Pain in the teeth is one of the most unbearable and can cause a person severe discomfort. If it is present, you need to contact a specialist as soon as possible, since you can lose your tooth, which can most likely be cured. In addition, you can start an inflammatory process with a wisdom tooth, which is quite problematic. In the future, undesirable consequences may develop, such as a hematoma after tooth extraction, and in addition, there may be swelling on the face or a bruise on the gum itself.
Socket with blood after tooth extraction
How to assess the risk: are complications after wisdom tooth removal dangerous?
Wisdom teeth (eights) are the last teeth in the row, the eruption of which begins in adulthood. During this period, soft tissues function worse, resulting in severe pain and inflammation.
When the discomfort becomes unbearable, the dentist recommends removing the tooth.
Also, indications for removal are: suppuration of the gums and jaw bones, injury to the enamel of adjacent teeth, incorrect position, pericoronitis (inflammation of the hood of the mucous membrane around the figure eight ).
Dislocations and fractures
Deep, rough or incorrect gripping of a wisdom tooth with dental forceps can lead to breakage of part of the interdental bone septum - the alveolar process. The patient can feel with his tongue the sharp edge of the bone where the removed third molar was located. The consequence is a long healing of the wound resulting from the removal of third molars.
Rarely, it is still possible to encounter fractures or dislocations of the jaw bone resulting from gross surgical intervention. Usually these are consequences of the removal of wisdom teeth in the lower jaw. It is the lower “eights” that often have a non-standard arrangement - they grow unevenly or cannot come out. We wrote about such phenomena in the article “Retention and dystopia of wisdom teeth.”
Jaw plates
Inexperienced doctors put too much effort into trying to pick out the intractable “eight”. This leads to a disastrous result, which can only be corrected by installing special tires or plates. Unlike beginners, professional dentists use other options for solving a problem instead of physical strength. For example, cutting a wisdom tooth into parts.
What causes complications after wisdom tooth removal?
Main causes of complications:
- the presence of carious formations in the oral cavity - because of this, pathogenic microorganisms begin to develop in the oral cavity;
- generalized caries;
- incorrectly selected hygiene products and irregular hygiene procedures.
In addition to the main dental factors leading to complications, there are other, secondary ones.
These include:
- hypertension;
- surges during stressful situations;
- fragility ;
- strenuous physical work.
Important! Bad habits, especially smoking and drinking alcohol, reduce the body's protective functions. Because of this, wounds in the oral cavity heal slowly , which sometimes leads to complications.
Consequences of unsuccessful extraction on the upper and lower jaws, treatment
At the first sign of complications, you should consult a doctor for advice and professional examination. The clinic will be able to prescribe the correct therapy.
How to treat osteomyelitis?
This is a purulent-necrotic process that affects bones and bone marrow, as well as surrounding soft tissue.
Rotting is caused by pathogenic bacteria and mycobacteria.
If during the removal procedure an infection got into the socket, or after the operation a blood clot did not form in the socket.
This will lead to inflammation in the periodontal and bone tissues of the jaw under the influence of harmful bacteria.
Over time, the inflammation will develop more and more and become purulent in nature, and it can spread to neighboring organs.
- pain in the area of the extracted tooth;
- temperature rise to 38 degrees and above;
- general weakness and malaise;
- headache, sleep disturbances.
Attention! Purulent formations worsen a person’s general condition, and in the absence of proper treatment, the outcome can be fatal.
If the disease is noticed in time, it can be treated quite quickly - it is enough to open the abscess and remove the lesion. After this, take a course of anti-inflammatory drugs.
Abscess
A tooth abscess is an infectious disease that affects the soft tissues of the oral cavity. Often inflammation begins at the root of the tooth.
An abscess develops due to a bacterial infection entering the body through damaged skin or mucous membranes.
- pain during eating;
- deterioration in general health;
- increased body temperature;
- development of tumors in the area of lymph nodes;
- violation of facial symmetry;
- formation of purulent foci in the oral cavity.
Sometimes the complication appears after a few days, and in some cases during the acute course of the disease - after a few hours.
If the disease is ignored, it can lead to the following consequences:
- meningitis;
- phlegmon;
- sepsis;
- cyst;
- brain abscess.
Paresthesia of the tongue
This complication is characterized by loss of sensitivity of the tongue. This occurs quite rarely, usually after complex operations.
If the affected area is large, the unpleasant symptom goes away after half a month, and if a small area is affected, sensitivity will return after 2-3 days.
If the oral cavity is in advanced condition, paresthesia will not go away without surgical intervention.
Main causes of numbness:
- improper location of the roots, severe inflammation, as well as proximity to nerve endings;
- dentist mistakes - if doctors have not studied the peculiarities of the location of the roots.
