Content
- Common reasons for the increase
- Diseases characterized by an increase in fluid volume Sialolithiasis
- Sialadenitis
- Specific viral infections
- Cyst
- Benign and malignant formations
- Sjögren's syndrome
Varieties
Oral tuberculosis is divided into several subtypes. The most common types are primary, tuberculous lupus, miliary ulcerative and scrofuloderma.
Important information: Focal pulmonary tuberculosis
Primary
Primary tuberculosis of the oral mucosa is a rare subtype of pathology. Observed only in children; in an adult, Koch's bacillus will quickly die in the mouth. Painful ulcers with purulent contents, characteristic of this type of disease, often burst. Education is delayed for a month.
Tuberculous lupus
This type of oral tuberculosis is secondary; lesions are localized on the jaw and face. A tuberculous ulcer that appears during the disease is easily damaged and begins to bleed. The disease occurs in 4 stages: first there is infiltrative, then tubercular, ulcerative and cicatricial.
Miliary ulcerative
Tuberculosis of the tongue, mucous membrane of the cheeks, palate, developing when the pathogen enters small wounds. In areas where pathogenic microorganisms have penetrated the tissue, ulcers and bumps form.
Scrofuloderma
It is observed rarely, more often in childhood. The resulting nodules do not hurt, quickly soften, after which fistulas form. Then follows the scar stage.
Reasons for enlarged salivary glands in adults, and which glands are capable of increasing in volume
The salivary glands play a vital role in the human body, secreting saliva into the oral cavity - a biological fluid involved in metabolic and immune processes.
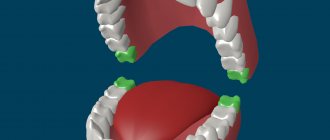
In addition to the many small glands located on the mucous membrane of the tongue, palate, cheeks and lips, there are three types of large glands that are paired:
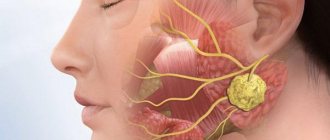
- The parotid glands are the largest glands located in front of the auricle behind the jaw. Large blood vessels and the facial nerve pass through the tissue of the parotid salivary glands.
- The sublingual glands are located symmetrically on the floor of the mouth under the tongue.
- The submandibular glands are located at the base of the lower dental arch, the upper edge is located near the parotid glands.
Where are the salivary glands located: parotid, sublingual and submandibular
Many factors can disrupt the normal functioning of the salivary glands. At the same time, the salivary ducts close, preventing salivary fluid from entering the oral cavity and causing inflammation. A characteristic initial symptom of the pathology is an enlargement of the salivary gland on both or one side.
Note! The average volume of the SF in men is greater than in the fairer sex, but inflammation is observed more often in women.
The parotid glands are especially often enlarged and inflamed. In old and senile age, half of the end sections of the gland are replaced by adipose tissue, diffuse and focal accumulation of lymphoid tissue is noted, as well as atrophy of the glandular sections. In addition, with age, cells - oncocytes - accumulate in the glands, which leads to the risk of the formation of benign and malignant tumors in people after 40 years of age.
Chronic sialadenitis is an inflammatory disease of the salivary glands with insufficiently studied etiology and pathogenesis. It has been established that in patients with chronic sialadenitis, genetically determined homeostasis is determined by a weakening of the body's defenses. A decrease in immunity creates the preconditions for the occurrence of diseases of certain systems, including the salivary glands.
Clinical picture
Interstitial parotitis most often affects women, especially in old age. A characteristic sign of this disease is uniform swelling of the salivary glands. Enlarged glands have a smooth, even surface, are not welded to the underlying tissues, and have a dough-like consistency. The skin covering the salivary glands is not changed, the mouth opens freely, the mucous membrane of the oral cavity is pale pink in color, well moisturized. According to the severity of changes in the salivary glands during interstitial sialadenitis, the initial, clinically pronounced and late stages of the process are distinguished. In the initial stage, patients note discomfort in the area of one or both parotid glands, sometimes pain in the back of the head, swelling of the parotid glands and a feeling of discomfort in the ears periodically appear. As a rule, the disease is discovered accidentally, by a soft, painless swelling within the anatomical boundaries of the gland. The secretory activity of the salivary glands does not change. Cytological examination of the secretion allows us to detect the poverty of smears with cellular elements, single neutrophils and columnar epithelial cells, goblet cells and bare nuclei. On sialograms, uneven images of the gland parenchyma and narrowing of the ducts of the III–V order are noted. The clinically pronounced stage is characterized by constant painless swelling in the area of the affected glands. With sialometry, the secretion of the salivary glands does not change or decreases to the lower limits of normal. During the period of exacerbation of sialadenitis, secretion decreases. Cytological examination of the secretion allows us to establish an increase in cellular elements in smears. On sialograms, the size of the gland is increased, the density of the parenchyma of the gland is reduced, the ducts of the III–IV order are sharply narrowed, the contours of the ducts remain smooth and clear.
