After removal: norm and deviations
After surgery to remove a tooth and the tumor subsides, the patient may find bone protruding from the gum. In addition, unpleasant sensations arise.
- not all fragments of the destroyed tooth or its root were removed;
- the jawbone was exposed;
- a fragment of the interdental septum appeared;
- supernumerary tooth erupts;
- exostosis develops;
- alveolar ridge.
Important! Only a doctor can diagnose this phenomenon, often after an X-ray examination.
In case of complications and lack of treatment, the following consequences are possible:
- The occurrence of an abscess is an inflammation characterized by suppuration of the tissue. Which leads to phlegmon - extensive damage to adjacent tissues, sepsis - blood poisoning and death.
- Cervical lymphadenitis is inflammation of the submandibular lymph nodes. Characterized by neck pain and high body temperature. If left untreated, pus comes out of the lymph nodes.
- The appearance of a radicular cyst, when the inflamed area is separated by a purulent capsule. This leads to fragility of the jaw bone, the occurrence of a fistula and osteomyelitis of the jaw.
- Alveolitis is inflammation of the walls of the socket. It manifests itself as prolonged pain in the gums, discomfort while eating, severe inflammation and swelling of the gums, fever, headaches and weakness.
Important! Even if inflammation has not developed, there is no pain and there is no discomfort, if bone appears from the gums, it is necessary to visit a dentist for a diagnosis.
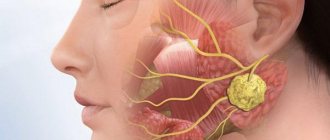
Photo 1. Inflammation of the periosteum often occurs due to incomplete removal of tooth fragments. In this case, surgery is required to remove them.
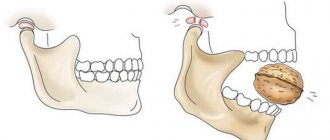
Photo 2. Sometimes after a complex tooth extraction, patients notice protruding bone in the gum. Perhaps this is exostosis; to make an accurate diagnosis, it is recommended to consult a dentist.
Photo 3. A bone is clearly visible near the hole filled with a blood clot. In this case, it may be a previously unnoticed tooth fragment, a jaw bone, or a supernumerary tooth.
If the patient had to have a tooth removed, you need to think about implantation or prosthetics as soon as possible. It is impossible to leave empty space in the dentition for a long time, since after a few years the bone tissue at the site of the extracted tooth will begin to atrophy, and it will not be easy to install an implant. Let's figure out what atrophy of the jaw bone tissue is after tooth extraction and how to avoid it.
The consequences of jawbone atrophy can be not only cosmetic disorders, but also digestive problems
Most dental patients underestimate the severity of bone atrophy after tooth loss. At first glance, it may seem that if a person loses one or two teeth, he does not risk anything. In fact, the loss of bone tissue affects not only the appearance, but also the functioning of the internal organs.
Bone atrophy provokes the following processes:
- Change in face shape, recession of cheeks, lips
- Increase in the number of wrinkles on the face
- Impaired diction, lisp
- Disruption of the normal functioning of the digestive system caused by insufficient chewing of food
- Displacement and loosening of adjacent teeth, increase in interdental spaces
- Problems with implant placement
There are different methods to speed up healing. Some surgeons load material for bone grafting - artificial bone plastic material - into the socket of the extracted tooth. This method is not always effective because the powder may wash out of the socket during the first two weeks. Others simply stitch the hole tightly so that the blood clot does not escape.
In our dental clinic we have found a method that gives a guaranteed positive result.
After tooth extraction, an empty space remains, which is filled with fast-growing gum cells - they do not allow the bone to fully recover and fill the bed where the tooth root used to be. Therefore, bone atrophy occurs, that is, a decrease in tissue volume, especially since it ceases to receive the usual load from the tooth.
Dental implantation with immediate loading of a prosthesis FOR 1 TOOTH: RUB 35,000. Save RUB 10,000. FOR 1 JAW: 265,000 rub.