Neuritis
A disease that is characterized by pain, decreased or complete absence of sensitivity in the facial area, as well as impaired motor activity.
Neuritis appears for the following reasons:
- violation of the anatomical integrity of the nerve;
- exposure to toxins;
- vascular and metabolic changes.
- constant aching pain;
- loss of sensation;
- numbness of soft tissues and teeth.
Lack of treatment leads to facial distortion and muscle atrophy in the area of inflammation.
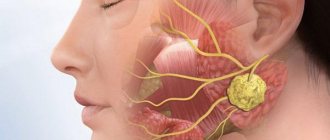
Cellulitis: photo of the disease
A disease that occurs due to the spread of infection in the soft tissues of the oral cavity.
Photo 1. An infection has spread in the soft tissues of the jaw, purulent inflammation begins - this is the most dangerous complication after tooth extraction.
The negative process leads to a delay in tissue formation, which causes the death of leukocytes and the development of purulent inflammation.
Most often, pathology manifests itself in certain areas:
- under the tongue;
- under the lower jaw;
- simultaneously both under the tongue and under the lower jaw.
In rare cases, inflammation can develop under the eyes or temples, as well as in the cheeks and palate.
Important! The disease is characterized by a high rate of spread to bone and muscle tissue, tendons and nearby organs.
- elevated temperature;
- pale skin;
- loss of appetite, general weakness of the body, headaches and sleep disturbances;
- inability to open the mouth completely;
- increased salivation;
- swelling and redness of the oral cavity.
Complications of phlegmon are purulent meningitis, as well as purulent arthritis and osteomyelitis.
Exostosis
Exostosis is growths that form due to the proliferation of osteochondral or bone tissue. Foreign bodies appear on the palate or lower jaw.
As the tumor grows, eating brings discomfort, diction worsens, and the bite changes.
- the appearance of a round lump on the palate or lower jaw;
- constant sensation of a foreign body in the oral cavity;
- pain in the area of the tumor;
- whitening ;
- the patient begins to lisp or “whistle”;
- the face becomes asymmetrical;
- in rare cases , jaw mobility deteriorates.
With the rapid growth of exostosis, there is a risk of it becoming malignant.
Neuralgia
Painful sensations that occur in the area of innervation of the nerve trunk or peripheral branch are referred to as neuralgia.
The disease is characterized by sharp, unbearable pain.
- headache;
- elevated temperature;
- distorted facial expressions.
The manifestation of neuralgia most often occurs in the following cases:
- when brushing your teeth;
- washing;
- applying makeup;
- shaving.
As soon as the disease begins to develop, it becomes difficult for the patient to smile, talk, open his mouth wide, and chew food. The disease causes muscle spasms, as well as a nervous tic in the affected area of the face.
Other complications: damaged or touched a nerve
Dry socket . This process occurs because the dentist used an anesthetic and vasoconstrictor drugs at the same time.
As a result, a spasm of the arteries occurs, and a blood clot, which is necessary for the natural healing of the wound, does not form in the hole.
To correct the situation, the doctor must slightly injure the gum, which will cause the hole to fill with blood.
- Pain in the area of the extracted tooth. It is normal to experience pain for 5 days after a dental procedure. However, if after the specified time the pain does not go away, this indicates the development of infectious diseases. Most often, this disease is alveolitis.
- Nerve damage . During the removal of the figure eight, the surgeon may damage nearby nerve fibers. Because of this, numbness occurs in the soft tissues of the oral cavity, and a person experiences difficulty opening the jaw. All unpleasant symptoms should go away in a maximum of two weeks.
Alveolitis
Alveolitis, or dry socket, is a problem in which a blood clot does not form in the socket of an extracted tooth. This clot is necessary for normal wound healing. If the clot does not appear or is washed out, it can cause inflammation and pain.
Causes of alveolitis
- Rinse your mouth in the first days after surgery;
- Smoking;
- Ignoring oral hygiene;
- Eating spicy, cold and hot foods after treatment;
- Complex operation;
- Doctor's mistakes;
- Serious pathologies of the body.
Alveolitis is the most common complication after tooth extraction surgery.
Symptoms of alveolitis
Alveolitis manifests itself as redness and inflammation of the gums. Sometimes a gray coating appears in the hole, and general health may worsen. If the problem is ignored, then pain occurs, radiating to the temple, headaches appear and the jaw ache. Sometimes the cheek swells.
Untreated alveolitis can easily cause dangerous diseases, such as osteomyelitis.
