950
All doctors are unanimous in the opinion that the effectiveness of therapy for most diseases depends on the timeliness of their diagnosis.
However, there are pathologies that are hidden in nature and do not manifest themselves for a long time.
In the field of dentistry, such ailments include cementoma - a neoplasm in the oral cavity, which is often detected at the peak stage of development during a routine examination.
General information
Cementoma is a type of benign tumor that is localized in the area of the tooth root. It is characterized by the formation of fibrous cement-like tissue, which only a specialist can identify.
The development of the disease is accompanied by the destruction of bone and epithelial tissues of the oral cavity. When it reaches a large size, cementoma leads to deformation of the jaw, and in some cases, its fracture.
Most often the disease is diagnosed in women. At the same time, the risk group includes patients whose age does not exceed 20 years. Cementoma is often located in the area of the central elements of the lower jaw row.
However, with a more complex variant of the development of the disease, the tumor may be localized in the upper jaw, which threatens to grow into the maxillary sinuses.
Benign tumors of the lower jaw
Treatment of Cancer >> Books on Oncology >> “Handbook of Oncology” Edited by Professor B. E. Peterson Third edition, revised and expanded Publishing House “Medicine”, Moscow, 1974 OCR Wincancer.Ru Given with some abbreviations
Primary tumors of the lower jaw can be non-odontogenic and odontogenic. Among nonodontogenic benign tumors, osteoblastoclastomas are most often observed, and fibromas, chondromas, osteomas, osteoid osteomas, and hemangiomas are less common. By their nature and clinical course, they differ from identical bone tumors only in their localization. In this regard, a description of non-odontogenic tumors of the lower jaw is not possible here. Odontogenic benign tumors in the lower jaw include epulis, adamantinoma and, rarely, odontoma.
EPULIS (supragingival)
. This term is used to refer to tumors (giant cell epulis) and tumor-like formations (fibrous, angiomatous epulis) that arise on the gum from the tissues surrounding the tooth (periodontal). It is usually observed between the ages of 20 and 40, more often in women.
Pathological anatomy. Macroscopically, epulis is a spherical or mushroom-shaped growth of soft tissue on the gum, covered with a mucous membrane. Tumors are 2-3 cm in size, and sometimes larger. They can be dense, densely elastic and soft in consistency. Tooth marks are sometimes visible on the surface, and less often - ulceration. Microscopically, fibrous epulis consists of bundles of mature fibrous connective tissue. Angiomatous epulis is characterized by the proliferation of thin-walled blood vessels of the capillary or venous type with the formation of cracks and cavities. Giant cell epulis (extraosseous) is similar in histological structure to osteoblastoclastoma. They contain giant multinucleated cells such as osteoclasts and mononuclear cells with round-oval nuclei such as osteoblasts.
Clinic
. The development of epulis is often preceded by prolonged irritation from the sharp edges of teeth, crowns, and dentures. It is located in the area of the gingival papilla, near the edge of the gum, and has the appearance of a rounded brownish-brown formation with a wide base. There is a spreading of nearby teeth. Sometimes (after injury) heavy, often recurring bleeding is observed. Growth is usually slow, but sometimes the tumor enlarges over several weeks. Particularly rapid growth is observed in women during pregnancy. Malignancy of epulis has not been registered.
Diagnostics
. The characteristic location of the tumor on the gum usually allows a correct diagnosis to be made. X-ray examination reveals a clearly demarcated focus of lysis of a round or oval shape with transversely running trabeculae. There is swelling of the bone, thinning of the cortical layer. Differential diagnosis should be made with gingival polyps (false epulis), dental pulp polyps, and osteoblastoclastoma.
Treatment
. The most effective resection of the alveolar process is with one or two teeth. This volume of surgery is necessary due to the fact that epulis develops from the periodontium or surrounding bone (alveolar wall or alveolar process). The epulis is removed as a single block with the bone, gum and teeth. The resulting defect is filled with an iodoform swab. Correctly performed surgery provides a good prognosis.
