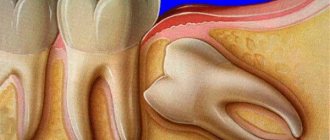
Temporary and permanent teeth have their own timing of eruption and specific locations on the alveolar process. Sometimes teeth erupt prematurely or remain in the bone, appearing much later (in this case, it bears the common name - wisdom tooth). Delayed teething is called “retention.” Sometimes teeth, including wisdom teeth, occupy an incorrect position, shift in the vestibular, palatal, lingual direction, and are rotated around their axis. This anomaly is called “dystopia”. Most often, the upper canines and lower wisdom teeth are affected by delay.
The presence of an impacted tooth (that is, the eruption of a wisdom tooth is delayed indefinitely) in the jaw in some cases does not cause any pathological phenomena in the patient. In this case, wisdom tooth removal is not urgent. But if an impacted tooth causes the formation of cysts, neuralgic pain, or an inflammatory process, then an atypical tooth extraction operation is used.
How are wisdom teeth different from other teeth?
- Wisdom teeth erupt between the ages of 18 and 25, and often later.
- Wisdom teeth do not have a distal neighbor that would prevent the tooth from moving distally.
- The wisdom tooth does not have a milk predecessor that would prepare the conditions for its eruption.
- Erupting at the age of 18-25 years, when the formation of the jaw bone tissue is completely completed, the tooth has to overcome a significant mechanical obstacle.
- The pterygomaxillary and external oblique lines thicken the cortical plates in the projection of the angle of the lower jaw and, thereby, create additional difficulties for the eruption of wisdom teeth
The difficult eruption of wisdom teeth is explained by the anatomical features of the structure of the lower jaw and the late timing of eruption. The lack of space in the dentition for the third molar - this is what the wisdom tooth is called in dental terminology - is associated with changes in the masticatory apparatus in the process of human evolution. The softer the food became, the less chewing stress was required on the teeth, which over time led to a decrease in the size of the jaws. Studies have shown that in modern humans, the width of the dental arch has decreased by 10-12 mm compared to distant ancestors.
If there is difficulty in the eruption of a wisdom tooth, it is necessary to consult a dentist and decide on its future fate. A general medical and dental history helps the dentist collect all medical information about the patient’s health, since the more the dentist knows not only about how the wisdom tooth is cut, but also about the patient’s health in general, the better he will be able to imagine the methods and methods of the upcoming treatment. The dentist must find out whether the patient suffers from any other disease and what medications he is taking.
After the dentist has collected an anamnesis and examined the patient, he begins an X-ray examination, with the help of which he assesses the condition of the wisdom tooth and gums, its roots, the bone located around the root and the degree of immersion of the wisdom tooth. After a thorough examination of the patient, the dentist decides whether wisdom tooth removal is necessary or not.
The operation of an impacted wisdom tooth begins with determining access to the tooth. Then a triangular-shaped mucoperiosteal flap is cut out, the bone tissue located above the tooth is removed, and the wisdom tooth is removed in parts or entirely. Then the flap is fixed with sutures, and the hole is tamponed with iodoform turunda.
The operation is performed under local anesthesia. In some cases, to improve psychological well-being, the doctor advises the patient to take medications to reduce anxiety during and after wisdom tooth removal.
Removal of third molars
Author: Reznick JB
There is no generally accepted method for removing impacted 3rd molars. Schools in the UK advocate the lingual approach, while US schools tend to favor the buccal approach. Bone preparation and tooth sectioning can be performed with a ball, fissure, or Lindemann bur (Fig. 1).
Figure 1 (a) Spherical bur. (b) Fissure bur. (c) Lindemann bone bur.
Third molars are usually sectioned with a surgical bur, but some clinicians still prefer a hammer and chisel. Working with soft tissues is extremely diverse. There are many types of flaps that use different incisions. Wound closure can be primary with suturing or secondary without suturing.
This article discusses the various surgical techniques used to remove impacted 3rd molars. Recommendations are based on a literature review and the author's 36 years of experience.
Third molars on the mandible
Removal of impacted third molars in the mandible can be divided into seven stages.