Treatment of alveolitis
Alveolitis is diagnosed very simply during a visual examination. To treat it, it is necessary to remove all foreign objects from the hole, perform an antiseptic treatment and close the hole with a swab with medicine. If the inflammation has spread further, it may be necessary to open the purulent foci. Additionally, medication and physical therapy can be used.
Osteomyelitis after tooth extraction
The main indicator of alveolitis is pain that occurs after a few days, which can greatly bother the patient.
Changes in the gums that occur with postoperative alveolitis
In addition, the following symptoms are present:
- swelling of the mucous membrane at the site of removal and local inflammation;
- there is no normal blood clot in the socket itself;
- temperature increase;
- difficulty swallowing.
This problem occurs if the healing processes are disrupted, which can be caused by non-compliance with the dentist’s recommendations after tooth extraction.
It may also be due to the surgical process being too difficult due to a particular tooth position or other factors.
As a result, pathogens from the oral cavity penetrate the open wound, triggering the development of alveolitis.
Another option is that the patient’s body is weakened by infection and cannot resist microbes.
If the pain and symptoms only get worse after 3 days, you should definitely visit the dentist. Most often, they are prescribed physical therapy along with general anti-inflammatory drugs and topical ointments.
What is osteomyelitis of the jaw
Osteomyelitis in dentistry is an inflammation of the jaw bone tissue of an infectious and purulent nature. The causative agents of the disease include:
- staphylococci;
- coli;
- tuberculosis bacillus;
- rickettsia;
- streptococci;
- Pseudomonas aeruginosa;
- Klebsiella;
- gram-negative bacteria;
- viruses.
The most common are streptococcal and staphylococcal infections of the jaw tissue. Often the disease leads to generalization of the infection, which causes infection of the entire human skeletal system and nearby tissues.
Osteomyelitis is a multifactorial disease, the likelihood of its development is influenced by:
- infection by pathogenic microorganisms;
- state of the immune system;
- disturbance of local blood circulation.
Damage to the maxillary sinus
But the consequence of removing a wisdom tooth in the upper jaw may be damage to the maxillary sinus. A hole (perforation) on its wall appears as a result of accidental pushing of the figure eight roots or penetration of a dental instrument. In the first case, only widening the hole will help. This will allow the third molar to be removed.
As a rule, these are all possible options that can await the patient while still in the dental chair. Fortunately, unsuccessful surgery can be corrected.
It is worth understanding that in certain situations, wisdom teeth removal is the only correct option. Refusal to undergo surgery may cause changes that are dangerous to the body.
Damage to the maxillary sinus
Causes
Jaw osteomyelitis occurs due to the penetration of pathogenic bacteria or viruses into the body. The further course of the disease depends on the state of the person’s immunity. If he is fine, then the disease enters the chronic stage or does not develop at all. But with immunodeficiency, the inflammatory process will begin to progress.
What diseases provoke osteomyelitis?
All causes of the development of osteomyelitis can be divided into several types:
The source of infection is a diseased tooth. Harmful substances enter the bone through the pulp when:
- pulpitis;
- alveolitis;
- periodontitis;
- tooth root cyst.
Pathogenic microorganisms enter the skeletal system from the primary source of inflammation:
- tonsillitis (chronic and acute form of the disease);
- furunculosis;
- otitis;
- scarlet fever;
- flu;
- omphalitis.
- jaw fractures;
- deep cuts;
- gunshot wounds;
- damage to the nasal mucosa;
- infection during surgery.
Treatment tactics depend on accurate diagnosis, but with any type of pathology, you first need to destroy the source of inflammation, and only then act on the organs and systems that have been infected for the second time. If the patient suffers from diabetes, pathology of the hematopoietic organs or cancer, the prognosis worsens.
Osteomyelitis after tooth extraction
Osteomyelitis can occur after tooth extraction. In this case, the infection enters the hole due to insufficient quality of treatment of the oral cavity. From the hole, pathogenic microorganisms penetrate into the bone tissue. One of the main signs of the disease is increased mobility of the teeth located next to the socket.
Osteomyelitis in the presence of milk teeth
A carious cavity in a baby tooth that is not treated in time can also cause the development of pathology. Moreover, the infection often destroys the rudiments of the main tooth, so if any problems appear with baby teeth, they must be treated quickly, and not hope that they will fall out soon. Milk teeth are also removed if they have become a source of inflammation in the body.
Bleeding
It also occurs quite often. Moreover, this can happen either immediately after the operation or an hour, several hours or even a day after it.
Bleeding from a tooth socket after surgery
The reasons for this may be some concomitant diseases (hypertension, leukemia, jaundice), as well as the actions of the dentist or the patient himself.
During the operation, the doctor may make some mistakes, for example, damage blood vessels, part of the alveoli or interradicular septum.