ADAMANTINOMA (ameloblastoma, adamantoblastoma)
. A benign epithelial tumor, similar in structure to the tissue from which the enamel of the tooth germ develops. The tumor develops from elements of the tooth germ at various stages of its development. It is observed rarely, but predominantly (up to 90% of cases) in the lower jaw. It occurs equally often in men and women, usually between the ages of 20 and 40. It is localized in the thickness of the lower jaw in the area of its angle.
Pathological anatomy
. There are solid and cystic forms of adamantine. Macroscopically, the solid form has the appearance of a soft grayish-pink tumor, in places brownish in color. In the cystic form, there are several interconnected cavities with smooth or slightly lumpy walls, separated by layers of soft tissue filled with light or brownish liquid, and sometimes colloid-like contents. Microscopically, strands of epithelial cells (cubic and cylindrical) are determined. Characteristic is the growth of the epithelium, similar to the structure of the enamel organ of a developing tooth. The fibrous stroma of the tumor is usually well developed. Sometimes stromal hyalinosis and calcification are observed.
Clinic
. The most typical is a slowly developing deformation of the lower jaw (usually in the area of its angle) in the absence of pain. Gradually, the facial deformity increases, and movements in the mandibular joint are impaired. Subsequently, symptoms of difficulty swallowing, pain, and, if the tumor is very large, bleeding from the mucous membrane ulcerated over the tumor appear. Tumor growth is usually slow, but malignancy is observed in 1.5-4% of cases. Adamantinomas are prone to recurrence, sometimes many years after surgery. Malignant transformation is manifested by accelerated growth and germination of the tumor into surrounding tissues. Metastases (lymphogenous) are rare.
Diagnostics
. In addition to the described clinical picture, radiological data are important for recognizing adamantinoma. Radiographs reveal a centrally located, well-demarcated single- or multi-chamber shadow with bay-shaped contours. The bone is swollen and thinned. There is no reaction from the periosteum. Differential diagnosis should be made with a single-chamber cyst, osteoblastoclastoma, fibrous dysplasia. Recognition can be facilitated by puncture and cytological examination, and in difficult cases, biopsy.
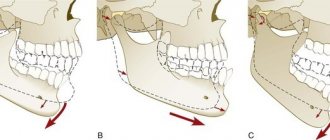
Treatment
. The method of choice is resection of the lower jaw. The extent of the operation is determined by the location and size of the tumor (resection without or with disruption of the continuity of the mandibular bone, resection of half the jaw or disarticulation). After surgery, splinting is necessary followed by bone grafting or prosthetics. Limited operations such as curettage are always accompanied by relapses and lead to accelerated tumor growth.
Forecast
.
If surgical intervention is performed in a timely and correct manner, it is favorable. See further: Malignant tumors of the lower jaw >>
Causes
Dentists note that a single reason that can cause the formation of cementoma has not yet been identified. There are several factors that serve as an impetus for the development of pathology:
- chronic inflammatory processes in the oral cavity , which include osteomyelitis, fibrous periodontitis, actinomycosis;
- single injury to the jaw rows as a result of impact, bruise, damage to soft and hard tissues;
- regular damage to oral tissues - the presence of poorly fitted dentures and orthodontic structures, unprofessionally installed fillings, sharp edges of teeth as a result of their carious lesions.
Experts also identify such important reasons that provoke the development of the disease as genetic predisposition and negative effects on the tissues of the oral cavity from the outside, for example, smoking, radiation therapy.
The main causes of tooth decay in adults and children.
Read here about the disease mucositis of the oral mucosa.
At this address https://zubovv.ru/krasota-i-uxod/narashhivanie/chto-delat-esli-otkololsya-nebolshoy-kusochek-zuba.html we will tell you what to do if a piece of a molar breaks off.
Possible reasons for the appearance
There are no clear answers to questions about the etiology of cementoma.
It has been proven that a predisposition to one of its types, the gigantic form, is inherited; it has been observed in groups of related people.
Presumably, the occurrence of cementoblastoma can begin with:
- Inflammatory process in the oral cavity and nasopharynx. Periodontitis, sinusitis, osteomyelitis.
- Injury to the gums or jaw, bruise, cut or fracture.
- Constant traumatic impact of a diseased tooth or incorrectly installed orthodontic equipment.
