A cyst on the tonsil is a benign neoplasm located on the surface or in the thickness of the lymphoid tissue. Most often, the appearance of an accumulation of pus and lymph, covered with an isolated capsule, accompanies chronic inflammation of the tonsils (tonsillitis). However, in rare cases, you may encounter congenital cysts. Congenital cystic cavities almost always require surgical intervention; acquired ones can be completely cured conservatively or using gentle laser techniques. You should not hesitate to visit a doctor, since the growth of a cyst, especially in a child, can threaten respiratory function.
Classification
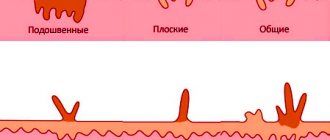
Determining the type of cyst plays an important role in choosing therapeutic tactics. Based on the mechanism of formation, appearance and content, cysts are distinguished:
- Dermoid cavities are congenital cavities that arise against the background of intrauterine development disorders. Externally they look like nodes covered with a dense capsule. The contents of such formations are viscous and may contain inclusions of tissues atypical for the location of the cavity - hair, bones, teeth.
- Retention cavities are acquired cavities caused by stagnant processes in the tissues of the tonsils. Their thin shell can be easily damaged by inspection or by eating hard food. The cavities are filled with a mixture of secretion of lymphoid tissue, pus and/or blood.
Since the area of the mouth and nasopharynx contains 6 tonsils - 2 paired and 2 unpaired, cysts may differ in location. According to ICD-10, cysts on the tonsils have the following codes :
- cysts of the palatine tonsils (paired, also called tonsils) – code – D4;
- lingual unpaired (D1);
- pharyngeal (nasopharyngeal) tonsil (with pathological enlargement, this accumulation of lymphoid tissue is called adenoids) (D6).
Among all diagnosed tonsil cysts, the majority are retentional.
Diagnostic Basics
As mentioned above, the described type of retention cyst of the lower lip in a child and an adult is localized on the outer side of the mucous membrane of the oral cavity or lips, so it is extremely simple and easy to notice their appearance in time. The difficulty in diagnosing such a benign disease may lie in the fact that tumors in the oral cavity or on the lips, for some reason, can form in the deep layers of the epithelium and develop there over a long period of time. Due to this location of the tumor, it is extremely difficult to find and begin treatment in a timely manner.
The retention cyst of the lower lip, according to reviews and official statistics, grows very quickly. Within a couple of days after its appearance, it can reach 5 millimeters in diameter. Diagnosing such a tumor is extremely easy. Another factor that helps in the process of determining the disease of a retention cyst of the lip ICD 10 is that it often greatly interferes with chewing food or talking, since it is located directly in the oral cavity between the lip and teeth.
It is important to say that due to the specific attachment site, the retention cyst of the lower lip ICD 10 can often be damaged. For example, when chewing food or brushing teeth mechanically. In this case, the capsule of the cyst ruptures, and a large amount of white serous or purulent fluid can be released from its body. In some cases, if this type of cyst contains bacteria, blood may accumulate in its capsule. After such a tumor ruptures, the inflammation may disappear for a while. However, after a few days, the retention cyst of the upper lip appears again.
Causes
The main prerequisites for the development of retention cysts are chronic infectious inflammations in the oral cavity and pharynx:
- palatine tonsils (tonsillitis);
- mucous membrane of the paranasal sinuses (sinusitis);
- mucous membranes of the larynx (laryngitis).
These conditions create favorable conditions for the growth of cysts, generally in the following sequence:
- Swelling of the mucous membranes.
- Impaired outflow of food particles and microscopic tissue debris, as well as glandular secretions.
- Stretching of the walls of the lymphoid tissue of the tonsils, filling them with stagnant or purulent contents.
In addition, acquired cysts can provoke the growth:
- Hormonal changes - affect the composition and consistency of glandular secretions, thickening it and thereby causing stagnation.
- Weakening of the immune system (including physiological - during pregnancy and childhood) allows chronic diseases of the oropharynx to occur over a long period of time.