Diagnostics
The diagnosis is established on the basis of a characteristic clinical picture, sialography data (increasing narrowing of the excretory ducts), and a cytological picture of the secretion (poverty of cellular elements). Interstitial sialadenitis is differentiated from chronic parenchymal parotitis, sialodochitis, tumor and mumps based on the characteristic epidemiological, clinical, cytological and sialographic signs of these diseases.
Diseases for which the characteristic symptom is an increase in SF
A developing inflammatory process in any of the glands in adults leads not only to problems with salivation, but also to more serious pathologies - almost the entire body is involved.
Salivary stones (calculi) or sialolithiasis
One of the most common problems is salivary stone, which is a formation consisting of calcium salts of the epithelium. The salivary ducts are closed with calcifications, which prevents the flow of salivary fluid into the oral cavity. Saliva accumulates in the ducts of the gland, which become swollen and inflamed, causing progressive pain.
Sialadenitis – inflammation of the salivary glands
The cause of a tumor of the salivary glands can be a bacterial infection, in most cases affecting the parotid glands. It can be caused by pathogenic microorganisms of the oral cavity, for example, staphylococci. As a rule, inflammation is left-sided or right-sided, and the regional parotid lymph nodes are also involved in the process.
In this case, the gland swells, which is accompanied by pain and pus discharge with a bad taste in the mouth. Without timely treatment, the disease can transform into a localized purulent process - an abscess.
Viruses as a cause of enlarged salivary glands
Numerous viruses may also be involved in swelling and inflammation of the parotid glands:
- ARVI;
- flu;
- mumps;
- Epstein-Barr virus;
- cytomegalovirus;
- HIV.
Swelling of the glands, as a rule, appears long before the onset of the main symptoms of a viral infection: fever and weakness. Moreover, swelling occurs on both sides (symptom of “hamster cheeks”), manifesting itself as swelling near the ear.
Cysts
Cysts can be caused by:
- injuries;
- inflammatory processes (stomatitis, sialadenitis);
- obstruction by salivary stone.
Some cysts are thought to be congenital in origin and progress with age.
A salivary gland cyst is a lump that is soft to the touch and filled with mucous, colorless fluid. As a rule, benign transformation occurs with small glands, but in 30% of cases cysts form under the tongue, affecting the sublingual gland. Treatment of cysts is specific, and is under the jurisdiction of maxillofacial surgery.
Neoplasms
The salivary glands are capable of infecting benign and malignant tumors. Among the malignant ones there are:
- adenocarcinoma;
- malignant pleomorphic adenoma;
- mucus-forming squamous cell carcinoma;
- adenoid cystic cancer.
The most common diseases of the salivary glands
A branch of medicine, like dentistry, includes not only the treatment of diseases of the teeth and gums. It involves the treatment of all pathologies that have developed in the oral cavity and inflammation of the salivary glands, including. Below are the main diseases of the salivary glands, which dentists have to deal with most often.
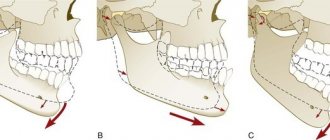
Sialolithiasis
Salivary stone disease is a chronic disease characterized by the formation of stones in the ducts of the salivary glands. Most often the submandibular gland is affected, less often the parotid gland, and it is extremely rare to find damage to the sublingual gland.
The pathology is widespread among the male population and practically does not occur in children. Improper functioning of the salivary glands leads to stagnation of saliva in the duct. At this point, the salts precipitate and the formation of stones begins.
The stones consist of phosphate and calcium carbonate and contain sodium, iron and magnesium.
Stones can grow rapidly, and the size of dense formations sometimes reaches the size of a chicken egg. Symptoms of the pathology are swelling and hyperemia of the skin in the affected area, difficulty chewing, swallowing and talking, dryness of the oral mucosa, pain on palpation in the mouth and cheeks, unpleasant taste in the mouth, hyperthermia, deterioration in general condition, headache and weakness.
Treatment involves conservative (drugs that enhance the secretion of the salivary glands, relieve swelling and inflammation, antipyretic, analgesic, antibacterial) and surgical treatment.
