Herpetic gingivostomatitis is a disease of the oral mucosa caused by the Herpes simplex virus. Acute herpetic gingivostomatitis (AHG) most often occurs in children, but can also occur in adults.
Stomatitis of any origin causes the patient quite severe discomfort.
The disease is caused by viruses belonging to the herpesvirus family. They include the following 8 types:
- HSV-1 and HSV-2;
- varicella-zoster virus;
- Epstein-Barr virus;
- CMV;
- herpes virus type 6, 7, 8.
Approximately 80-90% of adults have had herpes simplex.
It is possible to become infected from absolutely any virus carrier. From relatives, friends, co-workers and even pets sick with the virus, when saliva gets on the skin and mucous membranes of a healthy person. The source of infection is primarily the patient. The pathogen may not be released for a long time. Therefore, it is almost impossible to recognize the carrier. Only pronounced symptoms of herpes, located on open areas of the patient’s body, will make it possible to find out about the presence of the virus.
How can you get infected with a virus?
An increased risk of infection is direct entry of the virus into the oral cavity through kissing or using an infected toothbrush. The ability of the Herpes virus to be transmitted to others is very high. You can become infected in crowded places. As the weather gets colder, the risk of infection increases. The virus is highly contagious and is transmitted in the following ways:
- contact with infected people;
- due to sexual contact, with damage to the skin;
- by airborne droplets, inhalation or through household items;
- hematogenous method (through blood);
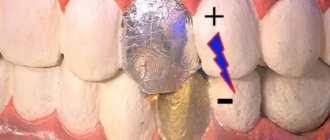
- as a result of using toothpastes containing sodium lauryl sulfate.
Prevention
As mentioned above, herpetic sore throat is transmitted from person to person by contact or airborne droplets, then the main method of prevention is the introduction of quarantine, that is, isolation of a sick family member or team, limiting contacts with him.
Preventive measures also include:
- systematic strengthening and maintenance of immunity.
- Maintaining a routine means getting enough sleep.
- Proper nutrition.
- Getting rid of bad habits - smoking, drinking alcohol.
- Maintaining cleanliness in the house, regular ventilation and wet cleaning.
- Reducing stress levels.
- Timely treatment of colds.
If a child shows signs of a cold, he should not be taken to kindergarten or school. It is better to take the baby to the doctor and let him rest at home. Such measures will allow the child’s body to regain strength. In addition, the likelihood of infecting other children will be reduced.
RCHD (Republican Center for Health Development of the Ministry of Health of the Republic of Kazakhstan) Version: Clinical protocols of the Ministry of Health of the Republic of Kazakhstan - 2015
First symptoms of the disease
From the 1st to the 8th day of the presence of the virus in the blood, it is difficult to recognize the disease due to the appearance of common symptoms: weakness, lethargy, headaches, drowsiness. Later, other symptoms are felt that most clearly indicate acute gingivostomatitis, such as:
- pain when swallowing;
- a sharp increase in temperature up to 40 degrees;
- vomiting and seizures;
- swelling of the oral mucosa;
- white coating on the tongue and cheeks;
- poor sleep, lethargy, decreased appetite;
- enlarged lymph nodes.
The main indicator of the disease is damage to the surface of the tongue by erosions along the gum edge and on the oral mucosa. After the first day, this manifestation can be distinguished by the following symptoms of an extensive process:
- rashes of the mouth, cheeks and palate;
- plaque on the tonsils;
- painful ulcers;
- bubbles with liquid;
- viscous saliva.
Manifestations of the disease last for 5-10 days. During this period, the face and sometimes the hands may be affected. Other mucous membranes, located, for example, in the gastrointestinal tract, may also be affected. Painful sensations occur along the intestines. Later, the pharynx, larynx, urethra, female genital organs, and cornea are involved.
Herpetic stomatitis in children: symptoms and treatment
The period that precedes the development of objective clinical symptoms in the oral cavity is called prodrome, and during this period patients may experience symptoms such as fever, lack of appetite, muscle pain, irritability, malaise and headache. These symptoms are equally characteristic of both children and adults, and they appear even before the formation of herpetic blisters on the oral mucosa.
Many patients note that in the places where the bubbles appear, they always first feel a slight burning, itching or tingling of the mucous membrane. It is very important to teach patients to feel this moment in order to begin treatment of herpetic stomatitis in this very initial period. It is in this case that treatment will be truly effective.
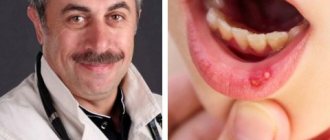
When examined in the oral cavity, the main objective symptom of herpetic stomatitis is the formation on the mucous membrane of the gums, cheeks, palate, tongue or throat - numerous small blisters (Fig. 4), which quickly open, turning into painful ulcerations (Fig. 1-3 ). The blisters are initially small, about 1 mm in size, then they enlarge and open - as a result of which numerous small ulcerations merge with each other, forming large ulcerations with jagged boundaries (Fig. 5-6).
Herpetic lesions are bright red in color and are usually very painful. It is because of the pain that many children begin to refuse to drink water, as a result of which their general condition worsens even more, and symptoms of dehydration also develop (according to statistics, in approximately 86% of children). Due to pain, children may also refuse to eat, they are diagnosed with bad breath (halitosis), and the submandibular lymph nodes are enlarged.