- Allergic reactions that cause swelling of the mucous membranes.
- Excessive alcohol consumption.
- Smoking.
- Professional activities involving inhalation of aggressive vapors.
- Injury to the tonsils - including when eating too hot, hard or spicy foods.
- Gastroesophageal reflux disease (GERD) is accompanied by constant belching and tonsillitis.
- Autoimmune diseases - tonsils play the role of the first line of immune defense when inhaling foreign pathogens or microorganisms. However, they may also suffer from incorrect functioning of the immune system itself, which attacks not pathogenic structures, but healthy cells, causing general or local inflammation.
The cause of the development of dermoid cysts is anomalies in the intrauterine development of the fetus; however, dermoids can be diagnosed both in childhood and in adulthood.
Cyst of the sublingual gland code icd 10
ICD-10 category: K11.6
ICD-10 / K00-K93 CLASS XI Diseases of the digestive organs / K00-K14 Diseases of the mouth, salivary glands and jaws / K11 Disease of the salivary glands
Definition and general information[edit]
Salivary gland mucocele
A mucocele (mucous cyst) is a cyst (usually about 1 cm in diameter) containing mucus that results from traumatic injury to the ducts of the minor salivary glands. Large mucoceles in the floor of the mouth are called ranulae.
Ranula
Ranula is a cystic tumor located in the sublingual region, deep in the muscles of the floor of the mouth. This name was given because of the resemblance of the tumor to a swelling pharyngeal bladder in some species of frogs (from the Latin rana - frog).
Etiology and pathogenesis[edit]
The tumor comes from the sublingual salivary gland, which opens on the lower surface of the tongue. Much less commonly, ranula originates from abnormally located processes of the sublingual gland. Most authors associate the occurrence of a tumor with chronic inflammation of the gland and narrowing of the excretory duct, which leads to secretion retention and the development of a retention cyst. The gland gradually atrophies. Some authors consider ranula to be a cystic embryonal tumor.
Clinical manifestations[edit]
A ranula is a thin-walled cyst covered with the oral mucosa through which fluid can be seen, giving it a bluish tint. The cyst is usually located to the right or left of the frenulum of the tongue; bilateral lesions are much less common. The contents of the cyst are a colorless liquid that looks like the white of a chicken egg.
Mucocele of the salivary gland: Diagnosis[edit]
Palpation of the tumor is painless, fluctuation is characteristic. Ranula sizes vary. A small ranula does not cause any particular trouble to the child. As the cyst grows, it lifts the tongue, protrudes it outward, and interferes with sucking and swallowing. Large wounds can make breathing difficult.
Differential diagnosis[edit]
Differential diagnosis is carried out with hemangioma and lymphangioma of the floor of the mouth, less often with lipoma and dermoid cyst.
There is a differential diagnostic technique that allows you to distinguish lymphangioma from ranula: when pressing on the chin area with lymphangioma, the tumor-like formation in the sublingual area increases due to the movement of liquid contents. Hemangioma, unlike ranula, has a bluish-purple color, is accompanied by vasodilation and has a tendency to grow rapidly. When pressed, the hemangioma flattens. Lipoma is a denser, whitish-yellow tumor. A dermoid cyst is most often located in the midline, has clear boundaries and contains a whitish, crumbly mass.
Mucocele of the salivary gland: Treatment[edit]
Ranula can only be eliminated surgically. It is preferable to remove the cyst after making an incision in the oral mucosa. In cases where it is impossible to completely remove the cyst, its anterior wall is excised, and the cyst cavity is lubricated with an alcohol solution of iodine.
If the condition of the child (usually a newborn) does not allow radical surgery, puncture of the cyst is possible.
The timing of the operation depends on the size of the cyst. If there is difficulty swallowing or breathing, surgical intervention is performed immediately after diagnosis, including for infants. In the postoperative period, oral toilet is prescribed.