Free consultation with an implantologist or write to us
Resorbable membranes dissolve in the oral cavity on their own. Therefore, they are fixed simultaneously with the replanting of an artificial or natural graft. The operation is carried out as follows.
After a tooth is removed, the gums peel off. The hole where the tooth was just located is filled with bone chips (graft). This may be the patient's own bone, cadaveric bone from another person, artificial material, or animal bone. Afterwards, the planted material is covered with a protective membrane, which after 6-8 weeks completely resolves on its own. The gum is returned to its place, stitches are applied. Once the grafted bone has completely healed, dental implants can be placed.
Non-resorbable membranes in the oral cavity do not dissolve and must be removed. Their installation is carried out in a less traumatic way - without massive incisions in the gums and the imposition of a large number of stitches.
After the tooth is removed, the hole is also filled with bone chips. A protective membrane is installed that will protect the cavity from fast-growing gum tissue cells. It is secured with small seams. While the bone tissue is being restored, a temporary denture is fixed. After the grafted bone has completely healed, the membrane is removed. The installation of implants can be carried out either at the same time or after a few days/weeks - depending on the condition of the bone.
These procedures allow you to protect the bone from resorption, preserve its volume immediately after tooth extraction, and install dental implants without complex bone augmentation. But if the budget and indications allow, then instead of membranes it is better to place an implant in the socket of a newly extracted tooth. This way you will significantly reduce the time required for tooth restoration.
Preventing bone loss after tooth extraction photo and video
After tooth extraction, it is important to resort to implantation as soon as possible. If the patient hesitates with this procedure, an unpleasant surprise may await him in a few years. Bone atrophy, which often occurs after tooth loss, is an expected phenomenon that can greatly complicate implant placement and generally worsen the patient’s quality of life.
We invite you to familiarize yourself with what a dental nerve looks like and how to kill it at home, a detailed illustration of the process and advice from dentists
“There is not enough bone tissue, osteoplasty needs to be done,” is the verdict heard by approximately 80% of patients who apply for dental implantation. Our implant surgeon Vladimir Aleksandrovich Voznyuk spoke about why problems with bone tissue arise, how its augmentation is carried out and whether it can be avoided.
There are many different methods, each of them has its own indications. The doctor decides which method is suitable for a particular patient during a consultation, based on examination data and computed tomography.
But in general, all osteoplastic operations are divided into 3 groups:
- Different osteotomy options. The doctor “stretches” the existing bone to create more space for the implant.
- Transplantation of your own bone (autotransplantation). Bone is taken from an area where there is a lot of it (for example, from the angle of the lower jaw or from the femur) and transplanted to where it is missing.
- Osteoplasty using biomaterials. The area to be restored is filled with artificial bone material. This may be cadaveric human bone (specially processed), animal bone, or a synthetic bone substitute (such as hydroxyapatite). The biomaterial is absorbed over time and replaced by the patient’s own bone tissue.
Implantation can be carried out simultaneously with osteoplasty, but more often it is performed in a separate stage - 3-6 months later, after the implanted material has finally taken root and the bone volume has been restored.
It is possible if the patient is missing a large number of teeth - 3 or more. Extended defects give the doctor more room to maneuver. He may not install implants to replace every missing tooth, but rather fix just a few systems at an angle, choosing those places in the jaw where atrophy is minimal.
For example, with a completely toothless jaw, it is enough to install only 4-6 implants into the bone, two of which are placed vertically in place of the front teeth, the rest - in the lateral areas of the jaw at an angle (all-on-4 technology). The operation itself is planned on a computer, which eliminates the slightest inaccuracies when working in a limited bone space.
For greater stability, the implants are covered with a permanent prosthesis on the same day or 3-4 days later. It has a metal frame that firmly connects the systems and prevents them from loosening. Almost immediately, patients can fully chew any food.
Compared to classical implantation, techniques that do not require bone tissue augmentation are associated with lower risks, are easier to tolerate by patients and allow you to get new teeth in just a few days. And yet they have one drawback: they are not applicable for single defects.
