Causes of cheek abscess and disease code according to ICD -10
The main provoking factor in the formation of pus is the addition of an infection, which, with the progression of the disease, in the absence of treatment and weak immune defense, leads to the melting of tissues with necrotic contents inside.
Pathological pathogens of cheek flux and inflammation of healthy tissues include the staphylococcal group of bacteria, streptococci, Escherichia coli, and less often, damage to bacteroids that cause phlegmon is observed after treatment with antibiotics.
An abscess develops against the background of provoking factors:
- in case of disruption of the protective barrier of the mucous membrane, weakening of local or general immunity;
- infection in the cheek area spreads from foci of chronic infection - tonsillitis, adenoiditis, with the appearance of stomatitis with white aphthae widespread in the oral cavity, with the formation of injuries - if you bite the mucous membrane until it bleeds, damage the gums with cutlery.
An abscess of the buccal area is classified according to ICD-10 as a purulent skin lesion, boil or carbuncle of the face - code L02.0.
Topographic anatomy
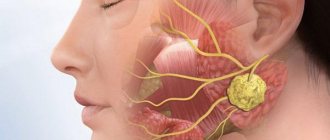
Borders of the submandibular region (Fig. 75): upper internal - mylohyoid muscle (m. mylohyoideus), external - internal surface of the body of the lower jaw, anteroinferior - anterior belly of the digastric muscle (venter anterior m. digastrici), posterior inferior - posterior belly of the digastric muscle ( venter posterior m. digastrici).
Layer structure (Fig. 76). The skin is mobile, in men it has hair. The subcutaneous tissue is loose and well defined. It may contain the marginal branch of the facial nerve (ramus marginalis mandibulae nervi facialis), innervating the muscles of the lower lip and chin, since in 25% of cases it forms a loop that descends below the edge of the body of the jaw by 4-8 mm (F. Henru, 1951; V. G. Smirnov, 1970).
Deeper is the subcutaneous muscle of the neck (m. platysma), covered outside and inside with layers of the superficial fascia of the neck (fascia colli superficialis). Between it and the superficial layer of the neck's own fascia (lamina superficialis fasciae colli propriae) there is a thin layer of fiber in which the vessels are located: the facial vein (v. facialis), the external jugular vein (v. jugularis externa), and in the upper section at the level of the anterior edges of the masticatory muscle (m. masseter) - facial artery (a. facialis). The submandibular cellular space itself (spatium submandibularis) is located even deeper. It is bounded above by a deep layer of the neck's own fascia (lamina profunda fasciae colli propriae), covering the mylohyoid (m. mylohyoideus) and hyoglossus (m. hyoglossus) muscles. From below, the space is closed by the superficial layer of the neck's own fascia (lamina superficialis fasciae colli propriae). Between the named sheets of fascia a closed capsule (saccus hyomandibularis) is formed, in which the submandibular salivary gland (gl. submandibularis) is located. The duct of the gland goes into the gap between the mylohyoid and mylohyoid muscles. This gap is one of the ways to connect the submandibular space with the adjacent cellular spaces of the floor of the mouth. Around the gland, inside its fascial capsule, there are numerous submandibular lymph nodes (nodi lymphatici submandibulares). The facial artery (a. facialis) runs along the posterosuperior surface of the gland, bending over the edge of the lower jaw, approximately halfway between the chin and the angle of the jaw. The facial vein is located on the lower surface of the submandibular salivary gland. Under the gland on the surface of m. hyoglossus are located the hypoglossal nerve (n. hypoglossus), lingual vein (v. lingualis) and closer to the posterior corner of the submandibular triangle - the lingual nerve (n. lingualis). The lingual artery is located somewhat deeper, under the fibers of the hyoglossus muscle (m. hyoglossus), within the so-called Pirogov’s triangle. Thus, in the submandibular region, different localization of the purulent-inflammatory process is possible (Fig. 77).
The main sources of infection in the buccal area
Routes of infection:
- Odontogenic – from focal damage to the dentition, inflammatory gum disease, the formation of an abscess after extraction of elements.
- Non-odontogenic, associated with injuries to the mucous membranes of the oral cavity, cheeks or damage to the facial skin by external factors.
Dental pathology includes:
- cheilitis;
- periodontitis;
- carious lesions of varying severity;
- gingivitis;
- an abscess after the removal of a wisdom tooth on the cheek often occurs due to the high risk of damage to the mucous membrane due to the difficult-to-reach location of the elements;
- periodontal disease;
- failure to comply with daily hygiene rules;
- stomatitis;
- eruption of fangs outwards.
Non-dental reasons for the development of an abscess localized on the cheek:
- injury to the gums with a sharp object - fork, knife, toothpick;
- scratches, deep cuts to the face;
- formations with hematogenous or lymphogenous spread; when the abscess is located in the jaw area, local inflammation of the nearby tissue of the cheeks is possible;
- disease of the ENT organs of bacterial etiology - tonsillitis, otitis media, adenoiditis;
- retropharyngeal boil;
- formation may occur when an abscess of the tongue appears with a history of strong immunosuppression;
- osteomyelitis provokes the spread of infected exudate, an abscess forms on the inside of the cheek;
An examination to find the cause, diagnosis, differential diagnosis, and prescription of a treatment regimen is carried out by a dentist, otolaryngologist, or maxillofacial surgeon.