Also, bleeding from the socket occurs when it is mechanically damaged, which is the fault of the patient who did not follow the surgeon’s recommendations for rehabilitation.
To stop the bleeding, apply cold (ice) to the affected gum or cheek.
To avoid a general deterioration in health, you need to see a doctor as soon as possible.
Clear signs of a dry socket are:
- the absence of a visible blood clot in it, instead of which bone is visible;
- strong pain;
- inflammation.
The cause of this phenomenon may be the actions of the patient himself:
- Unnecessarily frequent rinsing after surgery;
- drinking “with effort”, for example, through a straw;
- periodic spitting.
For treatment, you must consult a dentist, who will recommend anti-inflammatory drugs, and in difficult cases, he will additionally clean the hole, cover it with a special gel, or prescribe antibiotics.
In a normal case, after the procedure, the hole should bleed for about 20 minutes. Minor bleeding can also be observed in the first few hours after the operation, but if it continues longer, or unexpectedly opens after a few days, then we can already talk about pathology. Very often, socket bleeding is a complication after wisdom tooth removal.
Socket bleeding is treated as follows:
- If blood comes from the soft tissue of the gums, then sutures are required;
- If a vessel is damaged, then ice is applied to it, and a hemostatic tampon is placed in the wound for five days;
- If all these measures do not help, then the patient is prescribed medications that accelerate blood clotting.
Types and symptoms of osteomyelitis of the jaw
The symptoms of the disease depend on the location of the source of infection, the type and form of the pathology. With osteomyelitis of the upper jaw, symptoms of the development of pathology include radiating pain to the eyeball, temple or ear, and with mandibular pathology, pain radiates to the neck or even to the shoulder.
Odontogenic
In dentistry, ordinary odontogenic osteomyelitis is considered the most common form of the disease. This disease occurs as a complication of dental pathologies.
The photo shows signs of acute odontogenic osteomyelitis
Symptoms of pathology are considered:
- a sharp increase in temperature;
- swelling of the face, especially at the edge of the orbit;
- enlarged lymph nodes;
- the appearance of pus in the nasal passages;
- the occurrence of fistula tracts;
- facial pain on palpation.
Traumatic
The photo shows traumatic osteomyelitis of the lower jaw
The main symptoms of traumatic osteomyelitis are:
- severe chills;
- release of exudate from the site of injury;
- pain in the wound area;
- intoxication of the body.
The most common symptoms of osteomyelitis of the lower jaw are swelling and the appearance of a pseudarthrosis. A false joint occurs due to a disruption in the regenerative process of bone tissue after a fracture. The fragments are connected by loose tissue, and not by callus, which is why they are not tightly fixed to each other.
In the early stages of the pathology, the clinical picture can be erased due to injury; it begins to actively manifest itself only 3–5 days after infection.
Hematogenous
The development of hematogenous osteomyelitis is associated with the entry of pathogenic microflora into the jaw from another inflamed area.
- lethargy;
- swelling of the mucous membrane;
- heat;
- pale skin;
- the appearance of fistulas;
- general intoxication of the body.
The disease is often accompanied by inflammation of the bones of the entire skull and damage to some internal organs.
Acute form of the disease
Acute osteomyelitis of the jaw occurs suddenly and is characterized by general and local symptoms. Signs of the disease include:
- temperature increase to 40 °C;
- pale skin;
- severe pain in the location of the pathogenic tooth, over time they lose their clear localization and spread to the entire jaw;
- loosening of a painful tooth;
- sudden weakness;
- arthritis of the jaw joint;
- pain when swallowing;
- bad breath;
- swelling and hyperemia of soft tissues;
- increased sweating;
- pronounced facial asymmetry;
- enlarged lymph nodes.
If these symptoms are present, differential diagnosis is indicated:
- with a specific form of tuberculosis, syphilis or actinomycosis;
- with purulent periostitis;
- with oncological diseases of the jaw.