Sialadenitis
Acute or chronic inflammatory disease of the salivary glands, occurring for various reasons (infectious diseases, injuries, developmental abnormalities). The disease most often occurs in children and people over 60 years of age. There are 3 types of sialadenitis: submandibular, sublingual and parotid.
In addition to pain in the ears, throat and nose, the following symptoms may include: increased body temperature, hyperemia and swelling of the skin in the ear area, unpleasant taste in the mouth (putrid breath), pain when pressing on the earlobe, impaired taste, dryness oral mucosa as a result of insufficient secretion of saliva.
In case of complications, duct stenosis, salivary fistulas, abscess, phlegmon of the parotid and submandibular zone may appear. Treatment of sialadenitis is carried out conservatively with the help of antibiotics, antiviral drugs, and physiotherapeutic procedures. In case of frequent recurrent course of the disease, complete removal of the salivary gland is recommended.
Salivary gland cyst
A formation that is formed as a result of a difficult or complete cessation of the outflow of saliva, a violation of the patency of the salivary ducts due to their blockage. The classification of the cyst is as follows: retention cyst of the small gland (56%), ranula, submandibular gland cyst, parotid gland cyst.
Most often it forms on the mucous membrane of the cheeks and lips. It is most often asymptomatic. Measures to combat cystic formation in any location do not involve conservative treatment. The best option is to remove the cyst along with the adjacent tissues and apply self-absorbing sutures.
Sjögren's syndrome
Dry syndrome is an autoimmune disease that affects the exocrine glands, as a result of which dry mucous membranes can be observed not only in the mouth, but also in the nose, eyes, vagina and other organs. The pathology is most often found among women after 40 years of age, often accompanied by diseases such as scleroderma, lupus, and periarteritis.
Symptoms and treatment of gastrointestinal diseases
The first nonspecific signs of Sjögren's syndrome are dry mouth and eye pain, which is cutting and sharp when watching, for example, TV.
When examining the tongue, it is completely dry, it is impossible to swallow saliva, and there is a dry lump in the throat that causes discomfort.
As the disease progresses, photophobia, pain in the eyes, blurred vision, and degenerative changes appear. If you want to “squeeze out” a tear, nothing works, because there is no tear fluid. Two weeks after the onset of the disease, you may notice loosening of the teeth and loss of fillings.
Treatment includes taking glucocorticosteroids, immunosuppressive cytostatics, and symptomatic therapy.
Enlarged salivary glands in women
The probable causes of enlarged salivary glands in women are almost the same as in the stronger sex, however, pleomorphic adenoma is twice as common in them. It mainly occurs between the ages of 45-60 years. Usually the tumor is single, much less common on both sides. In the absence of timely treatment, it can reach large sizes, but grows slowly.
The tumor most often occurs in the parotid glands, but can form under the tongue, and even in small glands. The reasons for its appearance are the subject of much debate among scientists, but presumably the occurrence of the tumor is influenced by:
- bad ecology;
- injuries;
- smoking;
- unhealthy diet.
Treatment of adenoma is only surgical, since radiation therapy is ineffective due to the resistance of the tumor to this method of treatment. The choice of a doctor is of great importance, since with each incision there is a risk of damage to the facial nerve and facial muscles.
Complications of the disease
Inflammation of the parotid gland is considered the most serious, along with mumps, also called mumps. The danger lies in the fact that during the course of the disease, additional glands, for example, the pancreas, may be affected. Considering that this disease is contagious, it is necessary to avoid contact with an infected child and take him to a doctor as soon as possible for the necessary examination and treatment. If this is not done, complications of varying severity may occur, for example:
- The appearance of multiple ulcers in the area of inflammation and next to it.
- Significant increase in body temperature along with debilitating fever.
- Rupture of ulcers into the oral cavity.
- The occurrence of blood poisoning or abscess.
- Formation of fistulas that will bring pus to the surface.
- Phlegmon of the floor of the mouth along with meningitis and damage to the nervous system.
- Development of necrosis of the salivary gland and orchitis.
We will not provide photos of the inflamed salivary gland in children for aesthetic reasons.
Enlarged glands on one side
Unlike multiple inflammations of the gastrointestinal tract, which in most cases are a systemic disease, a single increase indicates a localized process.
Possible diseases characterized by enlargement of the salivary gland on one side:
- sialadenitis;
- tumor;
- salivary stone.
If only one side is swollen, this may indicate a blockage of the salivary duct or a developing tumor.