READ What is jaw odontoma?
It is assumed that the chance of cementoma occurring may increase under the influence of radiation, toxins, or smoking.
Symptoms
The key feature of cementoma is that it is asymptomatic. At the initial stage of the disease, the patient does not have any signs of developing oral pathology.
The progression of cementoma and its growth leads to a decrease in the thickness of the cortical plate, which is reflected in an increase in pressure on the periosteum. At this stage of the disease, a person develops the following symptoms of the presence of pathology:
- slight pain during eating and communicating;
- discomfort when pressing on the affected area;
- slight change in the color and structure of the enamel.
Excessive growth of the tumor can lead to rupture of the mucous membrane and soft tissues of the oral cavity, as well as deformation of facial features.
How to detect asymptomatic dental cementoma and how to treat it
The disease is diagnosed using x-ray examination, most often by chance, if it does not cause any inconvenience to the person. On an x-ray, the formation appears as a dense darkening of an oval or round shape in the area of localization on the jaw.
In 90% of cases cementoma is a practically asymptomatic disease, but if any signals arise, they look like localized discomfort when eating and talking. Gradually mineralizing and growing, the connective tissue captures the bone tissue of the jaw. As a result, there is a violation of blood circulation in this area, the formation of cysts, displacement of the dentition, deformation of the jaw and, accordingly, a change in the oval of the face.
The prognosis for treatment of the disease is favorable. The most important thing is detection of the tumor. In general, dental cementoma does not require surgical intervention. If the disease is at rest and does not cause significant disturbances in the area of its localization, then in this case dynamic observation has proven itself best. Since the cementoma of the tooth is associated with its roots, maximum caution in the intervention and competence in its implementation are necessary. During surgery, the defective area of tissue is removed with the maximum possible preservation of the jaw bone and tooth roots.
And as always, remember the most important rule of health: respect your body and visit specialist doctors on time.
Classification
There are several types of cementoma, each of which has its own characteristics and symptoms.
Benign cementoblastoma
Under the name benign cementoblastoma or true cementoma lies a neoplasm consisting of coarse fibrous tissue of varying degrees of mineralization. The tumor is located in a capsule that separates it from healthy cells.
Cementoblastoma is defined by slow but unlimited growth. At the initial stage of the disease, there are no symptoms.
Over time, resorption of the cortical plate occurs, which entails discomfort and pain during palpation and eating.
At an advanced stage of the disease, deformation of the jaw may be observed, as well as the eruption of a tumor, which leads to its infection and the development of inflammation.
Most often, cementoblastoma is localized on the lower jaw row in the premolar area.
Cement-forming fibroma
This type of neoplasm is characterized by a passive course with mild symptoms. As the tumor grows in the bone tissue, a lesion with weak mineralization of the tumor is formed.
This occurs as a result of the tumor having a fibroblastic structure. Cement-like tissue is formed only at the final stage of the disease, when the growth of the formation stops.
When a cement-forming fibroma is located on the maxillary line, its spread to the maxillary sinuses may be observed.
Periapical cement dysplasia
The disease is characterized by a pathological process that occurs in dental cement and bone tissue, during which the walls of the molar roots become thinner, which eventually leads to their fracture. Cement dysplasia, as a rule, has many lesions not exceeding 1 cm in diameter.
The formation and development of the tumor is asymptomatic. No jaw deformation is observed. Therefore, detection of a neoplasm in some cases occurs when taking an x-ray during treatment of concomitant diseases.
A common variant of tumor localization in cemented dysplasia is the frontal parts of the lower jaw row.
Gigantoform cementoma
The disease is characterized by intensive transformation of connective tissue into cement tissue. The X-ray image shows oval-shaped tumor areas located in close proximity to the root of the tooth.
They can be localized in different areas of the jaw rows, but, as a rule, symmetrically to each other.
According to experts, gigantoform cementoma is a genetic disease, so it can occur in several members of the same family. The presence of a tumor can only be detected by the results of an X-ray examination.