Prevention[edit]
Other[edit]
Traumatic salivary gland cyst
Patients complain of swelling in the area of the salivary gland (parotid, submandibular, sublingual), which appears in the 1st or 2nd week after the injury. In this case, healing can take a long time. During the treatment process, the patient is repeatedly punctured by the resulting “salivary tumor,” but the success of the treatment is temporary. After several months, the swelling is constantly determined. This or a similar history allows us to correctly determine the origin of the salivary gland cyst. Upon examination, palpation and additional examination, the clinical signs of the cyst are similar to those of salivary gland cysts of any origin. The swelling is soft and painless. Its boundaries are relatively clear. Scars can be found on the skin or mucous membrane of the oral cavity - traces of trauma or the result of surgery performed in the area of the gland. When the cyst is punctured, a clear, viscous liquid (saliva) is obtained. With sialography, it is possible to establish a filling defect, deformation of the ducts and their displacement by a cystic formation.
Treatment
Treatment of damage to the salivary glands depends on the nature and location of the injury. For incised wounds of the peripheral parts of the gland, layer-by-layer suturing is successful - suturing the gland, fascia, subcutaneous tissue and skin. Drainage should be left between the seams for 3-4 days. In this case, during the wound healing period, medications are used that suppress saliva secretion: 0.1% atropine solution, belladonna tincture, and radiotherapy. To bring the edges of the wound closer together, lamellar sutures are indicated. Plastic closure of the wound is possible later, during the period of its granulation. In this case, to prevent a salivary fistula, a long wound channel is formed for saliva to flow out of the wound using opposing triangular flaps or conditions are created for the outflow of saliva into the oral cavity. During the initial surgical treatment of gunshot wounds of the face, in order to avoid damage to the gland ducts (and in the parotid region, to the branches of the facial nerve), only economical tissue excision should be performed. If a wound to the parotid duct is detected, its ends must be carefully sutured, and the sutures are placed in such a way as not to disturb its lumen. A preliminary insertion of a polyethylene catheter into the duct is used, which is left for 12 days after the operation, or bougienage is performed.
Sources (links)[edit]
Surgical dentistry and maxillofacial surgery [Electronic resource]: National Guide / Ed. A.A. Kulakova, T.G. Robustova, A.I. Nerobeeva. - M.: GEOTAR-Media, 2015. - (Series “National Guidelines”). — https://www.rosmedlib.ru/book/ISBN9785970437278.html
Pathological anatomy. Atlas [Electronic resource]: textbook / Zayratiants O.V., Boykova S.P., Dorofeev D.A. and others. Ed. O.V. Zairatyantsa - M.: GEOTAR-Media, 2010. - https://www.rosmedlib.ru/book/ISBN9785970412848.html
Additional reading (recommended)[edit]
Active ingredients[edit]
Clinical picture
A small cyst - up to 5 mm - at a certain location can go unnoticed, without causing any discomfort to the patient. Further growth results in a pronounced increase in the size of the tonsil and is accompanied by :
- Sensation of a foreign body in the throat.
- Pain at the site of the cyst, including when swallowing.
- Difficulty eating – this symptom is easy to notice in a child. If the cavity suppurates, then the discomfort turns into severe pain.
- Itching, tingling or burning in the tonsils.
- The smell of rot from the mouth caused by the retention of food particles in the area of the cystic node.
- Coughing when talking or eating - children may cough frequently.
- Change in voice timbre, appearance of nasality or hoarseness.
- Breathing problems.
- Involuntary drawing of liquid food from the mouth into the nasal passages.
- A “popping” sensation in the ear.
- Frequent exacerbations of chronic ENT pathologies.
The cyst can be injured, allowing liquid contents to flow into the pharynx; if the cavity bleeds, urgent diagnosis is necessary to exclude oncological degeneration.
Clinical manifestations
At first, the patient feels the tumor as a small single growth on the mucous membrane of the lower lip. There is no pain or discomfort when pressing. The cyst on the lip gradually progresses, increasing in size to 2 cm.
After injury to the walls and leakage of cystic secretion, the patient feels an unpleasant odor and notices an admixture of pus and blood. Some time after emptying, the pathological fluid accumulates again, and the neoplasm soon returns to its previous size.