- flap
- Gutter Formation
- Sawing a tooth
- Dividing a tooth into fragments
- Removing fragments
- Surgical treatment of the wound
- Closing
flap
All third molar flaps are designed to separate the periosteum from the underlying bone and provide access to the intervention site. Various types of flaps and incisions are used (Figure 2).
Figure 2. Patch designs: (a) Envelope.
Figure 2 (b) S-shape.
Figure 2 (c) Triangular.
Figure 2 (d) Modified triangular.
Regardless of design, all flaps should be full-thickness with a wide base.
Much research has been conducted to determine the best flap design for mandibular third molar extraction. Most of these studies found no difference in postoperative healing between different types of flaps.
Sulieman evaluated four types of flaps for postoperative pain, swelling, and trismus. The 60 patients were divided into 4 groups based on flap type: envelope, triangular, modified triangular, and S-flap (See Figure 2). Pain and swelling were assessed subjectively, and trismus was assessed by measuring maximum mouth opening (in mm) between teeth 11 and 41. In the postoperative period, no significant differences were found between the 4 groups.
The second study compared the two most commonly used flaps, envelope and triangular, to evaluate periodontal healing and postoperative complications. Twenty-four wisdom teeth were removed from 12 patients with an average age of 16 years. Patients were included in the study when radiographs showed that only a crown had formed (germectomy). Each patient underwent two extractions using a triangular flap on one side and an envelope flap on the other. Periodontal probing was performed before surgery
Pericoronitis
One of the common problems arising from incorrect tooth position is pericoronitis.
Pericoronitis is an inflammatory process of the tissues surrounding the wisdom tooth. The cause of pericoronitis is difficulty in the passage of the tooth through the gum. Even a small protrusion of a tooth above the gum can form a hole in it, which gradually expands, forming foci of infection. Plaque accumulates in this space between the gum and tooth and is difficult to clean.
Symptoms of pericoronitis include sensitivity and swelling of the gums surrounding the wisdom tooth. Sometimes there is severe pain, bad breath or a bad taste in the mouth.
If the dentist discovers that the cause of the development of pericoronaritis is an immersed wisdom tooth, then he suggests removing the wisdom tooth. The patient is prescribed a seven-day course of treatment. Antibiotics help reduce the infection, allowing the removal process and subsequent healing to go more smoothly. After a course of antibiotic treatment, the wisdom tooth is removed.
Care and rehabilitation
After the operation, you must follow the doctor’s recommendations and take the following precautions:
- do not eat for 2 hours after the intervention;
- the first few days, eat warm, soft foods;
- chew on the opposite side;
- minimize physical activity;
- Until the wound heals, give up alcohol, smoking, and do not visit baths or saunas;
Hygiene must be carried out very carefully so as not to provoke the suture to diverge and wash out the blood clot from the socket. According to indications, the surgeon will prescribe antiseptic rinses and medications. If you follow medical recommendations, the alveolar socket will heal quickly, without complications. Rehabilitation takes 1-5 days.
Periodontal diseases (gum diseases)
Misaligned wisdom teeth can lead to the development of periodontal disease. If the wisdom tooth is misaligned, the patient is unable to clean out plaque with a toothbrush and floss, which allows bacteria to develop and leads to periodontal disease. If such a disease is neglected, it can cause great harm to the gums and surrounding bone tissue. Periodontal disease does not develop in isolation around a single tooth, so to prevent it, the dentist recommends removing wisdom teeth that are incorrectly positioned.
How to remove a wisdom tooth
After the patient is positioned in the dental chair or on the operating table, anesthesia is administered . For adequate pain relief during surgery, articaine anesthetics are usually used, with the exception of cases of individual intolerance and allergic reactions to the administered drug. In particularly difficult cases, wisdom teeth are removed under general anesthesia.
Further, the sequence of the surgeon’s manipulations depends on what was the reason for the decision to rip out the third molar.
If an operation is performed for G8 retention, the doctor’s action plan is as follows::
- Performing dissection of the soft tissue of the gums using a scalpel and detachment of the periosteum with a raspatory.
- Expanding the surgical field by removing part of the alveolar bone using a drill. If the roots are widely spaced, it may be necessary to saw them along the bifurcation to facilitate removal.
