Basic methods for diagnosing inflammatory lesions of the head and neck
The classification of inflammatory diseases of the maxillofacial area includes the division of diseases into three main categories:
- Acute odontogenic diseases. This group of pathologies includes inflammation of the pulp, ligaments and soft tissues of the oral cavity.
- Purulent-inflammatory lesions in the form of abscesses, phlegmon, actinomycosis, boils and carbuncles. In these cases, the patient develops a limited or diffuse area of suppuration.
- Reactive-dystrophic diseases of the salivary glands and severe complications of inflammation of the tissues of the maxillofacial area (sepsis, thrombosis).
Dental instructions for providing medical care to the population include the following set of diagnostic procedures:
- collecting anamnesis and compiling a medical history;
- visual and instrumental examination of the patient’s face and oral cavity;
- X-ray diagnostics of inflammatory diseases of the jaw and soft tissues using radiography, computed tomography and magnetic resonance imaging;
- ultrasonography;
- a biopsy, which is performed if the doctor suspects the oncological origin of the inflammatory edema;
- general and detailed blood test.
X-ray of the upper and lower jaw
The cost of diagnosis depends on the prevalence and complexity of the pathological process.
Materials and methods
The study was conducted retrospectively on a sample of 44 patients presenting to the San Raffaele Hospital (Milan) between January 2008 and January 2020 with acute severe sinonasal/deep cervical OI requiring admission to the ENT department. The original sample included 60 patients, but we excluded patients whose odontogenic etiopathology could not be clearly determined from the clinical record or those who were subsequently lost to follow-up (minimum follow-up: 6 months). Records were collected from the institution's Consolidated Dental Database.
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the principles set forth in the Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects”, adopted by the 18th World Medical Assembly (Helsinki, Finland, June 1964), and with as amended most recently by the 64th World Medical Assembly (Fortaleza, Brazil, October 2013). Ethics Committee approval was not required due to the purely retrospective nature of the study. All patients were examined by both dentists and ENT doctors. The sample included 21 men (47.7%) and 23 women (52.3%) with a mean age of 51.27 ± 18.72 years (range: 10-85) at the time of hospitalization (53.38 ± 18.70 years for the upper part of the body, 44.42 ± 17.85 years for the lower part).
The extent of the disease and underlying dental pathologies were assessed in all cases using sinus (for upper OA) or cervical contrast-enhanced (for lower AO) computed tomography (CT) and orthopantomography (OPG). Deep neck involvement was also assessed using neck ultrasound or magnetic resonance imaging (MRI) if precise connections to the cervical neurovascular bundle or superior thoracic outlet were required. Re-evaluation of the superior ROI was performed using cone-beam CT whenever possible.
Pathological specimens (ie, pus specimens) aseptically collected from surgical drainage of infectious lesions were analyzed for microbiology and histology. This latter assessment was necessary to differentiate fungal from bacterial sinusitis.
Whenever drug therapy was ineffective due to the persistence of symptoms, and there was a need for surgical treatment (osteomyelitis, implant dislocation, oroantral fistula, suspected fungus, neck abscesses), patients underwent functional endoscopic sinus surgery (FES), in combination with transoral or external (Caldwell-Luc) access for OG, and cervical surgical drainage for cervicofascial odontogenic infections. FEC was typically performed with a minimally invasive approach: lower partial uncinectomy, anterior ethmoidectomy, middle meatus antrostomy extended posteriorly to the vertical process of the palatine bone, maxillary sinus lavage, drainage/removal of pus and infected graft materials. No frontal sinusotomy, posterior ethmoidectomy, or sphenoidotomy was performed. Oral approaches to the upper segment have been used to treat critical areas (namely the alveolar recess of the maxillary sinus, which is difficult to reach endoscopically), narrow oroantral communications (OAC) with removal of the affected mucosa and bone, and reconstruction with a tension-free local flap, removal of dislocated/failed implants and treatment of concomitant dental pathologies. All surgical interventions were performed under general anesthesia with intubation.
Regardless of the surgical approach chosen, all patients received postoperative antibiotic therapy for 8–10 days. In some cases, steroids (usually intravenous methylprednisolone, 40 to 80 mg/day) were administered, especially in patients with severe symptoms.
The average hospital stay was 4.76 ± 6.31 days (3.64 ± 7.27 days for upper OIs, 6.92 ± 3.06 days for lower ones). A case of parapharyngeal abscess with subsequent extension to the mediastinum was excluded from the calculation because it required a 93-day stay. Patients were typically followed up 7, 20, and 60 days after discharge; those undergoing more intensive surgery initially required weekly examinations over a longer period. The mean follow-up duration was 10.7 ± 4.3 months (range 6–15).
