- Home /
- Articles /
- Osteotomy as a special case of osteoplasty
Osteotomy is a surgical operation aimed at eliminating deformity or eliminating anatomical and functional disorders by artificially breaking the bone and correct fusion. This operation is performed to treat both congenital and acquired pathologies, for example, in case of improperly healed fractures.
Osteotomy is a surgical operation aimed at eliminating deformity or eliminating anatomical and functional disorders by artificially breaking the bone and correct fusion. This operation is performed to treat both congenital and acquired pathologies, for example, in case of improperly healed fractures.
Indications for osteotomy:
- improperly healed bone fractures;
- ankylosed joints;
- change, shortening of the limb;
- rachitic curvatures;
- formation of a false joint;
- osteomyelitis;
- osteoarthritis, spondioarthrosis;
Depending on the surgeon’s goal and the patient’s clinical picture, the following types of osteotomy can be performed:
- wedge-shaped;
- linear (oblique and transverse);
- hinged (can be arc-shaped, that is, made in one plane, or angular, spherical - in several planes);
- staircase;
- Z-shaped;
- derotational.
By purpose they are distinguished:
- Corrective osteotomy - to correct deformity after complications that led to malunion.
- Hinge osteotomy is an operation to lengthen the limbs.
Osteoplasty techniques are also divided into closed and open. The first is performed with minimal access, through a 2-3 cm incision. The open method involves wide access - an 8-12 cm incision is made exposing the bone. In some cases, when there is a risk of damage to nerves and large vessels, preference is given to open osteotomy, despite its low invasiveness, over closed one.
The choice of method depends on the type of pathology, volume and area for surgical intervention - pelvis, jaw, hip, etc. Most often, the operation is aimed at restoring the function of the musculoskeletal system and removing bone deformations.
To equalize the lengths of the lower extremities, osteotomy is performed according to the principle of oblique cutting of the bone in mandatory combination with extrafocal compression-distraction osteosynthesis. The design for osteosynthesis is selected individually for each patient.
What is the role of osteotomy in dental practice?
Osteotomy is a type of operation that is performed on one of the patient’s jaws, and in some cases on both.
As a rule, osteotomy is prescribed when there are serious bite pathologies, disturbances in the development of the jaws, or in order to eliminate the results of an unsuccessful operation in the treatment of palatal clefts. In the lower jaw, surgery is often performed after injury.
Types of osteotomy:
- fragmentary;
- general.
All the defects mentioned above significantly disfigure a person’s appearance, which means they turn into a source of permanent complexes and contribute to the development of serious diseases, for example:
- respiratory dysfunction;
- diseases of the jaw joints;
- diseases of the digestive system.
For this reason, timely corrective surgery on the jaw can greatly improve the patient’s quality of life.
Why is osteotomy needed?
Bite anomalies are congenital or acquired. Such violations only in rare cases do not cause any negative consequences. In most patients, malocclusion is caused by:
- decreased self-esteem due to unattractive appearance;
- the development of various dental problems caused by constant trauma to the mucous membrane (due to malocclusion, the teeth regularly touch the back of the cheeks);
- respiratory dysfunction;
- problems with the digestive system that arise due to insufficient chewing of food;
- diseases of the jaw joints;
- pathologies of the maxillary sinuses and more.
Having a malocclusion significantly complicates a person’s life. Osteotomy can prevent the development of the above consequences.
Indications and contraindications for intervention
This operation is performed in the following cases:
The photo shows the patient's face before and after jaw osteotomy
- violation of the closure of the dentition, which cannot be eliminated using orthodontic methods and structures;
- obvious facial disproportion, intolerable from an aesthetic point of view.
There are cases when osteotomy cannot be performed. Such an operation is never prescribed for minor children, since their bone tissue formation is still ongoing.
Other reasons for refusal to implement this intervention:
- lack of preparation of the dentition;
- various infectious diseases;
- poor blood clotting;
- presence of diabetes.
It must be clearly understood that the main purpose of corrective osteotomy is to correct the position of the jaw and eliminate bone deformities.
She will not be able to change the initially incorrect position of the teeth. For this reason, before prescribing surgery, the doctor may recommend straightening the dentition using braces, tooth extraction, prosthetics, correction of lateral bands and other procedures.
What is a knee osteotomy?
Corrective osteotomy of the knee joint is an operation that eliminates congenital and acquired bone deformities. During surgery, the doctor excises a pre-designated area of bone tissue and connects the loose bone fragments with implants. As a result, the axis of mechanical load is transferred to the healthy area of the joint. The operation is performed under complete or spinal anesthesia. After treatment, the orthopedist immobilizes the patient's lower limb with a plaster cast during recovery. Rehabilitation is underway.
Osteotomy with metal structure.