Chronic form
Chronic osteomyelitis occurs against the background of an acute form of the disease and strong immunity. Sometimes the disease becomes chronic due to improper treatment. Symptoms of the pathology:
Photo of recurrent odontogenic osteomyelitis of the mandible
persistent low-grade fever;
Other jaw diseases in humans
Osteomyelitis of the jaw can be confused with other diseases, the most common:
| Name of the disease | Definition | Short description |
| Osteitis | Inflammation of the bone tissue outside the periodontium of the tooth. | As an independent disease, osteitis does not exist for long; it quickly develops into periostitis. |
| Periostitis | Inflammation of the periosteum. | It can be acute and chronic, purulent and serous. The purulent form of the disease develops as a complication of purulent periodontitis, the serous form - due to injuries. Purulent periostitis is accompanied by melting of soft tissues and periosteum, which leads to the formation of fistulas. |
| Sepsis | Infectious inflammation of bone tissue. | It occurs due to the presence of a focus of infection in the body and often leads to the death of the patient. |
| Cyst | A cavity in the root of a tooth or in the bone itself, with or without an epithelial lining. | They have odontogenic (due to dental diseases) and non-odontogenic genesis. |
| Fibrous dysplasia | Formation of a benign tumor. | The process is accompanied by significant deformation of the face shape. The causes of the disease are unknown; doctors do not rule out the influence of heredity. |
| Osteosarcoma, chondrosarcoma, lymphoma | Malignant tumors. | They develop in any bone tissue and even in the jaw. |
At the slightest suspicion of osteomyelitis of the bone tissue of the upper or lower jaw, you should contact your dentist without waiting for symptoms to intensify and complications to arise. It is better to remove the problematic tooth rather than wait for swelling or swelling to form. In addition, signs of illness may indicate a more serious illness, which only a doctor can identify.
Diagnostics
Before starting treatment, laboratory tests are required; on their basis, the presence of inflammation in the body can be determined:
- increased ESR;
- leukocytosis;
- leukopenia (in generalized form);
- high content of band neutrophils;
- hemolytic anemia;
- hypoalbuminemia;
- hyperglobulinemia;
- presence of C-reactive protein;
- increase in liver transaminases;
- decreased levels of potassium, chlorine and sodium;
- increased levels of phosphorus and calcium.
- red blood cells;
- red blood cell casts;
- traces of protein.
- taking a biopsy from a purulent focus of inflammation;
- pathogen identification.
Treatment of osteomyelitis with inflammation of the jaw bone
Treatment depends on the etiology and symptoms of the disease. It should include the following types of therapy:
- antibacterial;
- immunomodulatory;
- desensitizing.
If it is not possible to cure the disease with tablets, surgery is indicated.
You can take painkillers only after consulting a doctor; uncontrolled use of such drugs can lead to serious complications. These medications are aimed at relieving pain rather than eliminating the source of infection.
Antibiotics for osteomyelitis
Antibiotics are prescribed for osteomyelitis of the jaw before surgery and sanitation of the source of infection, which helps speed up the process of suppressing pathogens and preventing their active reproduction.
Classification
The following antibacterial drugs are most often used to treat osteomyelitis:
- penicillins: Amoxicillin, Benzylpenicillin, Nafcillin;
- cephalosorins are especially effective against staphylococcal osteomyelitis: Ceftriaxone, Cefuroxime;
- fluoroquinols: Levofloxacin, Ciprofloxacin;
- aminoglycosides: Amikacin, Torbamycin;
- glycopeptides: Vancomycin, Teicoplanin.
To prevent the development of a mycotic (fungal) infection, in addition to antibiotics, you should take Fluconazole, Nystatin or Ketoconazole.
Probiotics after antibiotics
After a course of antibiotics, probiotics are indicated:
- monocomponent: Lactobacterin, Bifidumbacterin, Bactisporin;
- multicomponent: Bifilong, Acylact, Acinol, Linex;
- combined: Bifiliz, Bifidumbacterin forte.
Surgical treatment in a dental clinic
Surgical treatment of osteomyelitis consists of various steps that are performed depending on the clinical picture of the disease and the results of a comprehensive examination. These include:
- Radical surgical treatment: sequestrectomy, sequestrectomy, trepanation of a long bone, resection of the jaw bone.
- Carrying out osteosynthesis.
- Replacement of cavities with vascularized tissues.
- Treatment of soft tissue defects.
- Surgical treatment of the source of infection.
- Removal of a tooth.
Surgeries for osteomyelitis are performed in all major cities of Russia (not only in Moscow or St. Petersburg). Before agreeing to surgery, it is advisable to request a license from the clinic to perform such manipulations.
Local therapy
Immediately after surgery, it is necessary to treat the surface of the wound with antiseptics - Levosin, Hinifuril, Iodopyron or Miramistin. In addition, foaming aerosols Dioxyzol and Aminitrozol should be used, as well as wound coverings (sterile sheets) Algimaf, Gentacyclol and Algipor. This treatment will help prevent postoperative purulent inflammation of the jaw.
Physiotherapy
The most effective methods of physiotherapy for jaw diseases include:
- electrophoresis with antibiotic solutions;
- ultra-high frequency therapy;
- UV irradiation.
Traditional medicine
Traditional medicine is an optional part of the complex treatment of osteomyelitis. This disease cannot be treated at home with herbal lotions, but the following remedies can be used to relieve some of the inflammatory symptoms (subject to appropriate antibiotic therapy and a doctor's permission):
- mumiyo;
- propolis and bee products;
- solution of soda and salt;
- herbal decoctions.