Periostitis of the jaw
Specific inflammatory processes in the maxillofacial region mainly occur in the form of limited purulent lesions of the periosteum in the area of 1-3 teeth. Odontogenic periostitis is essentially a complication of inflammatory lesions of the gums and teeth.
The disease manifests itself as follows:
- redness of the gums in the area of the inflamed tooth root;
- progressive soft tissue swelling;
- increase in body temperature;
- pathological mobility and pain of the causative tooth.
Treatment of periostitis is exclusively surgical. The dental surgeon, under local anesthesia, makes an incision in the gums and drains the purulent focus.
Then the patient is recommended to regularly rinse the mouth with saline solutions at home. The specialist removes the rubber strip (drainage) within 3-4 days.
Periostitis of the upper jaw
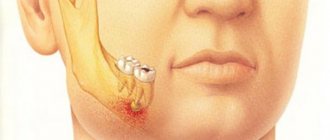
Sometimes a fully formed tooth does not erupt and remains embedded in the bone tissue. In such cases, doctors call them impacted.
Inflammatory lesions are usually caused by semi-impacted teeth. The pathological process develops in the infected or injured mucous membrane that covers the half-cut tooth.
Treatment of inflammatory diseases of the maxillofacial area in such cases is aimed at removing the causative tooth. Radical intervention is carried out in a hospital setting under local regional anesthesia.
Impacted lower wisdom tooth
Osteomyelitis in dentistry is usually called purulent-necrotic damage to the bone tissue of the jaw. The occurrence of the disease is associated with infection of the bone and a systemic decrease in immunity.
The main symptoms of osteomyelitis include:
- intoxication of the body, which is accompanied by a significant increase in body temperature, general malaise and chronic fatigue;
- suppuration of individual areas of the jaw and the release of necrotic masses from the fistulous tracts;
- mobility of one or more teeth;
- periodic attacks of intense pain.
Treatment of purulent-inflammatory diseases of the maxillofacial area is carried out using medication and surgery.
Therapy for osteomyelitis begins with eliminating the cause of inflammation. In such cases, the causative tooth is removed. The dentist then prescribes the patient a course of antibiotics and performs surgical cleansing of the damaged bone tissue.
Single-gene osteomyelitis of the upper jaw
Inflammatory lesions of the maxillary sinus are largely due to its structure and location. Odontogenic sinusitis is caused by pathological microorganisms of the oral cavity that penetrate into the cavity through ingrown tooth roots.
Sinusitis manifests itself with the following clinical picture:
- a feeling of “fullness and pressure” in the maxillary sinus;
- frequent unilateral nasal congestion;
- periodic attacks of pain;
- discharge of pus from one nasal passage.
Treatment of purulent inflammatory diseases of the maxillofacial area in such cases is carried out by two main methods: conservative and surgical treatment. The essence of therapy is to eliminate the cause of the disease, stop the inflammatory process and restore the drainage function of the maxillary cavity.
Odontogenic sinusitis of the maxilla
The submandibular lymph nodes become inflamed when a purulent infection spreads from the primary source of inflammation. The disease begins with a gradual enlargement and pain of regional lymph nodes. Body temperature, as a rule, is within the subfebrile range.
Acute lymphadenitis
Since the submandibular lymph nodes become inflamed due to the penetration of pathological microflora into them, treatment is aimed at eliminating the negative impact of the primary source of infection. Local therapy of lymph nodes is carried out in the form of antibiotics, detoxification of the body and physical procedures.
SPECIFIC INFLAMMATORY PROCESSES OF THE MAXILLOFACIAL AREA
⇐ PreviousPage 28 of 67Next ⇒ACTINOMYCOSIS
General information
Patients with actinomycosis of the maxillofacial area (face, oral cavity, jaws) and neck make up about 60-80% of the total number of patients suffering from this disease.