The described correction method is traditionally compared with knee replacement. Osteotomy is a less traumatic treatment method. This medical procedure is perfect for young patients suffering from late stages of gonarthrosis. The choice of osteotomy as a method of restoring mobility of the lower limb makes it possible to delay endoprosthetics for a long time.
Osteotomy has been used for two centuries. After the discovery of replacement arthroplasty methods, this surgical intervention faded into the background, but this method of treatment is still used. At the beginning of the 21st century, modern methods of fixing bone areas were developed, reducing the duration of rehabilitation.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Preparing for surgery
Before performing the operation, it is necessary to prepare the dentition. This is done through the use of braces or prosthetics or implantation.
Sometimes surgical preparatory and preventive interventions can also be performed:
- tooth extraction;
- crown exposure;
- correction of lateral bands and frenulums and other procedures.
What is corrective osteotomy
Corrective osteotomy is used to restore the function of the musculoskeletal system and eliminate deformation of large joints. During the operation, a part of the bone is excised, it is given the correct shape, and reverse fixation is carried out with a special apparatus for osteosynthesis, as well as with the help of plates and screws. To align the upper and lower limbs, in some cases they resort to shortening one of them. In this case, excision of a certain bone fragment is performed, followed by osteosynthesis.
After the operation, plaster bandages are applied. Sometimes they are replaced with knee pads with the ability to regulate range of motion, which reduces the risk of developing contractures in the joints.
The need for corrective surgery arises in the following cases:
- malunion of supramalleolar fractures (corrective osteotomy in the tibia);
- valgization and varus deformity (scarf technique is indicated);
- ankylosis of the hip joint;
- previous polio (correction of the subcondylar region);
- joint contracture;
- gonarthrosis;
- malunion of supracondylar fractures.
Indications for corrective osteotomy of the foot and 1st metatarsal bone are impaired fusion of bones after a fracture and severe arthrosis.
Carrying out the intervention
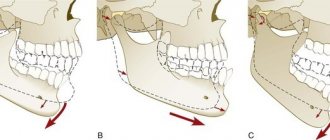
Features of osteotomy depending on the operated jaw.
On the lower jaw
Osteotomy of the lower jaw is performed through intraoral access, which will prevent the formation of scars on the facial skin.
The mucous membrane and periosteum are incised in the projection of the pterygomaxillary fold, and the transition to the outer surface of the body of the lower jaw is taken into account. The boundaries of the incision are expanded, which helps create comfortable access to the lower jaw.
Using a special saw, the surgeon cuts through the compact plates in the mandibular branch, after which its fragments are separated. Similar actions are performed on the second side.
After the bilateral osteotomy is completed, the jaw is placed in the already defined position.
The final stage consists of fixing the jaw fragments in their current position with special titanium clamps and screws.
For a month after the intervention, some swelling of the soft facial tissues will be observed. In addition, there may be a decrease in sensitivity in the area where the intervention was performed, which will disappear on its own after up to six months.
In some cases, in order to guarantee a successful outcome of the operation, the specialist performs splinting using mini-implants - the jaws are securely attached to each other, so the patient cannot open his mouth too wide. At this time, he will only be able to eat liquid or grated food.
On the upper jaw
Endotracheal anesthesia is used for this procedure. The oral mucosa and periosteum are incised just above the fold of the maxillary junction. The boundaries of the wound are expanded for better access to the jaw.
Markings of the cut boundaries are placed on the front and lateral jaw walls on the left and right sides.
Using a special file, osteotomy is performed according to the markings.
The sawn fragment is separated and placed in a predetermined position. The fragment is fixed with titanium miniplates.
Possible complications:
- wound infection;
- displacement of bone tissue fragments;
- too slow bone healing;
- paresthesia - decreased sensitivity of the skin in the area where the operation was performed.
Surgical interventions on the body of the lower jaw
SURGICAL INTERVENTIONS ON THE BODY OF THE LOWER JAW
The purpose of surgical interventions in this area is to eliminate deformation, expressed in excessive lengthening of the body of the lower jaw, especially in the horizontal region. A.E. Rauer proposed bilateral osteotomy of the horizontal part of the body of the lower jaw with resection of bone segments at the level of the 6-7th tooth and preservation of the neurovascular bundle (Fig. 97, 98).
Under endotracheal anesthesia or conduction and infiltration anesthesia, the body of the jaw (right and left) is exposed through an incision in the submandibular region, and the lower 6|6 or 7|7 teeth are removed in the predetermined osteotomy area. 3-4 mm above the lower edge of the lower jaw, the mandibular canal is opened with a grooved chisel, the neurovascular bundle is isolated and, to protect it from injury, it is raised upward on a hook. After this, pieces of bone are cut out in the area of the removed teeth so that the ends of the bone fragments have a stepped shape. After a bilateral osteotomy, the ends of the bone fragments are brought together, they are positioned along the bite and fixed with a wire suture or dental splints with intermaxillary traction. The fixation of the fragments is very reliable, since the stepped shape of the cut allows the fragments to be closely connected. In addition, the posterior fragment cannot move upward due to the fact that a protrusion remains on the posterior fragment.