Did you like the material? Like and subscribe. We write about how to keep your teeth healthy and what to do if problems arise.
Losing a tooth is not only fraught with cosmetic consequences, i.e. aesthetic defects. Functional impairments also occur. After all, healthy teeth have to take on excess load while chewing food. This means they break down much faster. In addition, all the teeth in the row shift and become mobile - after all, some of them lack lateral support.
In general, the bite and facial expressions are disturbed, and wrinkles appear. The lips sink inside the mouth, problems arise with the pronunciation of various sounds, because the tongue loses support in the form of teeth, a decrease in the lower part of the face is observed, and flabbiness of the masticatory and facial muscles develops2. In addition, the digestive organs suffer, since a person most often switches to softer foods, since it is too difficult to chew excessively hard foods.
- Added 11/27/2019
- Gum treatment
- No comments yet
Alveolitis
Diagnosis of the problem
The patient is not always able to correctly assess the situation after tooth extraction. A piece of bone may be perceived by him as the growth of a new tooth, along with unpleasant sensations and pain. To remove a fragment, you do not need to rely on your knowledge and experience of friends and relatives; you need to go to specialized medical institutions, where a qualified doctor can diagnose and prescribe the correct treatment.
In preparation for surgery, the dentist will collect anamnesis, study x-rays and plan all stages of therapy. For it to be successful, you need to inform your doctor about all medications you are taking and avoid drinking alcohol. If the patient is intoxicated, stressed, or suffering from exacerbated chronic diseases, the operation will have to be postponed.
Inspection
If a patient complains of discomfort and pain due to a bone sticking out in the socket, the doctor is obliged to examine the patient’s oral cavity for the presence of an inflammatory process. Only upon completion of a professional diagnosis can the foreign body be removed, followed by treatment of the gums with antiseptics. After examining the resulting wound, the dentist will complete the operation and take appropriate measures. It is worth adding that thanks to modern technologies and equipment, the risk of complications after tooth extraction surgery has been minimized in recent years.
X-ray
If, after the operation, the patient has complaints about the remaining tooth fragment in the socket or the development of exostosis, the first thing the doctor should do is to refer the patient for an x-ray examination. The image will clearly show the size of the bone, its shape and location. According to the results obtained, the doctor, using specialized devices, can begin the operation. Next, he extracts the remaining parts using tools, followed by processing the cavity.
Atrophy of the jaw bone tissue after tooth extraction and in various diseases: can it be restored?
Extraction is considered a last resort in dentistry. It is used in cases where other types of treatment or solutions to the problem are ineffective. Such an intervention involves not only the extraction of one of the elements of the dentition, but also injury to the mucous tissue, periodontal ligament, blood vessels, nerves and other structures.
Before performing the intervention, the doctor must carefully examine the patient and check whether there are any contraindications to the operation. Be prepared for the fact that you will need to take an x-ray before the intervention - this is necessary for the doctor to assess the condition of the roots.
How to behave correctly after tooth extraction surgery? How does healing occur, what does its quality depend on, and is it possible to speed up the process? The answers to these and other popular questions regarding tooth extraction are in our article.
After surgical removal of a tooth, a hole is formed in its place - a hole, which is gradually covered with tissue. Normal healing stages are as follows:
- formation of a blood clot (occurs 2–4 hours after removal);
- appearance of granulation tissue (3–4 days later);
- formation of bone tissue (after 1–2 weeks).
If you have a wisdom tooth removed, complete healing usually occurs in about a month. This is due to the fact that these teeth often have atypical root shapes, and operations to remove them are generally more traumatic than interventions on other parts of the dentition. Sometimes the roots of a tooth cannot be completely removed.
The time it takes for the gums to recover after tooth extraction will depend on how severely the tissue was injured during the operation. If the operation was complicated and stitches were required, the wound will bother you for about a week - usually the stitches are removed around the 7th day.