The addition of an inflammatory process can provoke pain . Constant injury to the retention cyst threatens to involve surrounding tissues and develop complications (bleeding, ulceration of the mucous membrane, abscesses). When an infection enters the bloodstream, the entire body suffers, the general condition worsens, and intoxication begins.
There are quite frequent cases of degeneration of pathologically altered cyst cells into malignant ones. The risk group consists of smoking patients, whose mucous membranes are regularly exposed to toxic cigarette tars.
Diagnostic measures
Symptoms of cysts are nonspecific - they can accompany both lacunar plugs and more serious diseases (tuberculosis, syphilis). Therefore, you should contact an otolaryngologist. After the initial examination and collection of complaints, he will prescribe the necessary diagnostic measures:
- pharyngoscopy - visual examination of the pharynx using a spatula, mirror and light source; depending on the location of the cyst, oropharyngoscopy, posterior rhinoscopy or indirect pharyngoscopy are used;
- X-ray, ultrasound or CT scan of the head - in the presence of large cysts, dermoids, and also if surgical intervention is necessary;
- examination of a tissue sample obtained during cyst puncture is necessary for large or deeply located cysts or signs of malignancy - intensive growth or bloody discharge.
If there are concomitant infections, a blood test or throat swab for culture may be required, and if degeneration is suspected, a consultation with an oncologist may be required.
Diagnostic methods
After an external examination of the tumor on the lower lip, the dentist prescribes a series of instrumental studies. They make it possible to determine the condition of the duct of the affected salivary gland and the presence of stones in it. Laboratory research makes it possible to identify the nature of the inflammatory process and the type of bacterial microflora, and to exclude the presence of a malignant neoplasm. The following types of diagnostics are carried out :
- probing the salivary gland duct;
- ultrasound examination of the salivary gland;
- sialography - contrast x-ray examination of the salivary glands;
- histological examination of the surgical material (carried out after completion of the operation).
Conservative therapy
This treatment strategy includes the use of medications and a course of therapeutic procedures. Among the groups of drugs prescribed for tonsil cysts:
- antibiotics for oral administration - in case of infection, suppuration or concomitant tonsillitis;
- antifungal agents - if bacterial culture analysis reveals the presence of pathogens of this type;
- antihistamines - in the presence of allergic swelling of the pharynx or runny nose;
- immunomodulators - to increase general immunity (Betaferon, Derinat);
- local remedies - sprays, nasal drops or ointments that have an antiseptic, anti-inflammatory or countercurrent effect.
If autoimmune disorders occur, drugs that suppress the immune system are prescribed - immunosuppressants (Prednisolone, Cyclophosphamide).
Procedures, including physiotherapy, play an important role in conservative treatment, some of which can be performed at home:
- Gargling is the simplest and most accessible technique. You can use Iodinol, Chlorophyllipt, Lugol, Furacilin.
- Wiping the tonsils with a swab moistened with an antiseptic solution - the admissibility and technique of implementation should be clarified with a doctor. With thin walls of cysts, it can cause rupture of the cavity.
- Rinsing the tonsil area with a syringe with a cannula (curved nozzle) - this procedure is not always pleasant and safe at home; sometimes it is advisable to entrust it to a specialist. Antiseptics are used - Miramistin, Rivanol or Rotokan.
- Inhalations - they can be carried out at home using a nebulizer using agents such as Amikacin or Chlorhexidine.
- Ultraviolet or infrared irradiation - for the purpose of disinfecting the surface of the pharynx.
- Phonophoresis is the cleansing of tonsil tissue using ultrasound. The procedure is painless and effective in treating children.
There is a special device - Tonsilor, which allows for deep cleaning of the tonsils. The course of treatment helps reduce relapses of chronic tonsillitis, which causes cysts. However, its use is possible only in a medical facility and has limitations (including pregnancy, hypertension, retinal detachment).
Conservative treatment
Surgery is recommended to treat a retention cyst on the lip . Only a radical method of therapy can ensure a quick and complete recovery of the patient with minimal risk of relapse.