A. Ya. Katz proposed performing a compatosteotomy of the lower jaw, which is used in cases where previous orthodontic treatment did not give the desired effect. In the area of a certain part of the body of the lower jaw, the cortical plate is removed from all sides on both sides, after which intermaxillary traction is applied (Fig. 99).
V. A. Bogatsky recommends performing a stepped osteotomy at the level of the rudiments of the 8th teeth, followed by their removal and resection of a section of bone in this section. The fragments are fixed either with splints and rubber rings, or with a wire suture, or with plastic.
Surgical interventions on the branches of the lower jaw. The essence of all operations in this area is to dissect the branch at different levels and shift the body posteriorly. Osteotomy of the branch is performed horizontal, oblique or stepped.
In 1924, Kostechko proposed to perform horizontal osteotomy of the branches of the lower jaw without incision of soft tissues—“blindly.” Under local anesthesia, moving down from the earlobe by 0.5-0.6 cm, an injection is made with a Kerper needle and advanced along the inner surface of the lower jaw branch, all the time feeling the bone, towards the lower edge of the zygomatic bone. The needle is poked out in the cheek area under the cheek bone. With this advancement, the needle passes above the mandibular foramen and lateral to the neurovascular bundle. After the tip of the needle is exposed from the puncture, one end of the Gigli saw is strengthened in its eye and the needle and saw are pulled in the opposite direction. Handles are put on the saw and the jaw branch is sawed. The direction of the cut should correspond to the plane of the bite. The same is done on the other side. The lower jaw is moved posteriorly, set in the correct bite position and fixed to the upper jaw using wire splints and an intermaxillary rubber rod for up to 2 months.
The operation is technically easy to perform, but is not always successful, since in the postoperative period it is difficult to prevent the displacement of the small bone fragment with the articular process upward and inward under the influence of the temporal and lateral pterygoid muscles. As a result, the bone fragments do not fuse, a false joint is formed, and after surgery an open bite often forms. Damage to the neurovascular bundle and facial nerve is sometimes observed. These disadvantages have recently forced many surgeons to abandon its use.
Anesthesia during surgery
A more favorable course and outcome are observed with horizontal osteotomy of the mandibular ramus according to Limberg or with oblique sliding osteotomy of the jaw ramus.
Horizontal osteotomy of the mandibular ramus. Under endotracheal or conduction and local anesthesia, the masticatory muscles (m. masseter et pterygoideus medialis) are removed from the submandibular incision and the branch of the lower jaw is exposed from the outside and inside. A horizontal osteotomy is performed above the mandibular foramina. After displacing the body of the lower jaw and establishing the correct bite, the excess posterior edge of the ramus is resected in order to eliminate its pressure on the soft tissues and form the angle of the lower jaw. Fixation of fragments is carried out using intraoral splints with an intermaxillary rubber rod.
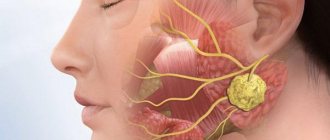
Oblique sliding osteotomy of the mandibular ramus. Under endotracheal anesthesia or conduction and infiltration anesthesia, the periosteum along with the masticatory muscle is separated from the bone to the mandibular notch from the submandibular incision. The masticatory muscle and parotid salivary gland with the surrounding soft tissues are raised upward as much as possible to provide a good view and access to the outer surface of the branch. The sharp angle of the chisel is used to mark the line of osteotomy of the branch, which should run from the middle of the mandibular notch to the angle of the jaw or slightly posteriorly and above it. The outer and inner compact plates are cut along the intended line with a fissure bur. In this case, the mandibular foramen, together with the neurovascular bundle entering it, remains in front of the osteotomy line on the anterior fragment. For better mobility of the inner surface, the posterior fragment is freed from muscles and ligaments to the base of the articular process, brought outward and placed on the outer surface of the anterior fragment. A similar operation is performed on the other side.
After this, the anterior fragment of the jaw is moved back until the teeth align in the correct bite. In this new position, the fragment is fixed to the upper jaw using dental splints and rubber rings. Then they begin to fix the bone fragments. To apply a wire suture, a hole is drilled on the front fragment, and a notch (notch) is made on the rear edge of the small fragment. The lower end of the posterior fragment, protruding outward in the form of a sharp spike, is smoothed with bone pliers, the masticatory muscle is sutured to the internal pterygoid muscle at the lower edge of the lower jaw. The wound is sutured in layers. Fixation of the jaws lasts 5-6 weeks.