These drugs have a weak therapeutic effect, but they can be used in the complex therapy of osteomyelitis, since they have virtually no side effects.
Rehabilitation after extraction
Depending on the type and complexity of the operation, complete restoration of the gums will take from three to twelve weeks. The patient may be prescribed:
- Taking antibiotics.
- Physiotherapeutic procedures.
- Therapeutic rinses and irrigation of the oral cavity with antiseptic solutions.
- Herbal applications.
A dentist can perform the operation quickly and painlessly, but it is impossible to completely eliminate all risks and negative consequences after wisdom tooth removal. Normally, an increase in body temperature to 38.5 °C, malaise and poor health, the formation of swelling and bruising in the cheek area, and slight bleeding, which should stop within 3-4 hours, are acceptable.
What can a patient expect after wisdom tooth removal?
The first time after surgery, you need to properly care for the wound and gums, clean the oral cavity in a gentle manner and adhere to the following recommendations:
- Postoperative pain intensifies in the evening and at night, so you should have painkillers ready to take if the pain becomes unbearable. The throbbing pain can be relieved by applying cold ice to the cheek. The analgesic effect and reduction of swelling are achieved through vasoconstriction.
- Sleep on a thick, high pillow or several pillows, which will help avoid swelling.
- Eliminate hard, cold and hot foods from your diet.
- On the first day, you should refrain from drinking drinks through a straw. When used, a vacuum is created in the mouth, which leads to a slowdown in regenerative processes.
- To avoid bleeding, you should not smoke for the first week after surgery, as tobacco smoke increases the fragility of blood vessels. It is especially important to avoid smoking after removing the 8th tooth from below, since the consequences in the form of bleeding are more typical for the lower jaw.
To learn how the surgical removal of a wisdom tooth is performed, watch the video:
Complications
If primary or chronic osteomyelitis of the upper and lower jaw is not treated, the disease can lead to serious complications:
- infection of the soft tissues of the face, neck and even back;
- sepsis and generalization of infection;
- inflammation of the orbital region, which can lead to vision loss;
- meningitis.
If you choose the wrong treatment method, osteomyelitis can develop into osteonecrosis - the death of bone cells, so you should not delay contacting a doctor.
Clinical picture of osteomyelitis of the tooth socket
The clinical picture of osteomyelitis of the tooth socket is characterized by complaints of acute throbbing pain both in the area of the socket and in the area of neighboring teeth. General symptoms such as weakness, hyperthermia, headache, chills, impaired performance and sleep are also observed. Swelling of the perimandibular soft tissues develops, the submandibular lymph nodes are enlarged, dense, painful on palpation.
With osteomyelitis of the socket of only one molar of the lower jaw, the inflammatory process can spread to the area of the masseter or medial pterygoid muscle, which, in turn, can cause difficulty opening the mouth. When examining the oral cavity, the doctor may detect a dirty gray coating on the bottom and walls of the socket. You can also smell a specific smell. Percussion of adjacent teeth is painful.
The mucous membrane in the area of the transitional fold is hyperemic and swollen. Palpation of the alveolar process from the buccal and oral sides is sharply painful both in the area of the socket and adjacent teeth.
The acute phase of inflammation lasts about 6–8 days, sometimes 10 days. Then the inflammatory phenomena decrease, the process becomes chronic. The general condition improves, body temperature decreases. Swelling and hyperemia of the mucous membranes also decrease, and then pain on palpation of the alveolar process, swelling of facial tissues and submandibular lymphadenitis disappear. After 12–15 days, the tooth socket is filled with loose, pathological granulation tissue, sometimes bulges out of the socket, and pus can be released when pressure is applied.
On the x-ray we see fuzzy blurred contours of the compact lamina of the alveoli; osteoporosis and bone destruction in the alveolar region are pronounced. In rare cases, after 20–25 days from the beginning of the acute period, it is possible to identify small sequesters.
Causes of limited osteomyelitis of the socket
1. as a complication of alveolitis. 2. as a result of decreased immunity
Treatment of socket osteomyelitis
In the acute stage of the disease, therapy begins with revision of the hole. Under conduction or infiltration anesthesia, the tooth socket is cleaned of remnants of a blood clot, food and pathological tissue. Then the well is washed from a syringe with a weak antiseptic solution or a biologically active drug. The following drugs are used: staphylococcal and streptococcal bacteriophage, proteolytic enzymes, lysozyme. After this, a bandage with Alvogyl is applied to the wound.