They can be quite strong. In this case, it is recommended to take painkillers and anti-inflammatory drugs (for example, Nimesil, Ibuprofen, Ketanov). The pain may be aching, pulling, throbbing - this is normal. Usually the pain syndrome completely disappears in 2–4 days.
During the first week after the intervention, it is recommended to carefully monitor your condition and, at the slightest suspicion of complications, consult a doctor.
Bleeding
In addition, bleeding may be present. Typically, a blood clot begins to form quickly enough, so that in the vast majority of cases, blood does not enter the oral cavity from the postoperative socket. In some cases, the dental surgeon installs a special self-absorbing sponge in the hole.
If swelling is observed after tooth extraction, there is no particular cause for concern: slight swelling is quite normal. But if the swelling increases, severe pain is present - this may already indicate the development of inflammation. It usually occurs if, after surgery, you accidentally damage a blood clot that has formed in the wound.
We suggest you read: Sour taste in the mouth: what causes the disease, treatment of high acidity in the mouth after eating
In this case, the hole remains open and infection can get inside. You should not hesitate to contact the dentist - the consequences can be serious. The doctor will examine you, clean the wound if necessary, treat it with antiseptics and prescribe antibiotics.
Severe swelling, in which not only the gums inside, but also the cheek swells, is a reason for an immediate visit to the dentist. A cheek tumor occurs when there is severe inflammation and pus formation. If you do not intervene in time, additional complications may develop.
If you have a fever after surgery, you should immediately consult a doctor. As a rule, this indicates infection of the postoperative wound. In some cases, this is how inflammation of the gums manifests itself. A sharp increase in temperature may indicate the development of serious complications.
In this case, it will be necessary to clean the cavity from pus in an office setting, treat it with antiseptics, and then carry out antibiotic therapy.
Alveolitis
Typically, alveolitis develops as a result of exposure to opportunistic flora, this is possible even if the tooth extraction operation was carried out flawlessly.
The occurrence of alveolitis can be facilitated by:
- chronic inflammatory lesions in the oral cavity;
- severe tissue trauma during surgery;
- impaired blood clot formation;
- the presence of chronic severe diseases.
The complication must be treated immediately after it has been diagnosed. In some cases, it is enough to treat the wound with an antiseptic composition. In more severe situations, antibiotics may be required.
This complication after tooth extraction can occur immediately after surgery or within a few days after it. Gum bleeding is associated with factors that cause vasodilation, as well as with trauma to the socket. In addition, the cause may be: damage to the gums, fracture of part of the alveoli, damage to blood vessels.
Treatment depends on the location of the problem: if the edges of the wound are bleeding, sutures are placed on them; if blood comes from a vessel in the hole, a tampon with a hemostatic compound is used.
Paresthesia
A rare complication caused by nerve damage during surgery. The main symptom is numbness in the cheeks, tongue, lips. As a rule, this phenomenon is temporary and harmless, disappears in a period of several days to 1–2 weeks.
In addition, the following problems sometimes occur:
- damage to adjacent teeth (chips, fractures);
- incomplete tooth extraction (in this case, a small part of the root remains in the jawbone);
jaw fracture (rare, usually associated with concomitant chronic diseases - for example, osteoporosis in older women).
Difficult removal may result in severe soft tissue damage. However, they usually heal fairly quickly.
Another complication can be considered a violation of the order of adjacent teeth. After removing any element of the dentition, the rest inevitably begin to shift. As a result, crowding of teeth or, conversely, unaesthetic “gaps” may form.
Gradually, the bone tissue at the site of the operation becomes thinner, and restoration of the lost tooth becomes problematic. That is why it is necessary to make maximum use of tooth-preserving technologies. If surgery cannot be avoided, it is worth considering the option of immediately installing an implant - this way you can restore not only the original appearance of the jaw, but also its full functionality.
After surgical tooth extraction you cannot:
- taking medications that interfere with normal blood clotting:
- Eating hard foods and sticky foods that can get into the wound:
- smoke and drink alcohol;
- visit the sauna and bathhouse.
