Jaw dislocation is a persistent displacement of the articular head of the lower jaw beyond its anatomical boundaries. As a result of such an injury, the function of the temporomandibular joint (TMJ) is severely impaired: speech becomes slurred, teeth do not close together, and often it is completely impossible to open the mouth. In addition, the configuration of the face noticeably changes: the chin “goes” to the side, uncontrollable salivation occurs - and all this is accompanied by pain.
Jaw dislocation is much more common in women, which is explained by the structural features of the female jaw joint - the shallow depth of the articular cavity, the relatively small size of the tubercle and the weakness of the surrounding ligaments.
Causes
The lower jaw is the only part of the skull capable of movement. The upper jaw is absolutely motionless, so it is not subject to dislocation. The lower jaw bone on both sides is equipped with articular heads placed in the fossae of the temporal bones. Inside the TMJ there is a disc that fuses with the synovial capsule and divides its cavity into 2 sectors.
The temporomandibular joint is extremely mobile, allowing a person to speak and chew food freely. The lower jaw can actively move in the vertical plane and partially in the horizontal.
Jaw dislocation occurs when the head of the joint falls out of the notch of the temporal bone. If this is repeated two or more times, they speak of a habitual dislocation. If the articular head does not fully emerge from the fossa, subluxation of the TMJ is diagnosed.
In most cases, the cause of injury is an external force or a sudden and unsuccessful movement of the jaw itself. For example, while yawning, laughing, vomiting, trying to eat a large piece of food. Sometimes such damage occurs during medical procedures - removal and treatment of teeth (especially those located at the end of the jaw), taking impressions. Bone displacement is also possible during gastric FGS, bronchoscopy, and tracheal intubation.
There are often cases when patients turn to doctors who have damaged their jaw due to opening bottles or other packages with hard lids with their teeth. Sometimes a subluxation in the joint is caused by chewing nuts.
The cause of an acute traumatic dislocation can be a direct blow to the face or a fall landing on the chin. Pathologically repeated and habitual dislocations are observed in patients who suffer from epilepsy, articular pathologies (arthrosis, arthritis, gout), as well as in a number of other cases.
These include:
- jaw deformation;
- malocclusion;
- stretching of the synovial capsule of the joint;
- weak ligaments that strengthen the mandibular joint;
- flattening of the articular surface of the head of the TMJ and a decrease in the height of the articular tubercle;
- joint hypermobility;
- absence of most teeth.
Often the cause of habitual dislocation is incorrect or too rough reduction of an acute dislocation, violation of the immobilization regime - for example, in the case of premature removal of the fixing bandage.
Important: the risk of dislocating the lower jaw increases with age, when the ligamentous apparatus weakens and metabolic processes slow down.
Causes of damage to the lower jaw
A number of reasons can provoke a dislocation of the lower jaw:
- Falling forward or backward when struck.
- Excessive expansion of the oral cavity during certain medical procedures in dentistry or surgery.
- Awkwardness of movements when yawning, shouting, singing, laughing and chewing food, especially hard food.
- Congenital joint anomalies, neoplasms, bone metastases.
- Malocclusion.
- Diseases leading to degeneration: arthritis, in particular rheumatoid. Arthrosis.
- Excessive muscle contraction during an epileptic seizure.
- Sprain.
Risk factors: changes in bone and connective tissue due to age or increased stress on the joint.
Types and classification
Jaw dislocations are classified according to the direction of displacement of the articular head relative to the socket, the causes of occurrence, the severity and duration of the damage.
Jaw arthritis
According to this classification, dislocations are:
- In front of them;
- rear;
- lateral;
- traumatic (primary);
- habitual (secondary);
- simple;
- complicated;
- sharp;
- outdated.
In addition, the dislocation can be unilateral or bilateral, but in most cases there is a bilateral lesion. A dislocation that occurred no more than a week ago is considered acute. A dislocation that occurred more than 14 days ago is considered old.
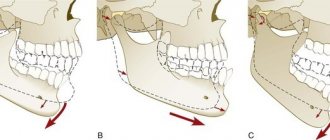
A simple dislocation does not entail damage to surrounding structures - skin, soft tissue, blood vessels or ligaments. If such damage exists, the dislocation is considered complicated. In practice, anterior dislocations and subluxations are most often observed, when the head of the joint is partially or completely displaced forward.
Important: in some cases, there are no visual signs of dislocation, and displacement of the bones can only be assumed based on the patient’s subjective sensations.