Varieties
Dentists divide neoplasms of tooth roots into four main types:
- Benign cementoblastoma or true cementoma. Development proceeds with a minimum of clinical symptoms. It can only be detected by chance, on x-rays obtained during the treatment of the affected or adjacent teeth. The tumor is firmly connected to the root, separated from other adjacent tissues by a membrane, and is formed on the outside of the jaw. The neoplastic tissues are similar to those affected by Paget's disease, in which the growth of new bone tissue outpaces the death of old bone tissue.
- Cementing fibroma, like the previous one, does not have specific pronounced symptoms. It causes thinning of the bones, which can lead to mild pain when pressed. It is also detected only with x-rays; in the photographs, clear outlines of an area of sparse bone are visible.
- Periapical cement dysplasia. It is a new formation of cement tissue near the end of the tooth root and thins it. This form of cementoma is often discovered during the treatment of a broken tooth. The pathological process goes through three stages. On the first, osteolytic, new tissue grows, on the second, calcifying, areas of mineralization appear and then grow. At the third stage, the tumor is called mature; morphological changes in it cease. The size of the formation rarely exceeds one centimeter, and it extremely rarely begins to grow again.
- Gigantoform cementoma. Hereditary form of the disease. It is characterized by very dense neoplasm tissue, comparable in density to dental tissue. There are several lesions, they are located symmetrically.
Also, the classification of neoplasms occurs according to their location.
Cementoma of the lower jaw is more common and less dangerous than the upper jaw. Damage to the root of the upper tooth threatens nosebleeds, difficulty breathing, and forward displacement of the eyeball.
Based on the number of affected roots, a distinction is made between local, developing in the area of one tooth, and diffuse, covering several adjacent teeth.
READ What causes jaw dislocation?
Diagnostics
Due to the absence of pronounced symptoms and external changes, diagnosis of cementoma is possible only in a dental clinic.
After clarifying the patient’s complaints and conducting a visual examination, the specialist will suggest performing x-rays of the jaw rows, which can be used to identify dense oval neoplasms.
With the help of microscopic examinations, a specialist is able to determine the structure and structure of the transformed tissues, which makes it easier to identify a specific type of tumor and make a diagnosis.
Histological examination involves studying the tissue that forms the tumor and is carried out with the aim of differentiating cementoma from other types of tumors.
What is gum fibromatosis, treatment of pathology in the clinic and at home.
In this article we will discuss why gums bleed during pregnancy.
Follow the link https://zubovv.ru/detskaya-stomatologia/d-zubi/vospalenie-nadkostnitsyi-naznachit-vrach.html if you are interested in how inflammation of the dental periosteum is treated with antibiotics.
Etiology of occurrence
Dental experts are still working on the causes of cementoma. To date, it has been possible to identify several factors that contribute to the formation of tumors according to medical indicators.
These include:
- long-term chronic inflammatory processes of the oral cavity - fibrous periodontitis, osteomyelitis, actinomycosis, sinusitis, etc.;
- injuries of a chronic nature - damage to the mucous membrane of teeth destroyed by caries, incorrectly installed dentures, sharp areas of fillings;
- immediate injuries - bruises, blows, mechanical damage to the jaws and gum tissue.
Experts do not rule out a genetic predisposition to the formation of cementoma. A version of the long-term harmful effects of certain unfavorable factors is also being considered. For example, smoking or radioiodine therapy.
See photos of tooth extension on a pin and learn about the modern approach to this procedure. In this article, read about what the official website of Ankylosis implants offers.
Follow the link https://dr-zubov.ru/lechenie/zuby/znachenie-i-primenenie-premedikacii.html if you are interested in how children are given premedication in dentistry.
Treatment
The method of treatment for cementoma depends on the type of disease:
- Treatment of benign cementoblastoma and cementing fibroma is based on surgical removal of the tumor with partial excision of the bone tissue that was affected. A tooth located in the area of development of the pathological process and fused with the neoplasm is also removed.
- Periapical cement dysplasia does not imply active growth of the tumor. When treating it, the surgical method is most often not used, since the creation of provoking factors can lead to tissue necrosis.