In 1957, Obwegeser used the method of stepwise longitudinal osteotomy of the mandibular ramus from an intraoral approach. The internal cortical plate is cut midway between the semilunar notch and the mandibular foramen. On the outer cortical plate, the cutting line runs 1 cm above the lower edge of the angle of the mandible. The cortical plates are separated, then the lower jaw is moved posteriorly, the teeth are aligned in the correct bite and fixed with dental splints and a rubber rod. The fragments are fixed with wire sutures (Fig. 100).
To increase the contact surface between fragments according to the author’s method, the lower cut of the outer cortical plate is made not horizontally above the angle of the jaw, but vertically between the 7th and 8th teeth to the base of the lower jaw. Surgery can be performed either externally or intraorally. The method is technically difficult, but due to the large contact area, the consolidation of fragments occurs faster. The method is more reliable in terms of preventing relapses.
Vertical wedge-shaped osteotomy of the mandibular ramus according to Van Zil, modified by Rudko. The operation begins in the same way as an oblique osteotomy. However, after cutting the bone, small fragments are not brought out, but a second cut of the bone is immediately made and the wedge-shaped section of the lower jaw branch is removed. The width of the base of the triangular section of bone excised from the branch is calculated in advance using models. The fragments are fixed with bone sutures. The soft tissue wound is sutured in layers. The lower jaw is fixed with wire splints with intermaxillary elastic traction.
An open bite is a type of jaw deformation in which, during closure of the teeth, occlusal contact is observed only up to the first molars. Lack of closure in the area of the front teeth causes cosmetic and functional defects: the mouth is open, the tongue is visible between the teeth, the lower part of the face is excessively large. The speech of such patients has a lisp, and the efficiency of chewing is sharply reduced. An open bite occurs due to the influence of all those causes that cause deformation of the jaws (rickets, improperly healed jaw fractures, etc.). Open bite accounts for 1.3% of facial bone deformities.
To eliminate an open bite, depending on the nature of the deformation, surgical interventions are performed more often in the area of various parts of the lower jaw. If rearrangement of the entire body of the mandible is necessary, the most appropriate method is bilateral oblique osteotomy of the mandibular ramus according to Limberg. Under endotracheal anesthesia or conduction and infiltration anesthesia, the branch of the mandible is exposed using a submandibular approach, the muscles and periosteum are peeled off, and an osteotomy line is drawn from the middle of the semilunar notch of the mandible towards the posterior edge of its branch. The bone is sawed with a bur or broken with a chisel. After osteotomy, the jaw is moved to the correct position and fixed in the position of normal occlusion with wire dental splints with intermaxillary traction. The jaw fragments are fastened with a wire suture.
Another operation proposed by A. A. Limberg for severe forms of open bite and mild progeny consists of bilateral wedge-shaped resection of the alveolar process in combination with vertical osteotomy of the jaw body. Under endotracheal anesthesia or conduction and infiltration anesthesia, the mucous membrane in the area of the 5th, 6th and 7th teeth is dissected with a trapezoidal incision. The 6th tooth is removed and in this area a wedge-shaped section of bone tapering downwards is cut out from the alveolar process of the lower jaw. The apex of the cone should reach the mandibular canal. Through an external incision, a vertical osteotomy of the body of the lower jaw is made, keeping the neurovascular bundle intact. The cutting line should start from the top of the triangle and reach the edge of the body of the lower jaw. After mobilization of the anterior fragment, it is moved to the correct position and secured using pre-applied wire splints with an intermaxillary rubber rod. The wound from the oral cavity is sutured with catgut sutures. To prevent relapse, it is recommended to insert an allograft (bone, cartilage) in the form of a spacer into the wedge-shaped bone defect that forms after displacement of the anterior fragment along the lower edge of the lower jaw. The soft tissue wound is sutured in layers. Fixation of the lower jaw continues for 2 months. The method gives good long-term results.
Branch osteotomy with skeletal traction of the mandible
A. Ya. Katz proposed performing compactosteotomy (decortication) of the lower jaw in cases where previous orthodontic treatment did not give the necessary effect in the treatment of open bite. The method is based on the principle of weakening the resistance of bone tissue by removing the cortical layer in those places where the bend is supposed to occur, and eliminating the existing deformation by moving the anterior section using elastic traction. The operation is performed under conduction and infiltration anesthesia.
From the vestibule of the oral cavity and from the alveolar process in the area of the 5th and 6th teeth, trapezoidal incisions of the mucous membrane are made. The mucoperiosteal flap is peeled off and the 5th or 6th tooth is removed. Then, using a bur or chisel in this area, the cortical layer of bone is removed from the outer and inner sides of the body of the lower jaw for at least 1 cm and along the entire vertical line of the body of the jaw. The mucoperiosteal flap is placed in place and fixed with catgut or silk. The same operation is performed on the other side. Elastic traction is applied to pre-installed wire splints with hooking loops, which is reinforced by applying a chin sling or Urbanskaya bandage. Elastic traction lasts 2-2.5 months.