Methods of reduction and rehabilitation for jaw dislocation
Among the pathologies associated with the maxillofacial region, jaw dislocation has always stood out, since this problem can affect absolutely any person, regardless of age, gender and other factors. Most often, women under 40 years old face this problem, because their mandibular bursa is characterized by shallow depth, and the articular apparatus of the fairer sex is far from strong. Note that such displacements of the lower jaw occur in only 2-4% of all dislocations.
The anatomy of the jaw region is simple: the upper jaw is fixed, so it cannot move, and the lower jaw is mobile, which is ensured by joints and muscles. This structure allows a person to chew, as well as perform many other actions, for example, communicate.
Symptoms
With an anterior dislocation in one or both joints, severe pain occurs on the side of the jaw (or on both sides), the mouth does not close, and the patient practically cannot speak. The shape of the face changes due to protrusion of the chin forward and flattening of the cheeks. Both active and passive movements in the joint are impossible. Pressing the chin from below only causes springy resistance in the jaw and increased pain. With unilateral dislocation, attempts to slightly bring the jaws closer to each other are sometimes successful.
Posterior dislocation is accompanied by similar symptoms, to which is added difficulty swallowing and impaired respiratory function. The leading symptom is pain near the ears, and the patient takes a forced position, tilting his head to his chest. It is noticeable that the lower jaw “goes” back, and the lower front teeth rest against the palatine vault. Sometimes bleeding occurs due to damage to the wall of the ear canal.
If the injury is repeated, that is, the dislocation is habitual, there is a misalignment of the lower jaw, the joint hurts and clicks when moving. Complicated dislocations are characterized by such signs as swelling of soft tissues, bruises and bruises, and possible disruption of the integrity of the bones forming the mandibular joint (in case of fracture-dislocations).
Diagnostics
Determining a reliable diagnosis is very often difficult for the reason that patients go to the dentist with the disease in an advanced state, when the root cause of the disease is almost impossible to establish.
Clicking may be accompanied by other symptoms, including morning soreness, joint stiffness, discomfort when moving the mouth, and sometimes pain at rest in the event of the development of purulent-inflammatory complications.
Differential diagnosis is carried out when clicking occurs as a symptomatic manifestation of the following diseases:
- dysfunctional disorder of the TMJ – this diagnosis is awarded to the patient’s dentist if the sound occurs during chewing. This is not a disease, but only a pathological condition in which the joint has certain structural abnormalities. A common sign of dysfunction is headaches that occur due to excessive muscle tension;
- arthritis is an inflammatory lesion of the joint, leading not only to pain, but also to structural damage in case of untimely treatment. Often occurs against the background of a previously occurring purulent-inflammatory process in the body (otitis, purulent tonsillitis or other processes in the oral cavity);
- pathological occlusion - clicks especially often occur during progeny, when the body of the lower jaw protrudes forward and the lower teeth overlap the upper teeth. This mutual arrangement of the jaws affects the structure of the joint, while the head of the lower jaw is located on the slope of the tubercle, and not in its proper place - the articular fossa;
- Arthrosis is a dystrophic disease with a chronic course that develops over a long period of time. In this case, pain and pathological noises occur in the morning, while the joint is not yet developed. By evening, the mobility of the lower jaw increases, and symptoms may disappear.
DETAILS: Impingement syndrome of the knee joint
If the clicking does not stop, you need to do something urgently. The first thing you need to do is consult a doctor, preferably an orthodontist, he will help assess the severity of the situation and first identify the causes.
It can be difficult to immediately unmistakably understand the causes of disturbances in the functioning of the TMJ, especially if patients consult a doctor in advanced cases. Therefore, the orthodontist will most likely give referrals to other specialists - a dentist, a gnathologist, perhaps a surgeon - to conduct a full examination.
The most common diagnostic procedures are carried out in the following order:
- careful questioning of the patient;
- palpation of the painful area;
- studying the characteristics of the bite, the condition of the teeth;
- taking blood tests to identify possible infections and inflammatory processes;
- ultrasonography;
- electromyography of the jaw;
- neurological research;
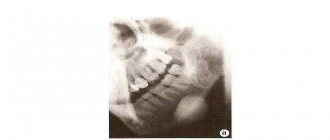
- X-ray;
- arthroscopy;
- MRI or computed tomography.
The most important thing is to determine whether it is mechanical damage to the TMJ and its components, or a bone disease - arthrosis or chronic arthritis.
Which doctor should I go to?
If your jaw is dislocated, it is best to contact the Department of Oral and Maxillofacial Surgery. The scope of activity of a surgeon of this specialization includes the correction of congenital and acquired facial deformities. Oral and maxillofacial surgeons realign the jaw and perform surgery if necessary. Surgical intervention is often required for chronic and habitual dislocations.