Characteristic local signs of abscesses and phlegmon of the buccal area
The clinical picture of the development of an abscess differs in symptoms:
- increasing pain intensifies when chewing food or trying to open the mouth;
- purulent infiltrate creates a visual effect of facial asymmetry and swelling on the affected side;
- sensation of pulsation in the affected cheek;
- the skin above the abscess may be red, hot to the touch, stretched, upon palpation with cavity fluctuation, irradiation, pain occurs in the ears, eyes, neck;
- as the abscess progresses, there is a limitation in mouth opening;
- numbness of the surface of the lips is often observed during the extraction of wisdom teeth;
- increase in general body temperature to 39 degrees Celsius;
- a dense formation can be felt from the outside;
- the abscess provokes swelling of the lower eyelid and nasolabial folds;
- as inflammation spreads, an increase in the submandibular lymph nodes is noted;
- in a severe stage of pathology on the cheek, the voice changes, the patient finds it difficult to talk and move his tongue;
- features of the lesion - weakness, malaise, lack of appetite, headaches with an abscess.
Timely identification of symptoms and contacting a specialized clinic will help to quickly and effectively get rid of the problem, preventing the development of negative consequences for human health.
general information
Short description
Purulent limited inflammation of the thickness of the lips:
1. Cellulite is an acute diffuse purulent inflammation of the subcutaneous fatty tissue (phlegmon). Characterized by a significant spread of the inflammatory process.
3. Fistula (fistula) - a channel connecting hollow organs or a tumor with each other or the external environment with the surface or any cavity of the body. It usually looks like a narrow canal lined with epithelium.
, the following clinical concepts are included in subheading K13.0
– “Zaeda (angular and other cheilitis) due to riboflavin deficiency” (E53.0)
2. Some authors indicate serous inflammation separately in the list of inflammatory processes of soft tissues. Sometimes in the literature it is interpreted as cellulite.
3. Adenophlegmon (a type of phlegmon) is a diffuse purulent inflammation of the tissue that occurs as a result of the spread of infection along the length of the affected lymph node.
4. Widespread cellulitis involving adjacent areas is coded in a different category.
Period of occurrence
– Professional medical reference books. Standards of treatment
– Communication with patients: questions, feedback, making an appointment
Download the application for ANDROID
– Professional medical reference books
– Communication with patients: questions, feedback, making an appointment
Download the application for ANDROID
Features of treatment of cheek abscess
The doctor will help you decide on therapeutic methods, taking into account all the nuances of the development of the abscess, localization, presence of complications, assessing the risk of spreading inflammation, the patient’s immune system, age, and concomitant diseases.
Often they resort to opening the attribute located on the cheek; if the abscess is shallow, the doctor will limit himself to conservative treatment with physiotherapy.
Surgical
Surgical treatment of an abscess on the cheek is used for deep, extensive lesions, the presence of complications, extensive symptoms, and the absence of positive dynamics with antibiotic therapy.
Need advice from an experienced doctor?
Get a doctor's consultation online. Ask your question right now.
Ask a free question
Variations of manipulations to eliminate an abscess:
- removal of a tooth affected by caries with sanitation of the oral cavity with an antiseptic solution - often used in pediatric dentistry in the absence of positive changes after treating a formation on the cheek with medications, during extirpation of incisors;
- opening the periosteum in order to evacuate purulent fluid from the abscess cavity, drain the affected area, eliminate inflammation with medications;
- a combination of two methods - tooth extraction and periostomy.
Stages of cheek surgery:
- administration of anesthetic;
- incision of the external capsule of the abscess;
- evacuation of the contents of the cavity with excision of the walls in order to prevent recurrence of pus accumulation;
- antiseptic treatment;
- drainage for large abscesses or suturing for minor abscesses of the cheeks;
- applying a cotton-gauze bandage with a hypertonic solution to provoke rejection of residual masses.
The course of antibiotic therapy after surgery is from 2 weeks, agreed with the doctor individually.
Conservative
The traditional treatment regimen for an abscess on the cheek involves a complex effect:
- Antibiotic therapy using broad-spectrum drugs or a combination of several units to suppress the activity of the pathogen, eliminate toxic waste products of bacteria, and effectively eliminate the purulent contents of the abscess. The group of penicillins with clavulanic acid and cephalosporin drugs are often used. Mostly they resort to the intravenous or intramuscular route of administration due to the severity of the chewing process.
- Local drugs with antiseptic, anti-inflammatory, and sedative effects are prescribed as an element of complex therapy for the elimination of an abscess on the cheek. Treatment with individual methods does not bring the desired results, but helps relieve acute manifestations of the disease. Levomekol, Vishnevsky ointment, Kamistad, Ichthyol liniment, Methogil denta-gel for mucous membranes are used.
- You can rinse your mouth with antiseptic solutions: Miramistin, Chlorhexidine, Chlorphyllipt alcohol.
- For the treatment of abscess, anti-inflammatory and analgesic substances are used - Ibuprofen, Paracetamol, Nimesulide. Long-term use may cause bleeding after tooth extraction.
If there is no positive dynamics in the treatment of the attribute located on the cheek, consult a doctor and adjust the therapy.
Physiotherapy
After opening the abscess in the cheek area, physiotherapeutic procedures are performed to stimulate regeneration and prevent scarring of the facial area:
- exposure to microelectric current pulses to activate cell growth in the lesion;
- UV therapy;
- electrophoresis with medications with a targeted effect on the buccal area;
- Ultrasound pulses;
- laser therapy after an abscess.
Physiotherapeutic influence to obtain a positive effect requires a course of 21-30 days, depending on the severity and extent of damage to the cheeks.
Causes
The most likely cause of a jaw abscess is mechanical damage , trauma , or periodontal pockets (cracks between the tooth and gum that can become infected). An abscess can be caused by any infection that enters the damaged area, either from the outside or through the body’s bloodstream. If a patient has chronic tonsillitis, the cause of inflammation may be streptococci and staphylococci, which constantly multiply in the hypertrophied palatine tonsils. In this case, the patient is recommended not only to treat the abscess itself and damaged soft tissues of the oral cavity, but also to remove the tonsils, if their treatment is not possible. Otherwise, infection may recur many times.