Also, you should absolutely not rinse the tooth after extraction - this can damage the developing or already formed blood clot.
You can: eat soft pureed food, taking extra care not to touch the gums, engage in usual activities, brush your teeth (but being extremely careful, trying not to touch the damaged area).
The doctor will announce detailed recommendations and precautions that you will have to follow in the coming days after the operation after it is completed. Try to strictly follow them - this way you can protect yourself as much as possible from unpleasant consequences.
Tooth extraction is a surgical procedure and can lead to general discomfort and individual reactions of the body. If preventive measures are followed, the wound heals in a short time and health improves in 2-3 days.
- reduces bleeding;
- prevents bacteria from entering the wound;
- participates in the formation of new tissue at the site of removal.
Do not scrape or try to remove the clot!
In the coming days, the composition of the contents of the hole will change and thicken, forming gum tissue. On day 4-5, the color of the edges will change to pale pink. The middle has a yellow tint, which is normal. After 2-3 weeks, the hole disappears almost completely.
In order for healing to proceed naturally and without complications, it is necessary to follow the rules of prevention for the extracted tooth, aimed at timely stopping bleeding and preserving the protective clot.
If treatment is not timely, suppuration develops, spreading into the surrounding soft and bone tissue. The risk of spreading infection increases due to improper prevention during wisdom teeth removal. Complications of alveolitis have serious consequences for the patient’s health, so it is better to start treatment at the first signs of inflammation.
Prevention of alveolitis after tooth extraction involves:
- compliance with hygiene rules;
- maintaining the integrity of the clot in the hole;
- preventing the penetration of bacteria.
The wider the jawbone at the location of the tooth, the more tissue and nerve endings are affected during extraction. For this reason, the removal of front teeth is easier than operations on teeth located in the posterior extended part of the jaw. Most often, long-term pain persists after surgery on wisdom teeth. At the same time, the removal of lower wisdom teeth is more traumatic, since in this place the jaw has its maximum width.
Tooth extraction always takes place under anesthesia. The surgeon selects the optimal dosage of the drug, so in most cases the procedure is painless for the patient. As the anesthetic drug is removed from the body, pain appears in 2-4 hours at the site of removal and surrounding tissues. The intensity of pain depends on:
- type of extracted tooth;
- complexity of the operation;
- compliance with doctor's recommendations;
- individual characteristics of the patient.
As a rule, the pain is aching in nature and intensifies only with mechanical impact. If the tooth was removed with inflamed gums, the pain will be more pronounced.
As the wound heals, the pain subsides and ceases to bother the patient. A little pain during the week is normal. To prevent pain after tooth extraction, painkillers with anti-inflammatory effects are prescribed: ibuprofen (Nurofen), nimesulide (Nise, Nimesil).
- tooth loss is the main cause of loss of bone structure quality;
- inflammatory diseases of the gums lead to weakening of the connective tissues that hold the teeth in a stable state; in advanced forms, the teeth become loose and fall out;
- cystic and purulent formations on the roots of teeth, inflammation of the maxillary sinuses - the infection “eats” and “liquefies” the bone tissue;
- anatomical structure of the jaw and diseases of the bone structure;
- congenital disorders of the structure and growth of the jaw;
- Previously, dentists, after tooth extraction, practiced strong squeezing of the edges of the socket to speed up the healing process and close the resulting cavity from infections; today, surgeons have abandoned this technique, because mechanical compression in the area of a lost tooth leads to damage (compression) of bone tissue and the formation of a so-called narrow alveolar ridge;
- Jaw injuries and knocked out teeth lead to problems with bone tissue in 90% of cases.
We invite you to familiarize yourself with the dynamics of socket healing after tooth extraction on days 3-7: photos, stages and care
Prevention
According to dentists, it is almost impossible to prevent the development of exostosis, therefore the main preventive measures are aimed at identifying the disease in the initial stage of development.
For this purpose, it is necessary to regularly examine the oral cavity using a small mirror for damage to the mucous membrane, swelling and growths.