If an injury occurs during dental procedures, assistance is provided by the attending physician. If a dislocation occurs at home at night, you need to call an ambulance. The ambulance will take the patient to the nearest emergency room, where they can determine the type of injury by taking an x-ray and put the jaw back in place.
Methods of reduction and rehabilitation for jaw dislocation
Among the pathologies associated with the maxillofacial region, jaw dislocation has always stood out, since this problem can affect absolutely any person, regardless of age, gender and other factors. Most often, women under 40 years old face this problem, because their mandibular bursa is characterized by shallow depth, and the articular apparatus of the fairer sex is far from strong. Note that such displacements of the lower jaw occur in only 2-4% of all dislocations.
The anatomy of the jaw region is simple: the upper jaw is fixed, so it cannot move, and the lower jaw is mobile, which is ensured by joints and muscles. This structure allows a person to chew, as well as perform many other actions, for example, communicate.
Treatment
In most cases, making a diagnosis is not difficult, since there is a characteristic deformation of the face, and the displaced bones can be easily felt. However, it is necessary to take an x-ray to exclude a fracture of the condylar process, which is located at the base of the temporomandibular joint. In difficult cases, magnetic resonance imaging (MRI) or computer imaging (CT) is prescribed.
Treatment always begins with reduction of the dislocation using one of the following methods:
- Hippocrates;
- Khodorovich;
- Blekhman-Gershuny;
- Popescu.
Most often, doctors use the Hippocratic method. Regardless of the chosen technique, anesthesia is given so that the person does not feel pain. The patient is seated on a low seat with a high back, which is necessary to support the back of the head. Before the procedure, the doctor wraps his hands in a thick layer of gauze, then grabs the lower jaw so that his thumbs are placed on the chewing teeth.
Smoothly pressing his fingers on the teeth, the doctor with a precise movement “pushes” the jaw back (in case of posterior dislocation, forward), while managing to remove his fingers in time. When the articular surfaces of the bones align, a click is heard.
After reduction, immobilization of the jaw is necessary to prevent relapse; for this purpose, a sling-shaped bandage is used. If with an anterior dislocation you need to wear such a bandage for no more than a week, then a posterior dislocation requires longer immobility - up to three weeks. The patient is recommended to eat only soft and pureed food, which is best taken warm.
If it is impossible to straighten the jaw due to structural abnormalities in the joint, surgery is performed. It is sometimes possible to treat old dislocations received more than two weeks ago only after removing the articular heads. In this case, special dentures are installed that prevent the mouth from opening too wide and can be removable or non-removable.
In case of habitual dislocations, the purpose of surgical intervention may be to strengthen the ligamentous apparatus, deepen the articular fossa, increase the height of the articular tubercle, and also reduce the cartilage disc.
The operation to reduce the dislocation is performed under local or general anesthesia
It is worth noting that the displacement of the cartilage disc can be reducible or non-reducible. In the latter case, the only treatment method is arthroscopy. During arthroscopic surgery, accumulated fluid is removed and the joint is washed with saline.
Then a revision of the damage is carried out: compression of nerves, blood vessels and soft tissues is eliminated, and the cartilage disc is repositioned and fixed. Having fixed the disc, the joint space is widened using galvanization, after which the torn vessels and synovial capsule are sutured.
Classification
Jaw dislocations are divided into different types:
- According to the location of the articular head:
- Front. In this case, the articular head begins to be located above the capsule. Injuries of this type occur in the vast majority of cases.
- Rear. With a posterior dislocation, it is displaced beyond the capsule.
- Lateral. Lateral disturbances, which are the least common, involve displacement away from the depression in question.
- By the nature of the displacement:
- One-sided. As the name implies, in this case only one articular head is displaced, that is, on one side of the jaw.
— Double-sided. In the same case, both joints change their position.
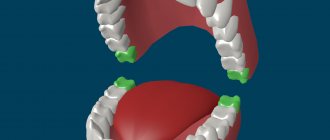
- According to the completeness of the dislocation:
- Full. The contact between the surfaces of the joints is completely disrupted, that is, the entire head extends beyond the boundaries of the fossa.
- Incomplete (another name is subluxation). Such an injury involves partial preservation of the connection between the articular surfaces.
- By severity of injury:
- Simple. A dislocation of this kind assumes the absence of any other disorders; there are no injuries to the skin, as well as tendon ruptures, damage to blood vessels and soft tissues.