According to T. G. Robustova and V. V. Roginsky (1976), actinomycosis among inflammatory processes of the maxillofacial area ranges from 6 to 8%, according to L. A. Lutsik, E. V. Gotsko and I. Ya Lomnitsky (1980), - 7.8%. Men get sick approximately 2-3 times more often than women. The age of patients varies (from 3 to 83 years), but people aged 40-50 years are most often affected. Previously, it was believed that actinomycosis was most often contracted by residents of rural areas associated with agricultural (field) work. It has now been established that this incidence is not associated either with the occupation of the patients or with the place of residence
Etiology and pathogenesis
The causative agent of actinomycosis was discovered in 1877 by Bollinger in animals, and in 1878 Israel was the first to discover similar formations in human inflammatory tumors, calling them “human radiant fungus.” These mushrooms are constantly
they grow in the human oral cavity, in the upper respiratory tract, and in the alimentary canal.
In the human oral cavity, the pathogen can be found at the necks of teeth, in gum pockets, in retromolar hoods, and in carious teeth. It is important for the dentist to know that in scrapings from the teeth of healthy (in relation to actinomycosis) people, aerobic radiant fungi can be regularly isolated, among which cultures are found that have the ability to lyse, similar to the lysis of radiant fungi isolated during actinomycosis. This indicates the potential importance of anaerobic radiata fungi of the oral cavity in the etiology of actinomycosis. At the same time, one should also take into account the fact that actinomycetes are present on ears of cereals and grass stems,
from where they can easily penetrate the human body.
Previously, it was believed that infection occurs mainly through exogenous routes. It has now been established that infection of the maxillofacial area and neck with actinomycetes usually occurs
but endogenously, and sometimes exogenously - from the oral cavity (through the hood over the wisdom tooth, gangrenous teeth, gum pockets, ruptures of the mucous membrane, surgical incisions in the oral cavity) or through damaged skin.
A single entry of radiant fungi into tissues is not enough to cause the disease. Only after repeated penetration, when a state of sensitization develops, does the picture of actinomycosis appear. The incubation period lasts 1-3 weeks after the introduction of actinomycetes. Sometimes radiant fungi, once in the maxillofacial or other area, grow into the wall of blood vessels and disperse throughout the body - into the kidneys, lungs, brain, skin, bones, joints, etc., causing a picture of generalized
actinomycosis.
'The constant presence of actinomycetes in the human oral cavity and the relative rarity of actinomycosis are explained by innate immunity to the vast majority of microbes that live on the skin and mucous membranes, which, however, can be disrupted depending on such local unfavorable factors as inflammation and trauma, and mainly - from general causes that reduce the body’s reactivity and increase its sensitivity to the pathogen. In this regard, one should always be wary of a banal chronic odontogenic inflammatory process that for too long
and causes both local and general changes. Actinomycotic inflammation can be added to banal inflammation. The importance of not only specific, but also nonspecific sensitization was proven in experiments on animals by T. G. Robustova.
Ways of spreading infection
with actinomycosis they are: contact, lymphogenous and hematogenous.
Spreading by contact,
actinomycotic drusen penetrate into loose tissue and connective tissue layers of organs and tissues; forming specific granulomas, they affect adjacent tissues and destroy them.
The lymphatic pathway is especially important
spread of friends The hematogenous route is of less importance, however, the possibility of germination of radiant fungi into the vessel wall and their metastasis to other organs along the bloodstream is quite likely.
Part IV. Inflammatory diseases
Rice. 53 Cervicofacial form of actinomycosis-a, b —
uncomplicated form, c - the same patient during the period of complicated actinomycosis
Pathological anatomy.
There are two forms of morphological manifestation of actinomycosis: purulent-necrotic and fibrous. At the site of the introduction of the radiant fungus, characteristic dense, inactive or completely immobile granulomas and infiltrates, inflammatory tumors appear. In the center they contain drusen of fungi - spherical plexuses of many individual actinomycete fungi, forming dense grains of a yellowish-gray color, the size of a millet grain or smaller. Lymphocytes or plasma cells accumulate around the drusen, as well as xanthoma cells, that is, connective tissue cells, in in the protoplasm of which there are droplets of fat - lipoids. Specific granuloma-nodules undergo necrobiosis and melting over time, but new granulomas appear next to them, the melted granulomas destroy the skin and form fistulous tracts on the skin or mucous membrane. If the peripheral layer of granulomas, consisting of connective tissue, grows and thickens, the inflammatory infiltrate acquires a woody density (fibrous form)
The described two morphological forms (purulent-necrotic and fibrous) in various combinations are found in humans, which is why the clinical manifestations of actinomycosis are very diverse.