With thoroughly washed hands, you can palpate the gum tissue of the jaw rows, palate and floor of the mouth.
If palpable tumors are detected, you must immediately contact your dentist for a professional diagnosis.
In addition, you should not neglect regular dental examinations , during which a specialist can detect existing problems of the jaw rows, soft and bone tissues, and also take timely measures to eliminate them.
Do's and Don'ts after surgery
Normally, the wound heals in a few weeks, but it happens that this process takes longer. This happens in the following cases:
- wisdom tooth removal;
- dissection of the gums during surgery;
- bone injury;
- socket infection.
In these cases, the epithelium may appear only after a month and a half. If the wound was stitched, then the stitches were removed, the drainage was removed, and the wound was washed with medications, then regeneration would take even longer and be more difficult. It should also be remembered that gums in children and young people heal much faster than in older people.
Bleeding
Socket bleeding can be early or late. Early appears within a few hours, later - after a day or more.
Causes:
- A few hours after a visit to the dentist, bleeding may begin if the doctor used adrenaline. When it stops working, the vessels dilate and the wound begins to bleed;
- if the patient violates the surgeon’s recommendations, touches the wound, presses on it with his tongue, late socket bleeding is possible.
Most often, the complication is associated with additional injuries (damage to the gums, tissue infection, vascular damage), less often it is provoked by general, systemic diseases (hypertension, metabolic and blood clotting disorders, sepsis, other serious conditions).
If alveolar bleeding does not stop within a few hours or appears again and again, treatment is needed. If the soft periodontal tissues are damaged, additional sutures are placed on the edges of the wound. If blood vessels are damaged, the wound is cooled and local medications with hemostatic agents are used. It is possible to use medications that increase blood clotting (if local remedies do not help).
We invite you to familiarize yourself with 10 reasons for the appearance of cracks in the corners of the mouth.
Why does bone tissue atrophy?
The most common cause of jawbone atrophy is aging. However, there are other factors that contribute to bone loss even in young people:
- Inflammatory processes of gums, periodontium, maxillary sinuses, cysts, granulomas
- Damage to the jaw, wearing dentures for a long time
- Thyroid diseases, ovarian dysfunction in women
- Vitamin D deficiency
- Side effects of certain medications, such as glucocorticoids
- Congenital jaw pathologies, structural features of the jaw, tendency to atrophic processes
When a person chews food, blood circulation is activated and living tissues function normally. After tooth extraction, blood circulation is disrupted and the bone mass begins to decrease in volume. Over the year it decreases by an average of 25%.
Why does the jawbone shrink?
When a person has all the teeth in the mouth, the chewing load is evenly distributed throughout the entire alveolar ridge (that is, pressure is received by the gums, ligamentous apparatus and directly the bone in which the tooth roots are located). This is a natural process through which bone cells receive nutrition and metabolic processes occur in them. And thus the bone maintains its volume.
In cases where a tooth is removed, the bone tissue no longer receives load. When chewing, all the pressure is redistributed between the remaining teeth. Therefore, the nutrition of tissue cells is disrupted, which leads to its resorption. And gradually atrophy of the jaw bone tissue occurs.
Bone loss is also affected by other dental problems, such as inflammatory processes (cysts, granulomas, periodontitis and periodontitis). In these cases, tissue resorption occurs as bone cells are replaced by others.
There are other reasons that lead to bone thinning:
- individual structural features of the maxillofacial apparatus,
- genetic predisposition,
- getting jaw injuries,
- age-related changes in humans and natural aging of all organs,
- prosthetics that rely only on the gums (removable) or on living teeth (bridge), due to which the bone again does not receive the necessary load,
- inflammation of the mucous membranes, periodontal tissue diseases.
Our jawbone consists of several sections: the central one is the spongy layer. It contains tooth roots. This section is the most porous, since it is in it that a large number of capillaries are concentrated, which means that it is the spongy section that undergoes atrophy first. Below it is the basal layer - it is already stronger, since it consists of bone partitions and there are several times fewer capillaries in it. Both layers are covered by a shell or cortical plate - it, like the basal layer, is very dense and does not undergo atrophy.