To reduce inflammation and pain, dissection of the infiltrated area of the mucous membrane and periosteum is performed. An incision is made along the transitional fold 1.5–2 cm long, as well as an incision on the inside of the alveolar process. Drug therapy is prescribed: antibiotics, sulfa and antihistamines, analgesics, physical therapy (UHF, ultrasound, helium-neon laser). To increase specific immunological reactivity, phagocytosis stimulants are prescribed: pentoxyl, methyluracil, milife, lemongrass.
After relief of acute inflammation, treatment with multivitamins and stimulants of nonspecific resistance of the body is continued (methyluracil 0.5 g or pentoxyl 0.2 g 3-4 times a day, sodium nucleinate 0.2 g 3 times a day, milife 0.2 G). Concomitant ultrasound or laser therapy of the inflammation focus is necessary. Approximately 20 days from the onset of the acute inflammatory process, if the wound has not healed and sequesters are found on the radiograph, pathological granulations and small sequesters are removed with a surgical spoon, the walls and bottom of the hole are scraped out. The wound is washed with an antiseptic solution, dried and loosely packed with gauze soaked in iodoform liquid.
The main culprit is inflammation
Intense pain and a long temperature reaction may indicate inflammation that has invaded tissues injured by the removal of wisdom teeth. This is the most dangerous complication that can be expected from surgery. After all, even a small inflammatory lesion without proper treatment risks growing and causing serious illness.
You can rinse your mouth only one day after surgery.
The cause of inflammation may be the accidental loss of a thrombus (blood clot) from the wound. This usually happens when the patient neglects medical recommendations. For example, he tries to pick out a tooth socket with a toothpick or rinses his mouth on the day of wisdom teeth removal.
A blood clot may not form at all if the dentist used a strong anesthetic to treat the wound and dried out the tissue.
In any case, an unprotected hole is open to the influence of pathogenic bacteria and microbes that inhabit the oral cavity or get there from the outside on dirty hands or products. Microorganisms tend to multiply quickly on a chosen surface and cause infection.
Trigeminal neuritis
Today, traumatic neuritis of the trigeminal nerve is considered one of the most common causes of pain syndromes in the maxillofacial area.
As a complication, it occurs during the removal of permanent molars of the lower jaw, due to damage to the lower alveolar nerve in the mandibular canal. The apices of the roots of the lower molars are in close proximity to the mandibular canal and in some cases may be located in the canal itself. Sometimes, due to chronic apical periodontitis, the bone between the root apex and the wall of the mandibular canal is resorbed. When a tooth is loosened by an elevator, the lower alveolar nerve can be injured, which will lead to partial or complete disruption of the functions of the third branch of the trigeminal nerve. The result is pain in the jaw, numbness of the lower lip and chin, decreased or absent sensitivity of the gums, decreased electrical excitability of the dental pulp on the affected side. Usually all these phenomena gradually disappear after a few weeks.
Electroodontometry
Electroodontometry is the most effective method for assessing the functional state of the trigeminal nerve when it is damaged. EDI is based on a study of the reaction of the teeth of the lower jaw to electrical stimulation. The method is performed on all teeth of the lower jaw, with preserved pulp both in the affected area and on the opposite healthy side.
S.N. scale Fedotova (1997) to assess the severity of damage to the inferior alveolar nerve based on electrical odontometry data:
- mild degree - reaction of teeth with preserved pulp on the side of nerve damage within 20-40 μA;
- moderate severity – reaction of teeth to currents from 40 to 100 µA;
- severe degree - complete loss of pain sensitivity, reaction of teeth to currents above 100 μA
The use of EDI to diagnose traumatic injuries of the inferior alveolar nerve is impossible if:
- lower jaw teeth endodontically treated
- lower jaw teeth are covered with orthopedic structures
- metal elements of splinting structures are fixed on the teeth
- missing teeth
Locations for measuring electrical excitability of facial skin
Assessment of the area of paresthesia in traumatic neuritis of the inferior alveolar nerve
The zone of paresthesia is identified - impaired sensitivity of the skin based on a tactile test, photographed, followed by an assessment of the area of the paresthesia zone: points are drawn on the border of areas of normal sensitivity of the skin, the red border of the lips and the paresthesia zone, which are then connected by a continuous line. Zones of hyper-, hypo- and anesthesia were marked with different colors.
I - vertical lines:
- midline,
- a line passing through the outer edge of the philtrum,
- a line passing through the outer edge of the wing of the nose,
- pupil line;
II - horizontal lines:
- lip line,
- a line running along the lower edge of the red border of the lips,
- the border line between the chin and lower lip,
- a line drawn along the most protruding part of the chin,
- line of the border of the chin and submental areas.
Schematic representation of the areas for measuring facial skin paresthesia.