- Extracting the wisdom tooth and checking the socket for the presence of granulations, fragments or root fragments. The extracted tooth is carefully examined and its integrity is determined.
- Medical treatment of the wound with the use of antiseptics, especially with purulent-necrotic masses.
- Bringing the edges of the wound closer together, placing the mucous flap in place and applying sutures.
You can ask your doctor before starting the procedure how much it hurts, and whether it’s even worth pulling out a wisdom tooth. A competent specialist will always treat you with understanding and answer any questions regarding the progress of the operation.
Such procedures are performed only in operating rooms or specially adapted surgical rooms with strict adherence to the rules of asepsis and antisepsis.
The patient is invited for a second visit after 2-3 days; during the appointment, it is determined whether there are any signs of inflammation of the socket.
Postoperative complications for wisdom teeth
Dry sockets are one of the most common complications encountered during wisdom teeth removal. After a tooth is removed, a blood clot forms in the empty socket. Formation of a blood clot is an important part of the socket healing process. If for some reason a blood clot does not form, it results in a dry socket.
Dry sockets usually form after difficult extractions associated with significant trauma. Dry sockets appear as dry or sharp pain after wisdom tooth removal, 3-4 days later. There is a feeling that the pain on the wisdom tooth spreads from the extraction site towards the ear. Dry socket often causes an unpleasant taste or smell in the mouth.
To treat a dry socket, the dentist places a cotton swab with a medicine on the extraction site that reduces and soothes the pain. You should change your tampon every 24 hours until all symptoms disappear. This procedure may take several days.
Paresthesia is the most rare complication during the wisdom tooth extraction procedure. Paresthesia is a long-lasting numbness of the lip, tongue and chin. This happens because wisdom teeth may be located very close to the jaw nerves. And during the removal process, sometimes these nerves are touched or damaged. Usually the paresthesia lasts for several days, weeks or months: however, unfortunately, if the nerve is severely damaged, the paresthesia can become permanent.
Structure of a wisdom tooth
According to basic anatomical principles, the structure of third molars is similar to other large molars. “Eights” also have root and coronal parts, and inside there is a pulp chamber filled with the dental nerve.
The main difficulties when removing the last teeth in a row are that their roots often have an atypical structure. As a rule, “eights” on the upper jaw have two roots, and on the lower jaw – three. However, doctors often encounter teeth with two or four roots that are widely spaced relative to each other. It is also not uncommon for wisdom teeth to have one massive root formed during fusion.
The main distinguishing characteristics of third molars:
- strongly curved and spaced roots,
- atypical structure of the tooth cavity, which complicates endodontic treatment and sometimes makes it impossible.
Age indications for wisdom tooth removal
There are no rules determining the optimal age for wisdom tooth removal. However, practice shows that the sooner you get rid of these teeth, the fewer complications you can expect from them. If there are very serious reasons for removing a wisdom tooth, it needs to be removed quickly. It is preferable to remove wisdom teeth when the roots of these teeth have not yet formed, and the bone surrounding the wisdom tooth is not yet very dense - this is late adolescence or early adolescence.
Carrying out complex surgery to remove
Patients are especially frightened by the need for surgical intervention when removing third molars. How long the operation lasts, whether it is painful to remove a wisdom tooth, what complications and consequences there may be - all this worries a person who is scheduled for extirpation of “eights” in a hospital setting.
Complex wisdom tooth removal is a method in which various devices, such as a chisel, drill, and scalpel, are used to remove the causative tooth. During the operation, incisions are made, part of the alveolus is removed, which prevents the removal of the figure eight, and sutures are placed on the wound.
Typically, the operation is performed on impacted (unerupted), semi-impacted (semi-erupted) and dystopic (located outside the dentition) wisdom teeth. The anatomical features of their location make it difficult to insert instruments and smoothly remove the tooth. The fact is that if the “eight” is located in the bone, then it will not be possible to pull it out with forceps. A drill is used to drill out a small piece of alveolar bone.
The preparatory stages and diagnostics are carried out in the same way as during normal removal. Is it painful to have wisdom teeth pulled out in such a complicated way? The introduction of a stronger and longer-acting anesthetic will remove all signs of discomfort.