In some cases, the salivary duct restores its functioning on its own after some time. In this case, the cyst resolves and there is no need for treatment. But, in most cases, the cyst progresses, and the patient is prescribed cystectomy.
After cystectomy, the surgeon recommends daily disinfection of the suture area with Chlorhexidine solution, applying Metrogyl Denta, Holisar, Propolis ointment and other wound-healing preparations.
Surgery
Surgery is inevitable in the following cases:
- congenital dermoid cyst was diagnosed;
- conservative treatment causes relapses;
- tumor size exceeds 1 cm;
- the cyst tends to grow deeper into the layers of lymphoid tissue;
- multiple cavities on one or two paired tonsils.
Emergency surgery can be performed in case of suppuration of the cyst, respiratory failure, or significant deterioration in the general condition.
Conventionally, three types of interventions can be distinguished:
- gentle laser surgery:
- puncture (drainage - pumping out the contents of the cavity);
- excision – the tonsil is partially or completely removed.
Among the advantages of laser manipulations performed under local anesthesia are::
- no damage to healthy tonsil tissue;
- eliminating the risk of bleeding and infection - the laser simultaneously disinfects the surface;
- minimal recovery period;
- low probability of relapse.
Laser surgery is not performed for multiple and large cysts.
Puncture can be classified as a palliative technique - it can significantly improve the condition (for example, if a tonsil cyst interferes with normal breathing). However, pumping out the contents threatens relapses - secretions and pus again accumulate in the unremoved capsule. This type of intervention is relevant if the patient is elderly or in serious condition.
Radical surgery (excision) has the following distinctive features:
- The use of general or local anesthesia depending on the volume of tissue removed. If the entire tonsil is removed (tonsillectomy), general anesthesia is required.
- Effective for complicated, large or congenital cysts, persistent relapses or malignant degeneration.
- Requires a recovery period of at least 3–4 weeks.
After radical removal of cysts on the tonsils, the following should be excluded for the duration of rehabilitation :
- heavy physical activity;
- visiting a bathhouse or swimming pool;
- any types of warming up;
- alcohol and smoking;
- hot, cold, spicy or solid foods.
To reduce pain, relieve postoperative inflammation and prevent infection, oral antibiotics and throat irrigation with antiseptics are prescribed.
After surgery, you must be observed by an otolaryngologist for 6 months.
Features of the development of a retention cyst on the lower lip
The reason for the appearance of a benign tumor of the described type in the oral cavity is a partial or complete blockage of the salivary gland, at the site of which a tumor of a lip retention cyst begins to form. Because of this, the body of the tumor is filled primarily with salivary substance mixed with pus or blood. Such tumors do not have a multi-chamber structure, do not grow large, and in very rare cases provoke the appearance of painful symptoms or inflammation.
It is worth saying that if, in addition to a cyst, an inflammatory process develops in the oral cavity, tooth suppuration occurs or the gums are damaged, the growth of the capsule may be accompanied by pain, which causes noticeable discomfort during eating or talking. Extremely inflamed and infected, these types of tumors may have multiple chambers in their body and be abnormal in size.
IT IS IMPORTANT TO KNOW!
Externally, it is extremely easy to determine the tumor capsule and remove the retention cyst of the lower lip. A retention cyst on the lip has a pink or red inflamed color. If the tumor exceeds the permissible norms for its size and begins to strongly stretch the mucous membrane in the thickness of which it is formed, a small inflamed blue or purple bubble can be seen at the site of its formation. If you press your finger on the problem area, it will most likely simply fall into the depression under the cyst and appear again after a while. To the touch, such a cystic body may resemble a large accumulation of blisters or multiple formation of capsules.
Traditional methods
In combination, herbs and certain foods are effective for chronic inflammation of the throat mucosa. Among the popular herbs for preparing rinses :
- chamomile;
- calendula;
- Oak bark;
- eucalyptus;
- sage.
Kalanchoe juice and sea buckthorn oil are used to lubricate the tonsils.