M.V. Mukhin suggested crossing the piece through a small incision. digastricus, geniohyoideus, genioglossus to prevent relapse of open bite. In cases where the deformity is noted in the anterior region, the bevel starts from the first premolar or canine and the body of the lower jaw does not need correction, osteotomy and relocation of the alveolar process without compromising the integrity of the base of the lower jaw according to Babitskaya are indicated.
Under bilateral conduction and infiltration anesthesia, an incision is made into the mucous membrane. The mucoperiosteal flap is peeled off. One of the premolars is removed from both sides and the outer and inner walls of the sockets of these teeth are resected. Using a bur, mark the line of osteomia along a horizontal line 10-15 mm below the apexes of the roots of the teeth and use a chisel to separate the alveolar process. At the same time, the connection with the soft tissues on the inside must be maintained. The mobilized area of the alveolar process is moved to the correct position and secured using pre-applied wire splints. During surgery, care must be taken not to damage the neurovascular bundles of the anterior teeth. In case of a massive and elongated chin, the chin is corrected simultaneously or at the next stage, removing excess bone.
Macrogeny is an excessive enlargement of the lower jaw or one half of it with a normal size of the other. In contrast to true progenia, with unilateral macrogenia, an increase in the size of the lower jaw branch is observed, sometimes especially large growth in the area of the articular process. When: in this case, the jaw moves forward and a sharp shift of the chin to the opposite side is noted. The contours of the face are distorted, the bite and chewing function are disrupted. The etiology of the disease is not clear. A sudden increase in height in some cases appears between the ages of 18 and 30 years. In some cases, phenomena of gigantism in other parts of the body are observed.
When diagnosing macrogenia, especially in cases of hypertrophy of the articular process, it should be differentiated from deformation of the articular head due to any pathological processes (deforming arthritis, etc.).
Treatment for macrogenia is only surgical. In case of unilateral macrogenia, a unilateral resection of the articular condylar head with part of the condylar process is performed, preserving the meniscus and part of the articular capsule. If necessary, the edge of the jaw in the area of the corner is simultaneously resected.
V.F. Rudko recommends not resecting the condylar process, but performing a wedge-shaped osteotomy of the mandibular ramus on one side. This eliminates deformation and preserves the integrity of the temporomandibular joint.
Microgenia is a unilateral or bilateral underdevelopment of the lower jaw, characterized by shortening of the branch or body. Unilateral microgenia develops most often as a long-term consequence of osteomyelitis of the lower jaw in the area of the angle and branch during the growth period, resulting in delayed growth of the jaw branch, deformation and underdevelopment of the condylar process. Sometimes the cause of microgenia is purulent otitis with the transition of the process to the articular head, as well as injury to the condylar process or articular head during childbirth or in childhood. This type of jaw abnormality is sometimes associated with heredity. Microgenia is often combined with ankylosis of the temporomandibular joint. Clinically, microgenia without ankylosis of the temporomandibular joint is characterized by facial asymmetry due to displacement of the chin towards shortening of the jaw. When you open your mouth, your chin moves further to the side. The tissue on the affected side appears more convex, while on the healthy side it appears flattened. With bilateral microgenia, the chin moves back, sinks, the entire lower part of the face is reduced, as a result of which a facial disfigurement develops, known as “bird face” or “pitcher snout”. With pronounced microgenia, the bite is disturbed. The dentition of the normal upper jaw is compensatoryly rebuilt due to the deformation of the dentition on the affected side of the lower jaw. The act of biting and chewing food is difficult.
Bone grafting of the mandibular ramus with allograft
In cases where the shortening of the jaw is insignificant, the asymmetry of the face is not very pronounced, the upper teeth are in good contact with the lower teeth, the indication for surgery is only cosmetic requirements. In such cases, operations are performed that change the external contours of the face, or so-called contour plastic surgery. To eliminate the asymmetry of the outer integument of the face on the flattened side, under local anesthesia, allogeneic tissues of appropriate size and shape are transplanted.
In recent years, the method of contour plastic surgery with crushed auto- or allocartilage, which is injected through a needle using a revolving syringe into the tissue without dissection and detachment according to the Limberg method, has become widespread.
Biologically inert plastics can be used for contouring.
In cases of severe deformation and underdevelopment of the lower jaw, various surgical interventions are performed depending on the size of the branch or body of the jaw. Radical treatment of microgenia consists of three stages: 1) surgical correction of the position of the lower jaw by osteotomy, followed by orthopedic fixation of the jaw in a new position; 2) orthodontic correction of teeth bite and the shape of the upper jaw; 3) operations to correct facial asymmetry (contour plastic surgery, plastic surgery using local tissues). Treatment ends with dentures.