Further, already behind the basal section, on the upper jaw there is a zygomatic bone, as well as buttresses - these are lines of force that evenly distribute pressure on the jaw between all the bone tissues of the skull.
We suggest you read: What a wound should look like after tooth extraction
On the upper jaw, the sinuses are located close to the jawbone. They have a rather thin shell, which can be easily damaged if implants are too long1. There are no sinuses on the lower jaw - the chin and jaw bone go under the alveolar process. They are very durable, so tissue atrophy below is less common, and implantation is easier.
Is it possible to restore bone tissue?
Modern dental technologies make it possible to restore deficient bone mass. The most effective method is surgery. There are also special medications that slow down the process of bone loss. However, the drug method is not effective in all cases.
If atrophy develops as a consequence of another disease, then it is necessary to treat it first. Problems are treated with hormonal drugs; vitamin D deficiency is treated by taking this vitamin in the right doses. Such therapy stops the process of bone loss, but cannot restore the lost bone volume.
In modern dentistry, there are several methods of bone tissue augmentation.
If atrophic processes have already begun, then the bone volume may not be enough to fix the implant. In this case, you have to resort to bone augmentation. There are several extension methods.
- Sinus lift. It is done only on the upper jaw. The bottom of the maxillary sinus is raised slightly, and bone chips are placed into the opened cavity. After surgery, an implant can be installed
- Osteoplasty. A small piece of bone tissue is taken from the patient and transplanted to the desired location. Your own biomaterial can be replaced with donor or even artificial one. The operation does not take much time, and the risk of tissue rejection is minimal
- Bone block transplantation. If there is a need to grow a large area of bone, then the patient’s bone taken from the chin, palate or lower jaw is used as the material. It is also possible to use donor or artificial biomaterial. However, with this method of extension it is impossible to immediately place an implant.
- Tissue regeneration. The essence of the technique is to grow the desired area of bone tissue. A special membrane is implanted into the patient's jaw to create a cavity in which bone tissue will grow.
It is not possible to increase lost gum bone tissue using folk remedies, but there are auxiliary preventive methods:
- Brushing teeth with calcium. Dilute a calcium tablet in a drop of boiled water and apply the resulting paste to your teeth using a toothbrush.
- Soda paste - a thick paste of soda and water - helps restore the alkaline environment, improves blood circulation in the gums and gets rid of bacteria.
- Salt paste: hold in mouth for 30 seconds and rinse mouth with warm water. Then apply calcium paste to your teeth, and propolis paste on top of it.
- Saline and soda solutions for rinsing teeth in a ratio of 100 g of salt or soda per 1 liter of water. Rinse several times a day after meals.
Treatment of seals
Therapeutic procedures can be very different, depending on where the compaction is located and what type it belongs to.
- The fistula is eliminated by treating the oral cavity with a soda solution. It helps wash away purulent discharge. The procedures are carried out until complete resorption.
- Periodontitis is treated by opening the filling and treating the area of inflammation with antiseptics. After this, the patient is prescribed a course of antibiotics.
- Epulis is eliminated by curettage. If the pathology has reached an irreversible stage, then the teeth that became the root cause of the disease are removed.
- The flux is removed by opening, after which the cavity is cleared of suppuration. If the tooth affected by the flux was exposed under the crown, then it is also removed for the duration of the therapy.
Opening an abscess
What is the probability that the bone material will not take root?
The risk of osteoplasty failure is 1-2%. This is a standard surgical risk. You can increase the chances of success if you heal diseased teeth and gums and do professional hygiene before surgery. Caries, periodontitis and tartar serve as a source of pathogenic bacteria that can provoke rejection of bone material.
In the postoperative period, it is important to maintain normal hygiene and not smoke. Smokers have impaired tissue regeneration processes, so they have the highest risk of rejection of not only bone materials, but also implants.