Traditional medicine recommendations include eating foods that help increase immunity and fight local infection:
- black tea (you can drink it or use it for rinsing);
- lemon juice with water;
- milk with turmeric;
- ginger with honey.
However, when using folk remedies, you should remember the need:
- prior consultation with a doctor - sometimes unconventional methods are inappropriate or unsafe;
- monitoring your condition - if signs of allergies appear, you should discard herbs.
Causes of cyst formation
Cystic cavities occur under the influence of the following factors:
- Dental diseases . Infection of the apical tissue (during caries or due to medical errors) contributes to the formation of a cavity with a dense shell, under which fluid accumulates.
- Inflammation of surrounding tissues . With sinusitis, gum pathologies and other similar diseases, the infection penetrates through the bloodstream into the bone tissue. In patients with immunodeficiency, bacteria can enter the jaws from distant sites of inflammation.
- Injuries . Mechanical impact provokes the formation of a cavity in which liquid accumulates over time.
- Congenital malformations of the facial part of the head . This factor in rare cases causes the appearance of cystic cavities.
Complications
One of the most common negative consequences of cysts on the tonsils (tonsils) is suppuration of the cyst with the addition of infection. In this case, pathogenic flora can penetrate into the cavity both from the outside (in case of cyst injury) and hematogenously - through the bloodstream. In this case it is observed:
- deterioration of general condition, weakness;
- headaches;
- signs of intoxication - fever, pain in muscles and joints.
No less serious complications of an untreated cyst can be:
- malignancy;
- decreased general immunity against the background of a constant focus of inflammation;
- relapses of tonsillitis and other ENT diseases;
- the appearance of multiple cavities on one or both tonsils;
- retropharyngeal abscess or phlegmon, meningitis (inflammation of the membranes of the brain) - when an infection of the festering cavity penetrates into neighboring tissues;
- sepsis – blood poisoning;
- breathing or swallowing problems.
A number of these conditions can be life-threatening. In addition, a complicated cyst requires more complex surgical procedures.
Complications of a median cyst
Since a benign tumor in the middle part of the neck can often attach to muscles or nerve endings, during its growth it often provokes the appearance of many dangerous complications and secondary somatic inflammations and ailments.
One of the most dangerous complications of such a cystic body is disorders of the lymphatic system. In such processes, the patient usually:
- general body temperature rises;
- swelling of the skin tissue around the site of tumor attachment may be observed;
- a large number of bruises and mucous discharge may appear on the tissues around, which indicates accelerated growth of the tumor and its swelling.
In most cases, the appearance of such complications indicates that the cyst capsule is filled with a large amount of purulent substance and requires urgent surgical removal or medical intervention. At the same time, as evidenced by the patient reviews left for surgery for a median neck cyst, surgical treatment allows you to get rid of the problem forever. Surgery is the only effective way to prevent recurrence of a median neck cyst.
It is important to note that the symptoms of a median neck cyst are not always expressed in any way. Most diseases of the type described cannot fester or become inflamed on their own unless collateral pressure is applied to them. Thus, often the median neck cyst, due to its external location, becomes an area of mechanical tissue damage or bruises. Tissue injuries lead to the fact that the cystic capsule begins to fill with toxic substances, becomes inflamed and grows.
Due to their high vulnerability, most cystic bodies of the median type are removed in the early stages - immediately after the birth of the baby. When the disease is advanced, a large number of bacteria penetrate into the tissues of the tumor body, which over time can cause not only massive inflammation of the tissues around the site of attachment of the cyst, but also other more complex and dangerous complications, which can be impossible to cure even after complete elimination of the tumor. Therefore, the need to remove the tumor is not discussed.
Prevention
A pregnant woman’s attention to her health will help reduce the risk of congenital cysts - giving up bad habits and uncontrolled use of medications, preventing infections.