Classification of actinomycosis of the head and neck
Actinomycosis of the head and neck is divided into three groups depending on the depth of the lesion:
1) deep,
or muscular, a form localized in the thickness of the muscles and intermuscular tissue, 2)
subcutaneous
form - localized in the subcutaneous base;
3) cutaneous
form - involves only the skin. K. I. Berdygan (1958) classified actinomycosis of the maxillofacial and cervical areas as follows:
1) cutaneous form; 2) musculocutaneous form;
3) musculoskeletal, which in turn is divided into: a) destructive and 6) neoplastic; 4) generalized form, grab
protecting skin, muscles, bone, oral mucosa.
According to our observations, the most comprehensive classification should be recognized as proposed by T. G. Robustova (1992): cutaneous (occurs in 0.3% of patients with actinomycosis of the maxillofacial region), subcutaneous (in 16.9%), submucosal (0 6%), mucous ( 0.3%), odontogenic actinomycosis granuloma, localized in the skin and subcutaneous tissue, submucosal tissue and subperiosteum (8.9%), subcutaneous (28.9%), actinomycosis of the lymph nodes (30.7%), actinomycosis of the periosteum of the jaw (0.9% ), actinomycosis of the jaw bone (6.9%), actinomycosis of the organs of the oral cavity and other parts of the maxillofacial area (tongue, salivary glands, tonsils, maxillary sinuses, appendages of the eyes) - 36.5% This classification involves distinguishing among skin forms - pustular, tubercular and mixed , and among the subcutaneous forms - abscess-forming, gummous and mixed.
Among the complications of the subcutaneous intermuscular form
actinomycosis includes: secondary actinomycotic damage to the bones of the facial skeleton, as well as metastasis and generalization of the actinomycotic process.
Clinic
According to the clinical course, actinomycosis should be distinguished, uncomplicated
secondary infection, and actinomycosis
complicated by
secondary infection. In addition, depending on the severity of clinical symptoms and their severity, it is necessary to distinguish between mild, moderate and severe forms of actinomycosis.
Clinic of uncomplicated actinomycosis.
Most often, painless or
Yu. I. Vernadsky. Fundamentals of shuttle-facial surgery and surgical dentistry
mild infiltrate, within 1-2 lymph nodes. At first, it looks like a limited node, dense, mobile, not fused with the surrounding tissues. At a later stage, the process does not have sharp boundaries, becoming diffuse and not contoured. Palpation reveals a “woody* density infiltrate, painless or slightly painful
when pressed.
Localized in the parotid, post-mandibular regions, and retromolar triangle, the inflammatory process spreads to the masticatory muscles and causes a relatively early symptom - painless trismus
later, swelling of half the face, eyelids, and impaired facial muscles appear. Significant infiltration of the neck makes it difficult to turn the head. An attempt to open the mouth does not, as a rule, cause a painful reaction. The body temperature is subfebrile, the general condition of the patient is satisfactory, but patients gradually lose weight due to the inability to eat normally. After various periods from the moment the infiltrate appears, it softens, and the skin above it acquires a red-bluish-violet hue, multiple skin and intraoral fistulas appear, through which a kind of pus with grains of drusen is released outward or into the oral cavity. The skin around the fistulas is thinned. The amount of pus is sometimes significant, sometimes scanty, sometimes completely disappears, after which the fistulas close, but after a while they recur, appearing nearby. If the process is localized under the skin and does not involve the masticatory muscles, there is no trismus, but subcutaneous spherical infiltrates soften faster and are more quickly complicated by fistulas.
Clinic of complicated actinomycosis
(Fig. 53 c).
If actinomycosis is accompanied by a secondary infection, the disease is more severe, with high body temperature and intoxication. After incisions or spontaneous opening of abscesses and phlegmons, persistent non-healing fistulas remain. A complicated form of actinomycosis should also be considered one in which the jaw, orbital bone, zygomatic bone, temporal and frontal bones, as well as more distant parts of the body are involved in the process, i.e. when the process generalizes (actinomycotic sepsis). Since 1970, cases of metastasis
of actinomycosis to the brain and abdominal organs have become more frequent.
Amyloidosis is a severe and dangerous complication of actinomycosis of the maxillofacial area and neck.
internal organs, usually developing against the background of severe concomitant diseases; obviously, actinomycosis and a decrease in the immunobiological resistance of these patients determine the constant absorption
products of tissue decay enter their body, which entails profound metabolic disorders in the body, and above all, protein metabolism. Consequently, even without the addition of a secondary infection, they represent a very severe chronic disease.
Diagnosis and differential diagnosis
Only about 8% of patients with actinomycosis are correctly diagnosed outside the clinic. This is explained by the fact that many doctors mistakenly imagine actinomycosis as a disease that begins and ends in the same way.