Lengthening the jaw body or ramus can be accomplished by plastic osteotomy or osteotomy followed by replacement of the defect with freely grafted bone. In most cases, when eliminating severe forms of microgenia, patients need repeated surgical interventions, sometimes with quite significant intervals between them. Step osteotomy operations have been developed to lengthen the ramus or body of the lower jaw.
Step-shaped osteotomy on the jaw branch according to Rudko. Under endotracheal anesthesia or conduction and infiltration anesthesia, the branch of the mandible on the shortening side is exposed from the submandibular incision. A step-like osteotomy is performed at the border of the upper and within its middle third. The lower jaw is pushed forward and placed in the correct position. The bone fragments are fixed in close contact with each other with a wire suture. The wound is sutured in layers. A bandage and chin sling are applied.
Step-shaped osteotomy on the body of the lower jaw according to Svistunov. Under endotracheal anesthesia or conduction and infiltration anesthesia, the body of the lower jaw is exposed through a submandibular incision on the affected side. A circular saw is used to cut the compact plate and cancellous bone to a depth of 2-3 mm from the outside of the jaw in the form of a step from the middle or posterior third of the body of the lower jaw to the canine or second incisor (the tooth is first removed) below the mental foramen. The length of the horizontal cut depends on the size of the extension required. Then the compact plate and spongy substance are dissected along the lower edge of the jaw according to the length of the first horizontal cut. On the vestibular and lingual side of the alveolar process, trapezoidal incisions are made in the mucous membrane in the area of the socket of the extracted tooth. The mucoperiosteal flaps are peeled off and, using a Gigli saw, the internal cortical plate is dissected to the anterior end of the cut along the lower edge of the jaw and at the same time the spongy substance within the height of the alveolar process (in the area of the socket of the extracted tooth).
After this, using a flat chisel or a rasp through the slit of the cut of the cortical plate along the edge of the lower jaw, with careful rotational movements, the jaw is separated into two fragments consisting of spongy substance, the inner and outer cortical plates. With this technique, the neurovascular bundle and teeth are not damaged. After moving the jaw fragments into the required position, the bone segments are fixed with a wire suture. Wounds from the oral cavity and submandibular region are sutured tightly. To prevent possible displacement of the bone fragments of the lower jaw, they are fixed to the upper jaw with wire splints with intermaxillary traction for 10-14 days. These operations are indicated if the required lengthening does not exceed 1-2 cm, and if the bone thickness is sufficient. If there is a sharp thinning of the body of the lower jaw, it is lengthened by vertical osteotomy, followed by bone grafting of the resulting defect after separation of the fragments of the lower jaw.
Currently, one-stage free plastic surgery of the lower jaw is used with “lightweight seedlings” in the form of the outer half of the rib, which have good plasticity and the ability to engraft. The operation of free bone grafting for microgenia of the lower jaw consists of three main stages: 1) taking and preparing a seedling; 2) vertical osteotomy of the lower jaw and separation of fragments to the required distance; 3) introducing a graft into the wound and securing it. A prerequisite for a successful outcome of the fragment operation is reliable fastening of the mandibular fragments. Currently, a method of securing segments of the lower jaw with one-stage osteoplasty for microgenia with a steel bone frame on screws has been introduced into practice. With the help of bone plates, long-term stable fixation of the lower jaw is ensured, there is no need for additional immobilization of the lower jaw, and postoperative care of the wound and oral cavity and feeding of patients are facilitated.
With osteoplastic lengthening of the lower jaw, the disturbed facial proportions are restored, but malocclusion remains due to secondary deformation of the upper jaw and movement of the lower jaw. After some time, this disorder is corrected using orthodontic methods, and in some cases, using compactosteotomy of the upper or lower jaw.
Compact osteotomy of the upper jaw. Under local anesthesia, an incision is made in the mucous membrane to the bone in the vestibule of the oral cavity from the lateral incisor to the last molar, exposing the anterior wall of the upper jaw and the alveolar process. Using a round bur in a checkerboard pattern at intervals of 2-3 mm, holes are drilled through the entire thickness of the compact layer of bone. The largest number of indentations is applied in areas where the compact layer is most pronounced: in the area of the pyriform opening, the base of the zygomatic process, above the roots and along the sockets of the teeth to be moved. After this, the mucosal wound is sutured tightly. Then an incision is made in the mucous membrane of the hard palate, 2-3 mm away from the necks of the teeth to be moved. The mucoperiosteal flap is peeled off to the midline and multiple depressions are also made on the alveolar process in the area of the indicated teeth. Then the detached flap is placed in place, sutured with 2-3 sutures and pressed with a tampon soaked in iodoform and a protective plate. The tampon and plate are removed on the 8th day after surgery.