Note! The submandibular salivary gland is rarely affected by tumors, but approximately 48% of neoplasms are malignant. In turn, the sublingual glands are also rarely subject to inflammatory processes and neoplasms, but 75% of tumors are malignant.
Based on this, any mass formation under the jaw or tongue is a reason for early and active examination, usually requiring a biopsy and surgical intervention.
Causes of enlarged parotid glands in children
By the time a child is born, the salivary glands are not yet sufficiently developed; in newborns they consist mainly of mucous cells. Their full formation is completed by the age of 17-20. Stagnation of saliva and insufficient secretion cause not only difficulties while eating, but also inflammation. Therefore, in children, enlargement of the parotid salivary glands is quite common. Other glands are less susceptible to inflammation.
Often the cause of the increase is bacterial and viral infections, which, if the child’s immunity is inadequate, cause sialadenitis. The development of the disease is provoked by measles, scarlet fever, stomatitis, tonsillitis and other infections.
Mumps in children
Infectious mumps, popularly known as “mumps,” is a viral disease that primarily affects the parotid salivary glands. Along with them, the virus can penetrate the gonads, lymph nodes, and affect the central nervous system. Infection occurs by airborne droplets, the incubation period lasts up to 23 days.
Note! During this period, patients may not have any symptoms, but they pose a danger to others.
In rare cases, non-infectious parotitis occurs, which occurs against the background of obstruction of the salivary duct due to injury from a calculus or other foreign object. As a result, pus is released into the oral cavity, which is formed when pyogenic bacteria enter the salivary gland.
If a child has swelling near the ear, pain and signs of general intoxication appear, self-medication should not be done under any circumstances. The disease cannot be stopped without specially prescribed drugs, and time for adequate treatment will be lost.
Causes of inflammation in children
Doctors identify four main causes of inflammation of the salivary glands in children:
- The presence of a viral infection or bacteria. By airborne droplets, the pathogen enters the child's body, which leads to a significant increase in the size of the glands, and in addition, to painful inflammation. An example is a disease such as mumps, which is often diagnosed in young children.
- Due to obstruction of the salivary duct. Something similar occurs when it is injured or damaged, as well as in the case of the development of a disease such as sialolithiasis.
- Due to poor oral hygiene. Irregular visits to the dentist along with poor brushing of teeth can lead to the child’s salivary ducts becoming a kind of “gateway” for various infections.
- Consequences of complications. Sialadenitis can form after surgery or against the background of diseases such as pneumonia, typhoid, encephalitis, or due to all kinds of poisoning.
Primary inflammation of the salivary glands in children is usually caused by infections, and secondary inflammation by fungi or bacteria. There are different ways of infection: through the salivary ducts, lymph or blood.
Now let's talk about the symptoms of inflammation of the salivary glands in a child and find out how the described disease manifests itself.
Salivary glands and colds
Inflammation in the salivary glands can occur as a complication of respiratory diseases:
- ARVI;
- flu;
- sinusitis;
- tonsillitis.
The reasons for the enlargement of the salivary glands during colds in adults are weakened immunity by the disease and untimely treatment. Therefore, the first stage in the fight against pathology is the elimination of the underlying disease. As a rule, after treatment is started, the affected glands quickly return to normal. You can contact your primary care physician about this problem.
Enlarged salivary glands in anorexia
Anorexia, or anorexia nervosa, is a disease manifested in excessive and deliberate weight loss by the patient himself.
Among people suffering from anorexia nervosa, enlarged salivary glands are quite common. Hypertrophy of the organ is caused by chronic constant regurgitation of gastric contents, which leads to reactive irritation of the nerve fibers of the oral cavity.
In anorexia, the parotid glands are most often enlarged, often 3-5 times their original size. Their increase is more pronounced if it is accompanied by hypertrophy of the masticatory muscles, which is often observed in patients with anorexia.
How to treat the salivary gland
When the salivary gland swells, the natural question arises of what to do and who to contact with this problem. A dentist can diagnose the pathology during an examination. If pain and symptoms of intoxication appear, you should immediately consult a therapist, who will determine why the glands are swollen and, if necessary, refer you to see specialists.
Treatment depends on the cause of the disease. If the gland is swollen as a result of the formation of stones, then treatment consists of removing them and using local anti-inflammatory therapy.
In case of neoplasms, surgery with radiation and chemotherapy is used. Surgical removal is indicated for the treatment of cysts.
All other pathologies of the salivary glands can be controlled with drug therapy. For a bacterial infection, a course of antibiotics and supportive treatment is prescribed.