- Complicated. Such an injury is much more serious, it may imply the presence of any of the disorders that were listed earlier.
The most common cases are jaw subluxations or anterior bilateral injuries. We also note that with regular displacements of this kind, the problem can become chronic, as a result of which the articular head begins to come out of the fossa for no apparent reason.
Treatment at home
You can straighten the jaw yourself using the Blechman-Gershuny method. This technique is taught to patients suffering from habitual dislocation. To return the jaw to its place, you need to press on the articular head in the posterior-inferior direction. Reduction occurs quite quickly and relatively painlessly. The alignment of the bones is indicated by a characteristic click. This way you can straighten your jaw yourself.
If the reduction is done by a relative or a doctor, then the impact on the displaced articular heads can be carried out from the inside. By placing the thumbs in the oral cavity, simultaneous pressure is applied to the edges of the lower jaw in a downward and backward direction.
Help with dislocation
Resetting a dislocated jaw yourself is much more risky than dislocations of other joints - any careless movement can lead to even more severe damage.
Therefore, it is best to consult a doctor in such a situation. However, if this is not possible (or you yourself have the appropriate skills), you can use one of the methods to return the joint to its place.
Correction of dislocation
There are three joint reduction techniques:
- the method of Hippocrates;
- Blekhman - Gershuni method;
- Popescu method.
Hippocrates' method
This technique is used for uncomplicated dislocation.
- The victim must be seated on a chair or armchair with a headrest - during the reduction process, the head must rest on a hard surface. The level of the victim's jaw should correspond to the level of the doctor's elbows.
- Local anesthesia is administered. To do this, an injection of novocaine, lidocaine or another pain reliever is given.
- The doctor disinfects his hands and wraps his thumbs with thick cloth, bandage or gauze to avoid injury.
- The doctor places his thumbs on the patient’s molars, and uses the remaining fingers to secure the lower jaw.
- Then direct reduction is carried out: the jaw is carefully moved slightly downward, while at the same time pressure is applied to the chin in the upper direction - this is done in order to relax the masticatory muscles. After this, the jaw moves back and then immediately upward: thus, the head of the joint returns to the notch. If all manipulations are carried out correctly, a characteristic click will be heard - this means that the jaw is in place. Immediately after this, the jaw will reflexively close, so it is important for the doctor to quickly remove his fingers from the teeth, moving them to the inner surface of the cheeks.
Blechman-Gershuny method
This method is the simplest and fastest, but it requires coordination and care, since it must be performed literally in one movement.
It is used for uncomplicated bilateral dislocations.
- First, the doctor feels the coronoid processes of the jaw bone near the arches of the cheekbones.
- Then, in one movement, the bone moves down and back - until a characteristic click occurs.
The jaw can be adjusted in this way from the inside (the coronoid processes are felt from the inside of the oral cavity) and from the outside. Reduction from the outside is considered an easier method, although it takes some skill to quickly find the coronoid processes.
The Blechman-Gershuny method is recommended for use for regular uncomplicated dislocations caused by ligament weakness or shallow depth of the articular fossa.
Popescu method
This method is the most radical and effective, but also the most risky - it should only be performed by a person with professional skills. When performed correctly, the Popescu method can correct even an old dislocation.
- The patient is placed horizontally on his back.
- Local anesthesia is administered in the area of the affected joint or, if necessary, general anesthesia.
- Between the molars of the patient's upper and lower jaws, rollers of bandage with a thickness of at least one and a half centimeters are installed.
- The doctor presses the chin upward and backward with force. Reduction is performed in one motion. After this, the joint should snap into place with a corresponding click.
Treatment after reduction
After realignment of the jaw, the joints require rest and some therapy.
To avoid repeated dislocation, the jaw is fixed with a special bandage, the so-called. sling-shaped, covering the lower jaw and fixed in the crown area. Splints can also be used for fixation.
Pain will persist for some time after the joint has been realigned - this is quite normal. They can be removed with the help of non-steroidal anti-inflammatory drugs (Diclofenac, Ibuprofen, Ketorolac). You can also apply cold compresses to your jaw.
During the recovery period, it is extremely important to be careful and not to put excessive stress on the joint - do not eat dense foods, which, when bitten, will put a large load on the joint; do not open your mouth too wide; If possible, reduce jaw mobility to a minimum. The rehabilitation period is approximately 2-3 weeks.
A dislocated jaw is not as rare an injury as you might think. It occurs quite often, and, unfortunately, it is very easy to earn it. Like any dislocation, it needs to be set as soon as possible, however, unlike the joints of the arms and legs, setting the jaw on your own is a more difficult and risky task. You can do this only if you can’t see a doctor and the situation is critical. Then the skills to independently reduce a dislocation may be useful to you.