However, actinomycosis manifests itself in a very diverse manner, which goes far beyond the cliché concepts common to a practicing physician. Therefore, every practitioner must learn to distinguish actinomycosis from banal (nonspecific) inflammatory processes - retromolar periostitis due to difficult eruption of the lower wisdom tooth, acute and chronic odontogenic osteomyelitis, odontogenic subcutaneous migratory granuloma, tuberculosis of the jaw, tongue, lymph nodes, maxillary sinuses, etc.
To do this, you should first of all always firmly remember that all acute odontogenic processes
They are distinguished by a special anamnesis, the presence of a gangrenous tooth, high body temperature, pain, changes in the blood picture, which quickly decline after surgery and drug treatment.
For chronic osteomyelitis
the jaw is characterized by the following symptoms: a single fistula, the presence of osteoporosis and sequestration or granulations protruding from the fistula; the skin does not have a bluish tint, and the infiltrate does not have a woody density and many fistulas. Sequestrectomy and curettage lead to recovery.
Odontogenic subcutaneous granuloma
(see Chapter XVIII) always has a cord leading to the “causal” - gangrenous tooth; tooth removal usually leads to a cure.
Tuberculosis of the jaw
(see below) is also characterized by a number of specific symptoms, as is its damage to the lymph nodes (see Chapter XVII).
Despite the fairly clear clinical symptoms of the listed diseases, in many cases the exact substantiation of the diagnosis of actinomycosis presents significant difficulties, and therefore the doctor has to resort to a number of special studies (microbiological, immunological, histological, etc.).
Microscopy data.
If there is a fistula, drusen of actinomycetes can be found in the pus; if there is no fistula yet, pus is extracted by puncture or through an incision. Visible in pus
Part IV Inflammatory diseases
The grains are yellowish-gray. They are placed on a glass slide and pressed down with a coverslip; 1-2 drops of a 5% solution of potassium hydroxide, which dissolves white and red blood cells, or distilled water are placed under a glass slide (T. G. Robustova, 1958). Under a microscope, drusen, that is, colonies of the fungus, are visible; they are round in shape, structureless in the center and branched-radial along the periphery. Under high magnification, branching thin threads of mycelium in the form of a felt ball are visible in the center of the colony, from which club-shaped formations with flask-shaped swellings at the ends extend.
An experienced eye can also notice xanthoma cells characteristic of actinomcosis.
It must be taken into account that in some cases, the detection of radiant fungus is not the basis for establishing a diagnosis of actinomycosis, since in some patients with the presence of a jaw cyst, chronic osteomyelitis, cancer and other diseases, actinomycotic drusen can sometimes be found in the discharge. In these cases, the presence fungus should be considered a secondary infection.
Biopsy data:
Under the microscope, characteristic actinomycotic granulomas are visible.
Data from skin allergic reaction • immunodiagnostics
Allergic skin reaction according to D.I. Asnin: 0.3 ml of actinolysate (filtrate of lysed cultures of radiant fungi isolated from human actinomycotic foci) is injected into the thickness of the skin on the flexor surface of the forearm. Nearby, at a distance of 10 cm, 0.3 ml of meat-peptone broth is injected. Soon blisters appear at the injection sites, which disappear after 1-2 hours. The erythema that replaces them lasts up to 12 hours and also disappears. If a person is sick, erythema at the site of actinolysate administration disappears only after 36-48 hours.
According to D.I. Asnin, clear results of this test are obtained in 92.1% of patients. Moreover, in 13.5% there is not only a local allergic reaction at the site of actinolysate injection, but also a general one, accompanied by an increase in body temperature to 37.5-40°C. However, in other diseases this allergic skin reaction can be positive. Thus, with pulmonary tuberculosis it is positive in 122% of patients, with skin tuberculosis - in 25.6%, with cancer and other diseases - in 12% of patients. N.V. Garifulina (1966) found a positive skin allergic reaction in 80.77% of patients with various inflammatory processes in the face and neck. Along with this, only 68.7% of the patients who actually suffered from actinomycosis had a positive skin allergic reaction, while the rest had a negative reaction. In light of these data, there is reason to doubt the strict specificity of the allergic skin reaction with actinolysate in actinomycosis of the face and neck. A more specific diagnostic antigen than akginolysate is a special actinomycete polyvalent vaccine (APV), created in 1959 at the Institute of Medical Parasitology and Tropical Medicine.