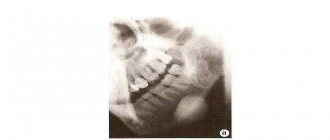
Tuberculosis of the salivary glands
Pathogenesis and pathomorphology.
The parotid tendons are affected. less often - submandibular and sublingual glands. The lesion is usually one-sided. Patients complain of pain when swallowing, dry mouth. There is a slow formation of a tumor with inflammatory manifestations. Possible formation of a fistula with the separation of thick, odorless grayish pus; possible formation of a fistula with the separation of thick, odorless grayish pus.
Diagnostics. Detection of deformation of the salivary ducts, calcifications and fistulas during X-ray examination only indirectly indicates the tuberculous etiology of the lesion.
Final confirmation of the etiology of the disease is based on cytological and bacteriological studies of the material obtained by puncture
With the development of extensive abscess formation in the salivary gland, its resection or removal is indicated.
.Signs of tuberculous sialadenitis include areas of destruction of the salivary glands in the form of cavities of various sizes and shapes; uneven size of lobular glands due to atrophy and desolation of some of them due to the development of connective tissue; presence of calcifications. Diagnostics.
Detection of deformation of the salivary ducts, calcifications and fistulas during X-ray examination only indirectly indicates the tuberculous etiology of the lesion.
The final confirmation of the etiology of the disease is based on cytological and bacteriological studies of the material obtained by puncture of one or another gland and histological examination of the affected tissue (after superficial parodectomy). The detection of MBT or specific granulomas with caseous necrosis in the center makes the diagnosis absolutely correct.
Ticket 14
1. Immunopathogenesis of MTB Secondary T-cell immune response
A secondary immune response develops upon repeated contact with the antigen. Antibodies, mainly igg, appear faster and in a higher titer than during the primary immune response. However, by reducing the duration of the latent phase of the immune response to 48–72 hours, there is no tendency to generalize the process. There are T cells of immunological memory.
They have a long lifespan, circulate in the blood and, after the first contact with the antigen, “remember” it for many years. After repeated contact, immunological memory cells recognize the antigen and a secondary immune response occurs - a more intense proliferation than during the primary immune response.
As a result, a large number of effector T cells, the so-called killer cells, are formed.
Tuberculosis of peripheral lymph nodes. Indurative form
Inflammatory changes subside, caseous masses become calcified. Lymph nodes decrease in size, become dense, and the disease becomes prone to wave-like progression.
Diagnostics - objective examination, Mantoux test, puncture biopsy
Treatment - includes antibiotic chemotherapy and surgical treatment methods
Ticket 15
1.Pathogenesis of primary tuberculosis
The MBTs that have reached the alveoli undergo phagocytosis by alveolar macrophages. The macrophages fix on the MBT membranes, immersing them in the CP with the image of the phagosome. Further, the formation of phagosomolysosome complexes occurs as a result of the fusion of the phagosome or isosome. Lysosomes contain farms that destroy macromolecules.
Infected macrophages release into the extracellular space the destruction of the office, mediators IL-1, which activates CD4 + cells (T-HELPER). They secrete lymphokines - IL2 and interferon-gamma, under the influence of which the migration of new macrophages to the site of lysis and stimulation occurs.
Activated macrophages secrete tumor necrosis factor, which initiates the formation of a granuloma product, which limits the spread of MBT and prevents their reproduction. In the center of the granuloma there are epithelioid cells, along the periphery there are plasmacytes, lymphocytes, neutrophils and Pirogov-Lanhhans gigabyte cells.
Subsequently, the granuloma product is surrounded by a fibrous capsule, and its center becomes necrotic. Limiting the area where the office is located and necrosis reduces the partial pressure of O2 and creates an unfavorable environment for the proliferation of the office.
MTB—organism—primary fixation and formation of primary pulmonary affect (subpleural, 3, 8, 9, 10 segments (well ventilated))—entry into the lymphatic system (lymphadenitis or lymphangitis) and formation of the primary tuberculosis complex. Outcome: recovery (formation of a focus of Gon) and 2. progression and generalization of the process.
Instead of the primary affect, alveolitis, which is replaced by cheesy necrosis, because The lesions are subpleural, then the pleura is involved (pleurisy).
PHASES: 1) pneumonic (formation of pervasiveness)
2) resorption phase (caseosis image)
3) compaction phase (the primary focus is well defined, the contours are clear, along the periphery the beginning of calcification in the form of small crumbs)
4) formation of a Gon lesion (encapsulation, calcification or ossification)
Source: https://studfile.net/preview/6469398/page:9/