Preventive measures
Treatment of habitual dislocations necessarily includes correction of the underlying disease that led to joint instability. According to indications, selective grinding of teeth, installation of dentures, and blockade of masticatory muscles are prescribed. Physiotherapy procedures - electrophoresis, galvanization, therapeutic exercises for facial muscles and massage - have a good effect.
To prevent re-injury, you must wear a fixing bandage for the period recommended by your doctor. Loading the jaw too early can lead to stiffness of the joint or the development of habitual dislocation.
Timely correction of the bite and installation of dentures will help to avoid jaw dislocation. This is especially important if a large number of teeth are missing. Special care is also required when chewing and in situations that require wide mouth opening.
What kind of sound is produced?
Clicking can vary in nature and volume. Based on the intensity of the sound, the condition is divided into three main types: a light click, which is felt only by the patient himself, a click of medium intensity, or a very strong, pronounced click that is heard by others, sometimes even by a person standing far away.
There is also a classification that divides the problem according to the immediate moment when the click occurs: it can occur during the opening of the mouth or during the process of closing and closing the jaws.
- If a click occurs when you open your mouth, it can happen with a small opening or with an intense opening.
Clicks that appear with a small range of mouth opening are usually quiet, dull, but very frequent and occur, as a rule, with arthritis, when the meniscus becomes thinner or an inflammatory process develops.This process is usually accompanied by swelling, as well as loosening of the ligaments. Sometimes local fusion of the jaw joint with cartilage occurs. Then, when opening, a sound resembling a crunch occurs.
- If the click occurs when the mouth is half or fully open, then we are most likely talking about serious changes in the articular head.
Most likely, this is a sign of arthritis, and often in an advanced state. During diagnosis, defects in the head, meniscus or cartilage may be detected. The entire joint capsule can participate in this process. - If a click is heard when the mouth closes, a sprain or problem with cartilage tissue may be diagnosed.
There can be two varieties here: when the mouth is open wide and closing has just begun, or when the process of closing the mouth is already at the very end. In the latter case, clicks most likely indicate dislocation due to malocclusion or chronic problems with teeth or their artificial substitutes.
DETAILS: Production of hip joint endoprostheses
If a dull pain occurs when you click your jaw, this most likely indicates mechanical problems with the joint. If the pain is acute or increasing, which is accompanied by swelling, then the problems are more serious - we are talking about inflammation, intra-articular or even bone changes.
It is much worse if the pain does not have an exact localization: when there is a sensation of ringing in the ears, painful sensations radiating to the ear or teeth, or spreading to the temple, neck, back of the head and even to the scapular part of the back - all this can complicate an accurate diagnosis.
Especially often, with TMJ diseases, headaches occur, usually in the temporal or occipital part. The pain can be so severe that even an experienced doctor may suspect migraine and other problems associated with the blood vessels of the brain.
Failure to see a doctor in a timely manner can not only result in a protracted search for the true cause of the pain, but also aggravate the situation, leading to the following consequences:
- neuralgia of the facial muscles;
- joint dislocation, the occurrence of chronic defects;
- disc tear or damage;
- arthrosis of the lower jaw;
- gradual destruction of the joint, up to complete.
If the disease is neglected, the treatment will be delayed and will be not only more expensive, but also less effective, with inevitable side effects.
If you feel severe pain when clicking, this may be a clear symptom of arthritis. Arthritis is an internal infection of the joint followed by acute inflammation. Infection can occur in a variety of ways, including through injury, and can destroy tissue.
Destruction can transform arthritis into a chronic form and even lead to ankylosis - a complete disruption of the motor function of the lower jaw.
As mentioned above, if clicks occur when you open your mouth and are more like a crunch, this is precisely a sign of the likelihood of incipient arthritis.
The pain that occurs during the opening process naturally intensifies as you chew food and apply pressure to the area. In addition, the painful area becomes red and swollen because inflammation has already begun.
There is also a sensation of the jaw shifting to the side. All this is often accompanied by dizziness, fever and lethargy. If the inflammatory process is aggravated by suppuration, hearing deterioration and even partial loss may occur.
When things have gone this far, surgical intervention is indispensable. After the operation, the patient must wear a specially made sling-shaped bandage for some time and keep the plate between the teeth.
In addition to a strict diet of liquid dishes, antibiotic therapy and regular physiotherapy are prescribed. Therapeutic exercises and massage are started after the bandage is removed.