A serological or immunological reaction is carried out with a polyvalent actinolysate (as an antigen) and the patient’s blood serum. This reaction was first proposed in 1922 by Walker, and then developed by S. F. Dmitriev, M. F. Firyukova, G. O. Suteev, D. I. Lenin, etc. Evaluation of the result of this complement fixation reaction occurs immediately after the onset of hemolysis in the control tube. This reaction will provide clear and accurate data in 92-80% of cases of actinomycosis. The greatest number of positive serological reactions can be obtained in patients with a significant history of actinomycosis, which characterizes this reaction as especially valuable for diagnosing advanced forms of this disease. The skin allergic reaction in these patients is often negative, and microbiological diagnosis is difficult.
Consequently, there is not yet an ideally accurate test for actinomycosis. Therefore, in some cases it is necessary to resort to a series of diagnostic methods: an immunodiagnostic skin test, a serological reaction with actinolysate (as an antigen), and inoculation of pathological material (pus, sputum) on appropriate nutrient media. With the help of such a complex of studies, it is possible to establish a diagnosis of actinomycosis even in its early, hidden and erased forms
Considering the large number of diagnostic errors in actinomycosis, which is so multifaceted in its symptoms and localization, S. A. Burova (1983), together with 28 dental specialists, subjected 125 symptoms to mathematical processing and identified 35 symptoms from them, the most significant for the diagnosis of “actinomycosis”, i.e., which are the most informative for the differential diagnosis of actinomycosis with other diseases of the maxillofacial region. The average weight of the main ones is characterized by the following figures (M±t): the course of the disease is chronic - in 12.8±0.89%; the skin over the lesion is bluish - in 12.04±0.85%;
history of one or more exacerbations - 12.00±0.96%; disease duration 3-4 months - 11.68±0.99%; the onset of the disease is gradual - 11.07±0.93%; slight pain in the lesion - 11.54±0.95%; the course of the disease is recurrent, the infiltrate is dense, there are many fistulas on the skin - 11.68±0.99%;
the cause of the disease is a fracture of the lower jaw or tooth extraction - 11.04±1.04%; after opening the lesion, the infiltrate decreases slightly - in 10.93±1.06%; skin over the lesion: violet - 10.571:1.01%, dense - 10.07±1.07%, lumpy - 9.04±1.24%, roller-shaped folded - 10.43±1.13%; fluctuation in the form of small foci (10.25±1.10%) superficial - 9.89±1.12%; the cause of the disease is pericoronitis - 10.89±1.08%; disease duration 1-2 months - 9.43±1.15%, and 10 months -9.04±1.24%; preservation of working capacity in the presence of a lesion - 9.25±1.19%; difficult
Yu I Vernadsky Fundamentals of maxillofacial surgery and surgical dentistry
full mouth opening - 9.61± 1.11%; deep infiltrate - 907±1.23% and painless - 9 86±1 20%, presence of one fistula - 907±2.15%; discharge from the fistula is crumbly - 11 04 ± 1 11% or purulent - 896 ± 1.10%, drusen of the radiant fungus were found - 11.86 ± 0.92%, the boundaries of the infiltrate are clear - 964 ± 1 10%.
As you can see, not a single symptom is strictly obligatory, and therefore pathognomonic for actinomycosis. Therefore, the diagnosis of actinomycosis can be made only on the basis of the presence of a combination of several symptoms
Treatment
Treatment of actinomycosis should be combined, that is, it is necessary to combine the following conservative and surgical measures
Intradermal actinolysate therapy according to Lenin
20-25 injections at intervals of 2-3 days. During the first injection (made, like subsequent ones, through a thin needle of a tuberculin syringe), 0.5 ml is administered; the second - 0.7 ml, the third - 0.9 ml of actinolysate. The dose of each subsequent injection increases by 0 1 ml, by the 14th injection it reaches 2 ml and remains so until the end of treatment
A. I. Evdokimov and G. A. Vasiliev (1959) present another, more intensive scheme of actinolysate therapy. After the first course - a break of 1-2 months
Intradermal injections are indicated for the cutaneous form of actinomycosis, and intramuscular and subcutaneous injections of actinolysate are indicated for deeper lesions; actinolysate is administered 3 ml 2 times a week, a total of 15-20 injections. After clinical recovery, a course of prophylactic actinolysate treatment is indicated.
