitis.
Phlegmon is a purulent inflammation of the soft tissues of the jaw.
Often, submandibular phlegmon forms in the area of molars and wisdom teeth. Sometimes such a nuisance results from injury to the sublingual area or skin pathologies, such as stomatitis, boils, or pustular rash. But the most important problem is bacteria - staphylococci and streptococci. They are the ones who provoke the outflow of lymph and venous blood from the deep layers of the skin. More often, phlegmon appears against a background of weakened immunity, diabetes, or exacerbation of allergies. In young children (under 6 years old), the cause of such a diagnosis may be Haemophilus influenzae bacteria1.
Facial phlegmon
This is a rather severe subtype of the disease, occurring mainly in the temporal region, near the jaw and under the masticatory muscles. With facial phlegmon, the patient experiences severe tachycardia and an increase in body temperature of up to 40 degrees, facial tissues swell greatly, and chewing and swallowing functions are impaired.
Patients with suspected facial phlegmon should be immediately hospitalized in a specialized medical facility (dental surgical department). In the absence of treatment for facial phlegmon, the prognosis is always extremely unfavorable.
How to treat phlegmon?
Treatment of phlegmon is carried out exclusively in a hospital setting. Initially, it is necessary to eliminate the pus; accordingly, treatment begins with the evacuation of purulent exudate - opening and drainage. Excision of necrotic areas occurs, as well as additional opening and excision when pus spreads. This procedure is not carried out only when the phlegmon is at the initial stage of its development, when pus has not yet formed.
How to treat phlegmon? This is where physiotherapy becomes effective:
- Dubrovin dressing (compress with yellow mercury mixture).
- Dermoplasty.
- UHF therapy.
- Sollux lamp.
- Warming compresses and heating pads.
- Infusion therapy.
Medicines are actively used to promote recovery and rejection of dead tissue:
- Painkillers.
- Antibiotics.
- Calcium chloride solution.
- Glucose solution.
- Adonilen, caffeine and other drugs that improve cardiovascular function.
- Antigangrenous serums.
- Hexamine solution.
- Proteolytic enzymes.
- Ointment with enzymes – iruksol.
- Sea buckthorn and rosehip oil.
- Troxevasin.
- General strengthening agents.
- Immunomodulators.
Treatment is not carried out at home, so as not to provoke chronicity of the disease or the spread of pus. The diet includes drinking plenty of fluids and eating foods rich in vitamins. The patient is kept in bed with elevation of the affected limb.
How is cellulitis removed?
At an early stage of the disease, surgery can be avoided. However, with conservative treatment of phlegmon, the patient still needs bed rest, antibiotics, and physical therapy. Against the background of ongoing activities, the patient is monitored throughout the day, and if during this time period the dynamics of recovery do not become positive, he is sent for surgery.
Surgery is usually performed under general anesthesia. The doctor dissects the tissue, removes the neoplasm, tissue affected by necrosis, and washes the purulent contents with antiseptic solutions. After removing the phlegmon, the patient does not need sutures or the suture is of a suggestive nature. Sometimes it is possible to apply a blind suture when installing active drainage systems.
Taking into account the peculiarities of the work of the medical center, we are able to treat only small, in volume, phlegmons if patients refuse hospitalization. The length of stay in the hospital for rehabilitation ranges from seven to fourteen days, while care and treatment are carried out according to the same algorithm as for therapy of purulent wounds.
Treatment in St. Petersburg
In order to get rid of phlegmon or remove an ingrown toenail, you need to contact a medical professional. Our own laboratory, surgical unit and hospital allow us to provide treatment as quickly as possible, and the latest equipment and experienced staff make the level of service provision very high. At the same time, the clinic’s pricing policy makes it possible for every person who cares about their own health to become a client of the center. Maximum comfort of staying within the center, an individual approach and discount programs are among the reasons for contacting the Union Clinic.
| Make an appointment | Make an appointment by calling +7 (812) 600-67-67 or filling out the online form - the administrator will contact you to confirm your appointment |
UNION CLINIC guarantees complete confidentiality of your request.
Complications of cellulitis
If treatment is not treated in a timely manner, such general complications as sepsis (the entry of microorganisms into the blood and the spread of infection throughout the body), thrombophlebitis (purulent inflammation of the veins with the formation of blood clots and microabscesses), purulent arteritis (destruction of the artery wall by microorganisms with the development of massive bleeding, which is very difficult) are possible. stop), secondary purulent leaks as the process spreads.
Depending on the location of the phlegmon, specific complications are also identified, for example, purulent meningitis (inflammation of the meninges) with phlegmon of the orbit, or mediastinitis (inflammation of the mediastinal organs) with phlegmon of the neck.
Possible complications and deep forms of phlegmon
The most common infections will cause serious illness:
- Lymphadenitis;
- Lymphangitis;
- Erysipelas;
- Thrombophlebitis;
- Sepsis.
Facial swelling may be aggravated by purulent meningitis.
If the inflammation begins to spread to nearby tissues, the following may develop:
- Osteomyelitis;
- Purulent pleurisy;
- Tenosynovitis;
- Purulent arthritis.
The latter is the most dangerous complication. As the arterial wall becomes inflamed, it then dissolves and severe arterial hemorrhage occurs.
Deep phlegmon of the extremities is inflammation with pus that spreads through the intermuscular spaces. The source of such inflammation will be various wounds on the skin. For example, a bite, scratch, burn, or disease, panaritium, purulent arthritis or osteomyelitis.
The disease is characterized by pain in the limbs, body temperature increases, and general weakness of the body is present. The disease does not wait long and develops rapidly. As a result, tissue swelling is visible, the lymph nodes in the region enlarge and the limb becomes greatly enlarged. If the phlegmon is located on the surface, you can observe hyperemia and swollen skin.
Purulent mediastinitis. It is a purulent inflammatory process located in the mediastinal tissue.
Often mediastinitis is a form of complication of perforation:
- Esophagus and trachea;
- Purulent formations in the mouth;
- In the pulmonary tract;
- Complication of phlegmon of the neck;
- The result of a hematoma;
- Osteomyelitis of the sternum or spinal column.
This problem is developing rapidly, the patient may experience severe pain in the chest, and the body temperature will rise. The pain will move to the back and neck. The neck and chest will swell. To reduce pain, people often sit and tilt their head forward, which seems to work.
People's heart rates increased, their blood pressure decreased, the veins in their necks dilated, and they complained of pain when swallowing.