If the pathology is asymptomatic, treatment is based on regular monitoring, improving the quality of oral care, monitoring the area of periapical lesions and measures to prevent tooth loss.With severe symptoms and the presence of an inflammatory process, the sclerotic masses are rejected, which takes quite a long time, but ends with recovery. To speed it up, a specialist can form a depression in the area of the affected bone tissue.
- In the presence of gigantoform cementoma, conservative methods of therapy are also used. The patient is prescribed anti-inflammatory drugs, as well as constant monitoring by the dentist.
Modern classification
Modern medicine distinguishes two main types of disease, which are characterized by the area affected:
The photo shows a giant cementoma of the lower jaw
- local - the tumor occurs near the root of only one tooth;
- diffuse - pathology affects the area of several tooth roots, and also affects bone tissue.
Depending on the specific type of cementoma, the pathological process has unique causes and symptoms:
- Fibroma . The symptoms of fibroid cementoma are unclear. The tumor damages the bone cortex and forms mineralizing zones. The capsule is located on the outside.
- True . Signs of pathology are weak. Just like fibroids, there are areas of calcium accumulation. The neoplasm is covered with a membrane, due to which the pathological process has a limited area. Formed from the outside.
- Fibrous . Another name is periapical cement dysplasia. Localized in the posterior part of the mandibular structure. A fibrous tumor is characterized by the formation of many foci, bone destruction and places where minerals accumulate.
- Gigantoform cementoma. The most complex type of disease in which transformation into cement connective tissue occurs. The neoplasm grows tightly to the tooth root. The tumor has a high density.
Complications
In most cases, complications resulting from the development of cementoma occur if the neoplasm is located in the upper jaw row.
This is dangerous because the tumor can grow into the nasal sinuses, which can subsequently provoke the development of nasopharyngeal diseases.
Another complication of cementoma can be a breakthrough of the oral mucosa with the emergence of a neoplasm on its surface. As a result of such perforation, a hole is formed from the bone tissue to the mucous membrane.
The consequence of this phenomenon is often infection of the affected area, which spreads to other parts of the jaw.
Causes of jaw tumors
Tumor diseases tend to change their nature of origin, which is why it is not possible to name a single cause for the occurrence of a tumor in the jaw. Modern medicine continues to study various types of circumstances that provoke a tumor process in the jaw. The only reason for the appearance of a tumor, as all experts believe, is a jaw injury. In all other respects, opinions differ to a greater or lesser extent. The nature of the injury can be either prolonged (internal injury to the oral mucosa) or isolated (bruise of the jaw). Also a common cause of the disease are foreign bodies (material for filling a tooth or its root) and inflammatory processes that develop over a long time.
Adverse habits such as smoking and poor oral hygiene contribute to the occurrence of neoplasms. There is a high probability of a jaw tumor appearing during chemotherapy and radiotherapy treatment.
Tumors of the jaws can manifest themselves as a distant focus of cancer pathology.
Prevention
Key methods for preventing cementoma are aimed at preventing damage to the teeth and jaw, as well as regular oral care.
Experts recommend following these tips:
- brush your teeth at least twice a day and rinse them after each meal;
- in addition to a toothbrush, use floss or irrigator;
- promptly seek help in case of mechanical injury to the teeth, mucous membrane or temporomandibular joint;
- do not delay treatment of dental diseases;
- undergo regular dental examinations and oral hygiene.
What complications may arise
Complications, as a rule, arise when a tumor forms in the anterior part of the upper dentition. As the tumor grows, there is a high probability of it growing into the sinuses, which is fraught with serious complications.
Another no less dangerous complication may be a breakthrough of the mucous membrane with the eruption of the tumor outward. As a result, the risk of infection entering the affected tissue increases significantly. Infection is accompanied by the development of inflammation with further spread of the pathological process in the oral cavity.
Reviews
Most patients treated for cementoma note that they did not notice the symptoms of its development, and the diagnosis of the disease was the result of a visit to the dentist for other reasons.
That is why experts recommend not to neglect regular preventive examinations, since in most cases it is easier to prevent the development of the disease than to eliminate it, especially at an advanced stage.
If you have encountered any type of cementoma, please share your experience regarding the course and treatment of this disease.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags jaw
Did you like the article? stay tuned