Actinolysis therapy for maxillofacial actinomycosis gives good results. The effect of actinolysates is based on an increase in the immunogenic activity of the body, which explains the highest percentage of lasting recovery.
polyvalent vaccine can also be used as a specific immunotherapeutic agent
(AL B), which in its therapeutic effect is not inferior to actinolysate, and even surpasses it in reducing treatment time. APV can be used in a hospital and clinic, alone or in combination with other treatment methods
Methodology. APV is injected into the thickness of the skin of the flexor surfaces of the forearms in increasing doses - at the first injection - 0.1 ml, with each subsequent injection 0.1 ml is added, bringing the dose to 1 ml (1 ml of APV contains 1 billion microbial bodies) In the future, this
the dose is not changed until the end of the course of treatment. 0.1 ml of vaccine is injected into each point, each time to a new place, the 10th dose is administered into 10 points spaced 4-5 cm from each other (5 points on each forearm ) After a few hours, a dense dark red papule appears at the injection site, resolving within 4-7 days. APV is administered 2 times a week (with an interval of 3-4 days). The course of treatment is 20-25 injections. If after this treatment there is no recovery has occurred, treatment is resumed a month later according to the same regimen. When clinical recovery is achieved, a preventive course of immunotherapy is administered (10 injections).
Antibiotic therapy
directed against secondary infection and actinomycetes. The fact is that a secondary infection can reduce the reactivity and resistance of the body, and thereby worsen the course of the actinomycotic process. Antibiotics affect the secondary infection, thereby mobilizing the reduced reserve forces of the body to fight actinomycetes.
In addition, broad-spectrum antibiotics can also inhibit the growth of actinomycetes. Therefore, surgeons successfully carry out intensive complex antibiotic therapy for both secondary inflammatory layers in actinomycosis and the underlying disease. Only broad-
spectrum antibacterial drugs should be prescribed, since in addition to actinomycetes,
a wide variety of microorganisms
Purpose of ftivazid
This drug is usually prescribed for tuberculosis, however, due to the biological relationship of the actinomycete with the tuberculosis bacillus, ftivazid has a good anti-actinomycosis effect. Prescribe it 0.3 g 3 times or 0.5 g 2 times a day, gradually increasing the dose (up to 2 g per day), monitoring the condition patient The course of treatment is from 3 to 8 months.
X-ray therapy
prescribed in combination with immunotherapy and antibiotics or in combination with potassium iodide, which is administered, according to K. I. Berdygan, in the form of a 4-5% solution (per os) 1 tablespoon 4-6 times a day, sodium can also be prescribed iodide, but intravenously - 10% solution in ascending doses from 10 to 50 ml daily. Radiation treatment is prescribed (0 4-0 5 Gy), after the elimination of the acute process - 1-15 Gy. Total dose - up to 15 Gy per field.
Stimulant therapy
carried out in the form of autohemotherapy, blood transfusion, enhanced nutrition, etc. As indicated by T. G. Robustova et al.
(1983), when treating actinomycosis, it is necessary to include physiotherapeutic components in a complex of therapeutic measures strictly according to indications.
They are indicated for normo- and hyperergic inflammation, but are contraindicated for hypoergic inflammation and anergy in patients with other concomitant
Part IV. Inflammatory diseases
diseases. In addition, it is not recommended to use physical methods in children with actinomycosis periostitis, productive-destructive bone actinomycosis.
UV irradiation
indicated (as a desensitizing, restorative, anti-inflammatory and stimulating agent) at the stage of formation of superficial actinomycosis foci, as well as for abscessing lymphadenitis of the superficial lymph nodes.
Fluctuation
indicated for submucosal form, odontogenic actinomycosis granuloma, lesions of the periosteum of the jaws, tongue and tonsils
Ultrasound
(5-10 procedures) daily using a stable method (pulse mode, intensity 0.05-0.5 W/cm2 for 10 minutes) it is advisable to use for resorption of residual sluggish infiltrates, with persistent actinomycotic lymphadenitis
Helium-neon laser treatment
gives good results with odontogenic subcutaneous granuloma, subcutaneous-intermuscular form, damage to the lymph nodes and salivary glands. Usually, 5-10 ultrasound procedures of 3 minutes each at an exposure density of 0.3 mW/cm2, using iodine and hydrocortisone preparations, are sufficient.