Lattice compactosteotomy of the lower jaw. Through a submandibular incision made 1-3 cm below the edge of the jaw on the shortening side, the outer and inner surface of the jaw body is exposed in the area from the lateral incisor to the angle of the jaw. Using a round bur, multiple depressions are made in the compact layer of bone throughout its entire thickness, and through cuts are made along the edge of the jaw. The wound is tightly sutured and a pressure bandage is applied. Orthodontic treatment begins after 12-16 days, when the plasticity of bone tissue noticeably increases.
Management of the postoperative period in each case depends on the method of operation. Each operation ends with the application of intermaxillary traction using rubber rings on the toe loops of the tires. To avoid the formation of bedsores, it is necessary to ensure that the hooks do not put pressure on the mucous membrane of the gums, cheeks and lips.
The patient is placed in a bed with the head end raised, in a semi-sitting position. This position makes breathing easier and prevents the development of asphyxia from tongue retraction. Anti-inflammatory therapy is prescribed. The next day, the first dressing is done: the rubber graduates are removed and the wound is cleaned. The sutures are removed on the 7th day. It is necessary to clean the oral cavity daily, irrigate 6-8 times a day, monitor the correct position of splints, rubber rings and the condition of the bite. Patients are on a tube diet. After osteotomy in the area of the jaw branch, fixation continues for 1.5-2 months. 4-5 weeks after the operation, the patient is allowed to remove the rubber rings from the dental splints while eating, irrigate the oral cavity after eating and put the rings back on. This should be done until a strong consolidation occurs. After the sutures are removed (on the 7th–8th day), a light aseptic bandage and Urbanskaya sling are applied to the chin and submandibular area. This sling is recommended to be worn for 1.5-2 months after removal of the intermaxillary fixation. At the end of this period, the patient can only wear the Urban sling at night.
Expected effect
After some time has passed after surgery, when the rehabilitation period is completed, patients note a clear positive result.
- Biting and chewing food becomes easier , which also affects the functioning of the digestive system.
- Teeth wear out and decay less , which is a very common occurrence in the presence of malocclusions.
- The patient’s appearance improves – the bite returns to normal, the jaw relationship becomes harmonious, and the smile becomes beautiful. A person’s self-esteem increases and he becomes more confident.
- The likelihood of developing diseases of the temporomandibular joint is reduced , as the volume of loads is reduced.
- If the problem is the result of an injury, surgery will help restore the previous appearance .
Osteotomy is a fairly popular and sought-after procedure precisely because of its effectiveness.
Rehabilitation
Long-term treatment results depend on rehabilitation measures. After surgery, the doctor conducts follow-up examinations and selects methods for restoring mobility of the knee joint. The goals of rehabilitation include pain relief, prevention of postoperative complications, and restoration of the muscular system of the lower extremity.
Rehabilitation methods:
- Physiotherapy: electrical stimulation, cryotherapy and heat. Physical therapy relieves pain and reduces tissue swelling in the postoperative period.
- Massotherapy. Manual therapy improves blood flow in tissues, relieves pain and normalizes muscle tone.
- Physiotherapy. Exercises can be done at home. The main task is to restore flexion and extension movements in the knee joint.
- Orthopedic rehabilitation to prevent relapse of the disease. The patient is advised to wear a knee brace or elastic bandage to secure the joint. For the first time after surgery, it is necessary to use a cane and wear shoes with orthopedic insoles to reduce the load on the articular surfaces.
The rehabilitation plan is drawn up by an orthopedist and a physical therapy doctor. Drug therapy is selected. Full restoration of motor activity occurs within a year.
Rehabilitation period
Although jaw osteotomy is a common operation, the rehabilitation period after it is quite complex and lengthy. Immediately after completion of the intervention, the patient is prescribed antibiotics to avoid infectious diseases. In addition, a tight bandage is applied, which can be removed only one day after the end of the operation.
The doctor installs special clamps to secure the position of the jaws, after which he must monitor both their location and the bite as a whole.
Until the retainers are removed, the patient cannot chew food, blow his nose, or open his mouth wide. The stitches will be removed approximately two weeks after surgery. The fixing screw will be removed by a specialist after three months. The next stage is orthodontic therapy.
Rehabilitation after osteotomy
Let's consider the recovery period after surgery using the example of corrective osteotomy.
The patient is in the hospital under the supervision of doctors for 3 to 7 days. At this time, regular treatment of the surgical wound is carried out, painkillers, antibiotics and anti-thromboembolism drugs are given. It is important to start getting up as early as possible and not to lie around.