Will help reduce the likelihood of acquired cysts:
- maintaining a healthy lifestyle - proper sleep and rest, playing sports, walking in the fresh air, avoiding hypothermia;
- giving up bad habits (smoking) or reducing the number of cigarettes to 2 per day;
- oral hygiene – timely sanitation of caries, teeth cleaning;
- balanced diet, taking vitamins;
- eliminating sources of chronic infection in the body;
- adequate and timely treatment of oropharyngeal diseases.
Chronic tonsillitis can be both a cause and a consequence of cystic formations on the tonsils. A cyst requires consultation with a doctor, regardless of its size and growth tendency - even a small cavity can become a source of infection and contribute to a decrease in overall immunity.
Share the article on social media. networks:
Methods for preventing cysts
It is impossible to prevent the formation of a cyst if the cells were formed at the time of fetal development. However, you can avoid complications during pregnancy:
- a woman should not be exposed to severe stress;
- it is important to monitor your diet, make it balanced, with a minimum content of harmful foods;
- take vitamin complexes for pregnant women with a high content of folic acid;
- complete cessation of alcohol, smoking and other bad habits;
- you need to get enough sleep, lead an active and healthy lifestyle;
- refuse work involving contact with toxic substances: aggressive household chemicals, pharmacological agents, industrial products.
Immediately after the birth of the child, it is necessary to monitor his condition and visit the doctor as scheduled. If the tumor is diagnosed early, complications can be prevented.
A cyst on the neck in an adult and a child is in most cases a benign pathology that requires medical intervention. If it is median, the risk of developing a malignant process is minimal. The lateral growths, on the contrary, are prone to degeneration. Surgical methods are used for therapy. The sooner the patient sees a doctor, the higher the chance of successful recovery without complications.
Diagnostics
The most reliable diagnostic method is dental radiography. Often, a radicular cyst is discovered accidentally during the treatment of other teeth. On an x-ray, this formation appears as a round or oval shadow with clear boundaries, located at the apex of the tooth root or adjacent to the side wall of the root. The bone structure of the periodontal fissure is destroyed and is not visualized on the image. The roots of adjacent teeth are displaced. In some cases, it is not possible to identify a cyst even on an x-ray, due to the fact that the root of the causative tooth is not fully visible. To clarify the diagnosis, the electroodontometry method is used. The excitability threshold of the causative tooth is in the range from 100 to 120 μA, which corresponds to pulp necrosis. To find out whether the cystic formation is malignant, a puncture is performed with a thick needle. The contents of a non-festering radicular cyst are yellow liquid with a suspension of cholesterol grains. To exclude the growth of the formation into the cavity of the paranasal sinuses, it is necessary to additionally conduct radiography of the paranasal sinuses. Radiological signs of a cyst are dome-shaped protrusion and deformation of the bone floor of the sinus. In doubtful cases, contrast radiography or computed tomography of the maxillary bone is recommended.
Differential diagnosis
Differential diagnosis of radicular cysts is carried out with other cystic formations of the jaw and tumors (ameloblastoma and osteoblastoclastoma). Thus, with a follicular cyst, there is no connection between the disease and the inflammatory process in the causative tooth, and with radiography, the crown of a permanent tooth is visualized in the cavity of the cyst. Analysis of the dental arch shows the absence of a permanent tooth, or a baby tooth in its place. Follicular cysts usually occur in childhood and adolescence. Incisive canal cysts form clearly in the area of the midline of the hard palate behind the upper central incisors. Under the base of the wing of the nose in the area of the nasolabial beard there are nasolabial cysts, and in the space between the lateral incisor and the canine of the upper jaw - globulomaxillary cysts. Ameloblastoma is characterized by its location in the area of the angle and body of the lower jaw, and its development is not associated with inflammatory periodontal diseases. On X-ray examination, the tumor appears as a single-chamber cyst or polycystic formation with an unerupted wisdom tooth inside. To clarify the diagnosis, puncture and cytological examination of the obtained contents are necessary. Osteoblastoclastoma differs from a radicular cyst in its cellular structure and less clear boundaries on an x-ray. Once in the tumor area, the roots of the teeth are usually resorbed. When osteoblastoclastomas are punctured, a small amount of brown liquid without cholesterol is obtained.