Electrophoresis with
calcium chloride, dimexide, diphenhydramine (5-10 procedures) is useful to complete with 10-15 sessions of electrophoresis with iodine or lidase with greater severity of scar-productive changes in the subcutaneous and dermal layers of actinomycosis lesions. With hyperplastic actinomycosis lymphadenitis, the best results are obtained after io - nophoresis with calcium chloride, diphenhydramine, dimexide (5-10 sessions), and then iodine, lidase or other enzymes. Dense skin scars and periostitis thickenings after bone actinomycosis in adults are easily reabsorbed after 5-10 sessions of iono- and phonophoresis with hydrocortisone. For residual intraosseous lesions, it is necessary to combine iontophoresis with dimexide, lidase (10-15 sessions), phonophoresis with hydrocortisone (10-15 sessions).
Surgery
consists of evacuating the contents of leaks and abscesses; it is better to do this by suction rather than incisions, since a secondary infection may occur through the incision. The festering lymph nodes of the face are opened and scraped out. With extensive and advanced actinomycosis of the head and neck, it is often necessary to simultaneously carry out a set of measures in order to remove the layer of a banal inflammatory process, suppress the main actinomycotic process, and increase the body’s resistance and regenerative abilities.
Physiotherapy
is indicated as an element of complex treatment throughout the entire illness, excluding periods of exacerbation due to the addition of a secondary infection. The methodologist and the patient himself must carry out exercises, the scheme and complex of which are presented in table. 11, 12 Among active and active-passive physical exercises in complexes of therapeutic gymnastics and during independent exercises on assignments, systematically perform special exercises for the facial and masticatory muscles 4-5 times a day in accordance with the recommended topic of the lesson and the content of the approximate complex of therapeutic gymnastics It is recommended to use special exercises for facial muscles symmetrically for the healthy and affected halves of the face. For medical reasons, the complex use of therapeutic physical education with physiotherapy, therapeutic massage and other therapeutic methods of treatment is allowed.
Prevention
Prevention of actinomycosis consists primarily of sanitation of the oral cavity and the implementation of a set of general strengthening measures, oral hygiene, where the causative agent of actinomycosis is always present.
⇐ Previous28Next ⇒
Abscesses and phlegmons of the face and neck
Specific inflammatory processes of the maxillofacial area in the form of abscesses and phlegmons are areas of diffuse or local suppuration of soft tissues. Such lesions are manifested by severe swelling, hyperthermia, limited opening of the oral cavity, impaired swallowing of food and attacks of intense pain.
Such diseases require immediate surgical intervention, which is performed in the following sequence:
- local conduction anesthesia;
- radical dissection of soft tissue in the area of edema;
- opening the abscess and draining it;
- fixation of a special tube for drainage of pus.
When treating abscesses and phlegmons, the doctor simultaneously prescribes antibiotic therapy to the patient for 7-8 days.
Etiology and features of the clinical course and treatment of odontogenic diseases of the head and neck
Odontogenic inflammatory diseases of the jaws and soft tissues of the face, as a rule, develop as a result of infection of the patient with pathological microorganisms of the oral cavity and skin. This group of diseases includes:
Inflammation of the ligamentous apparatus of the tooth, which is located in the periodontal fissure, is predominantly of infectious origin. In such cases, the source of infection is the dental pulp.
The clinical picture of the disease is represented by the following symptoms:
Treatment of the disease involves creating an outflow of purulent masses through the cavity and subsequent filling of the root canals.
Therapy for periodontitis is predominantly conservative. Doctors perform radical intervention only in the presence of a concomitant root cyst or purulent inflammation of the soft tissues of the oral cavity.
Negative consequences of inflammatory processes in the soft and hard tissues of the head
Complications of inflammatory diseases of the maxillofacial area occur in the following main forms:
- Sepsis is a severe generalized infectious lesion, which is combined with the penetration of pathological microorganisms into the circulatory system. This pathology often causes death.
- Mediastenitis is a purulent inflammation of the mediastinum, the cause of which lies in the odontogenic spread of infection.
- Thrombosis and thrombophlebitis of the facial veins. Inflammatory damage to blood vessels is a complication of abscesses and phlegmon of the soft tissues of the face.
The prognosis for inflammatory lesions is predominantly favorable. The exception is advanced cases when the patient exhibits signs of sepsis or mediastenitis.
In 9 out of 10 patients who seek help in dental surgery departments, doctors diagnose inflammatory diseases of the maxillofacial area. If in the 50s of the last century mortality was completely eliminated by the massive use of antibiotics, today pathogenic microflora has become less susceptible to antibiotic therapy. Because of this, the problem of purulent intracranial complications has returned to the level of the 30-40s, when the incidence of deaths was more than 20%.