After discharge, the patient must continue taking the prescribed medications at home. On the 10-14th day, the sutures are removed. Next, rehabilitation is indicated - the use of crutches for up to 6-12 weeks, regular visits to the doctor for examinations. Heavy physical activity will be allowed only 6-8 months after the operation. Sometimes installed metal structures are removed after 1-2 years.
Indications for use
Corrective osteotomy is recommended in the following cases:
- congenital deformation of the lower and upper limbs in a child;
- changes in the position of the joint and disruption of the structure of bone tissue due to previous diseases (rickets, Paget’s disease, osteoporosis);
- deformity due to growth disorders (Blount's disease);
- post-traumatic deformation;
- arthrosis of the knee joint;
- instability of the ligamentous apparatus of the knee.
Progress of the operation
The duration of the operation directly depends on its complexity, the condition of the patient and the specific part of the body that needs treatment. Modern types of intervention allow the procedure to be carried out in the shortest possible time - about 1-2 hours, but there may be delays of up to 3-4 hours.
The duration of the operation directly depends on its complexity
Preparation
The preparatory stage includes diagnostics, consultation with a therapist, surgeon and other specialists. Mandatory tests and an ECG, obtaining an X-ray or MRI image of the damaged area. It is usually recommended to fast for approximately 10 to 12 hours before the procedure. In addition, it is advisable for overweight patients to organize a diet several weeks before surgery.
Note! If a patient suffers from chronic diseases and takes medications on an ongoing basis, he must immediately inform his doctor about this. You may need to stop taking these medications for a while.
Technique
The intervention is always carried out under anesthesia and includes the following stages:
- Patient preparation, local or (more often) general anesthesia.
- Incision of soft tissues and spreading them to the sides using fixing elements.
- Bone cutting is an artificial fracture using an osteotome or chisel.
Osteotome is a special surgical instrument for cutting bone.
- Removal of damaged fragments (if necessary), replacing them with an implant.
- Correction of the shape of a bone fragment.
- Osteosynthesis is the fastening of parts using fixing elements (hinged osteotomy).
- Closing the wound, applying sutures.
How a jaw osteotomy is performed is detailed in the video:
Possible consequences and complications
As a rule, properly performed surgical intervention does not entail any serious complications. However, in some cases (up to 10%), undesirable consequences may occur, such as:
- bleeding in the wound;
- purulent skin lesions;
- penetration of infection;
- displacement of fragments;
- slow recovery of bone tissue;
- hematomas.
It is very important for the patient to carefully monitor his health and carefully follow the doctor’s recommendations. If pain occurs, severe swelling or other symptoms occur, the surgeon is immediately informed.
Features of the recovery period
The recovery period largely depends not only on the condition and age of the patient, but also on the type of intervention. For example, after a femoral osteotomy, a person can recover for 2–3 months or more. In this case, complete fusion of bone fragments after injury occurs no earlier than after 4 months (with a favorable course of the operation and the patient’s normal state of health - no more than 6 months).
Wearing a joint orthosis
For a successful recovery, you must follow the advice of doctors, for example:
- measured load on the damaged part;
- special diet;
- physical therapy exercises;
- massage sessions;
- physiotherapeutic procedures for accelerated restoration of bone tissue;
- taking medications for pain relief and recovery;
- wearing joint orthoses;
- use of technical means of rehabilitation.
Types of surgery
The following types of osteotomy are used:
- Z-shaped or scarf (for hallux valgus);
- wedge-shaped (correction of the axis of the phalanx of the finger);
- angular (excision of tissue at an angle to return the correct position);
- linear (alignment with a graft).
Osteotomy of the calcaneus for flat feet.
Depending on the access, the following two types of surgery are distinguished:
- Option using closed access. Allows you to correct the pathology through a 2 cm incision in the skin. The specialist works “blindly”, so this treatment option requires increased caution and often leads to complications.
- Open access option. This type is used more often. The operation is performed through a skin incision of up to 12 cm, which allows you to completely open the required area of the bone.
Quite often, the bones of the foot are subject to correction - the phalanx of the big right or left toe and the heel. This area bears a large load during recovery after a fracture of the bones of the lower extremities, which is fraught with improper healing. Surgical treatment is also prescribed for planovalgus deformities with severe valgusation, clubfoot, and flatfoot with complications.
Surgery on the knee joints is performed when severe deforming arthrosis develops. The severe consequences of this disease lead to disability and a sharp decrease in quality of life. To correct the disorder, installation of an implant is indicated; this treatment remains inaccessible to many patients due to its high cost. An alternative option is tibial osteotomy according to Ilizarov.
Hip surgery involves changing the configuration of the hip joint. In this case, surgeons strive to achieve correspondence between the surfaces of the femoral head and the acetabulum. Treatment of the hip joint using the Chiari technique is carried out for hip dysplasia in children (osteotomy with derotational varus) and coxarthrosis in adults.