Each of the 12 resulting squares was assigned a score depending on the nature of the sensitivity disorder:
0-sensitivity is not impaired;
1-skin hyperesthesia
2-hypoesthesia of the skin;
3-anesthesia of the skin.
Next, the sum of points was calculated and divided by 12 (quadrants).
3.0-2.1 – severe sensitivity impairment was diagnosed;
2.0–1.1 – moderate severity;
less than 1.0 – mild severity of the pathology being studied
Treatment of neuritis
Treatment of neuritis in traumatic injuries must be timely and wait-and-see tactics are unacceptable. For mild damage to the inferior alveolar nerve, decongestant therapy (prednisolone, veroshpirone) is sufficient. In case of moderate severity of damage, drugs that improve the conductivity of the nerve trunk (neuromedin) are added to decongestant therapy. In case of severe damage to the nerve trunk, in the absence of positive dynamics in the restoration of sensitivity within 4 months, the patient should be referred for a consultation with a neurosurgeon in order to resolve the issue of the possibility of restoring the anatomical integrity of the nerve trunk.
Various reflexotherapy methods are widely used in the complex treatment of diseases of the peripheral nervous system. In the complex treatment of diseases of the peripheral nervous system, reflexology methods such as electroacupuncture and transcutaneous electrical neurostimulation are widely used.
Prevention of neuritis
Prevention of neuritis of the inferior alveolar nerve is the correct technique for removing teeth, correct diagnosis and correct reading of the radiograph, and a gentle technique for dislocating the roots of teeth in the lower jaw with an elevator.
Paresthesia
Paresthesia is a loss of sensation in the lips, cheeks, tongue and chin. It is the result of damage to the facial nerve. This complication after tooth extraction is quite rare, and most often goes away within a couple of weeks. Taking vitamins B and C and injections of galantamine and dibazole help speed up recovery.
During the operation, nerve endings may be affected, and not always through the fault of the doctor - an option with a complex location, structure and the very removal of the diseased tooth is possible.
This can provoke neurological complications, one of which is paresthesia - numbness of the tongue. In addition, a feeling of numbness, “pins and needles” sometimes appears in the area of the lips, cheeks and chin.
The doctor may prescribe injections of drugs such as Galantamine and Dibazol, as well as taking vitamins C and B.
Abscess after tooth extraction
An abscess after tooth extraction is a long-term complication of a tooth extraction operation that occurs as a result of contamination of the wound surface with microorganisms. When teeth are removed, not only the tissues surrounding the tooth can be injured, but also the mucous membranes of the mouth and cheeks. A fresh wound is a favorable environment and entry point for microorganisms. Therefore, under appropriate circumstances, an abscess may form in the soft tissues or in the hole, which over time and without treatment can “spill” with the formation of phlegmon in several areas.
Causes of abscess
The cause of an abscess may be failure to comply with the rules of asepsis and antisepsis directly during the tooth extraction operation. As a result of incorrect actions by the doctor, infection occurs in the tooth socket and subsequent suppuration. Also, infection of the socket and soft tissues can occur due to the fault of the patient himself if he does not follow all the dentist’s recommendations. The patient must strictly follow the prescribed procedures, otherwise repeated surgery cannot be avoided.
Prevention and treatment of tooth abscess
Prevention of the appearance of an abscess after tooth extraction is basic regular oral hygiene and following all the recommendations of the dentist. Also, preventive measures include visiting the dentist if you experience pain within a few days after tooth extraction. Treatment of an abscess consists of opening and cleaning the abscess cavity, removing purulent formations and prescribing anti-inflammatory therapy. Sometimes the abscess opens on its own, and the pain disappears. But this does not mean that the process has been stopped, so further treatment by a dentist is necessary. Otherwise, the infection may spread to contact areas and intensify the process.
Root remains inside the gum
Incomplete tooth extraction is the most common problem with such dental surgery.
In severe cases, the operation has the status of “complex”. This formulation means that a root or a fragment of it remains inside the gum after tooth extraction.
Symptoms of this type of complication:
- pain in the area of the operation;
- edema;
- development of inflammation.
The first is more rare: when the doctor was not sufficiently prepared for the operation and simply did not notice the fragment that formed during the process.
The second reason is the surgeon’s conscious decision to leave the fragment. It is dictated by the location of the foreign body, which, when removed, can lead to infection or damage to the nerve.
To remove the fragment it is necessary to perform a second operation. Before the procedure, the patient must undergo an X-ray examination, and the doctor carefully studies the images and plans his actions.
There is another option, which takes longer, and is used when repeat surgery is problematic.
With complete healing using sea buckthorn oil lotions, the fragment will be “pushed out” by the soft tissues on its own.