If herpetic stomatitis in children also causes dehydration, then in parallel there are symptoms of dry mouth + very little urine is produced. However, otherwise, with stomatitis in children, on the contrary, drooling is often observed. Then the following happens - the ulcerations are gradually covered with yellowish-gray films (Fig. 5-6). The total duration of the disease from the moment the blisters appear to the epithelization of the ulcers is 8-14 days, but in patients with weakened immunity, stomatitis usually takes a longer and more severe course.
If one of the localization sites for herpetic stomatitis is the gums, then severe swelling, redness + bleeding may be observed when brushing your teeth. In this case, a diagnosis of herpetic gingivostomatitis is made (Fig. 5-7). In addition, herpetic stomatitis in adults and children, as a rule, is almost always combined with the appearance of ordinary herpetic rashes in the corners of the mouth and on the red border of the lips (Fig. 8).
Important: an interesting point is that the child is born with a sterile oral cavity, and his infection with the herpes simplex virus occurs from his parents. Remember this when you lick your baby's spoon or put his pacifier in your mouth. In addition, it is worth knowing that, unlike the non-contagious aphthous form of stomatitis, herpes stomatitis in children and adults is extremely contagious. The most contagious period is from the moment the vesicles burst until they are completely healed.
Therefore, if you have several children, you should at least limit their contacts. In addition, if a child touches herpetic rashes near the mouth or licks his fingers, and then rubs his eyes with these hands, the development of herpetic eye lesions is possible. In this regard, in young children it is often recommended to instill special antiviral drops into the eyes for prevention.
Features of herpetic stomatitis in children -
As we said above, viral stomatitis in children, symptoms of intoxication can be aggravated by the development of dehydration due to the child’s refusal to drink water and eat food. In these cases, even with fairly small herpetic lesions, the child may have a high fever and feel unwell.
In addition, children more often than adults simultaneously develop herpetic gingivostomatitis and pharyngotonisillitis. Gingivostomatitis means that in addition to the occurrence of herpetic blisters and ulcerations (for example, on the mucous membrane of the lips, cheeks or tongue), severe swelling and redness of the entire marginal gum around the teeth may occur.
Features of herpetic stomatitis in adults -
As we said above, herpetic viral stomatitis in the oral cavity is most often caused by the herpes simplex virus type HSV-1, less often by the type HSV-2. The latter, according to statistics, causes about 10% of all cases of herpetic stomatitis, and it occurs mainly in adults. HSV-2 is the type of virus that is most often responsible for the development of genital herpes, but the spread of oral sex has led to the fact that this type of virus can also cause stomatitis.
Why this is worth special mention... The fact is that the HSV-2 virus type is much more virulent than the HSV-1 virus type. Herpetic stomatitis in adults caused by the herpes virus HSV-2 is much more severe and is much more difficult to treat. Also, the HSV-2 virus develops resistance to major antiviral drugs, for example, Acyclovir, much more quickly.
If in children Acyclovir is quite effective, then in adults the resistance of herpes simplex viruses to Acyclovir reaches up to 10%, and some recent clinical studies show that this figure in some groups of patients can reach 30-36%. It has been noted that drug resistance to acyclovir develops more often in those who have already repeatedly taken courses of this drug, in patients with weakened immunity, as well as in patients with the herpes simplex virus type HSV-2.
Forms of disease severity
Depending on the severity of toxicosis and the area of damage to the surface of the mouth, the disease is divided into the following forms:
- incubation period;
- light;
- average;
- heavy.
Incubation period
The incubation stage lasts about a week. The disease develops rapidly, often with a temperature reaching 39 degrees and severe malaise. After two days, discomfort occurs in the mouth, increasing while eating and when talking. Rashes occur on the edematous mucosa, single or in quantities from 2 to several dozen. It is not difficult to notice them, as they quickly turn into ulcers that appear on the tongue, palate and face. The gums are affected from the inside, becoming covered with purulent plaque. Salivation is viscous, increasing over time. This process lasts another 5-10 days after inflammation of the ulcers.
Mild form of the disease
It is difficult to notice the mild stage of the pathological process due to the mild symptoms of the course.
There are either no rashes, or there are 1-2 flat ulcers that appear as a painless small spot on the inner surface of the mouth.
After a few hours, the inflammatory process intensifies, and the ulcers become painful and fill with fluid inside. At the same time, the lymph nodes become enlarged. After 2-3 days, the stage of healing of ulcers-erosions begins. Relapses of this form of the disease depend entirely on the human immune system.
Medium severity
It is characterized by prolonged healing of ulcers up to 2-3 weeks, and especially deep erosions disappear in a month or more. With this form, patients still suffer from regular relapses every month. Erosion ulcers go deep into the mucous membrane, causing severe pain upon contact. Exacerbations of the moderate form occur immediately - the ulcers become denser, corroding the mucous surface of the erosion, and then deepen. Later, the ulcers heal with the formation of scars.
Severe illness
Severe disease is less common than others, but is characterized by the sudden formation of several ulcers on the oral mucosa. Patients suffering from allergies, gastrointestinal diseases, rheumatism, and viral infections are susceptible to such manifestations. The primary symptoms are:
- lethargic state;
- heat;
- headache;
- joint pain;
- pain in the mouth;
- poor appetite;
- apathy and depression;
- sleep disturbance.
A blood test diagnoses an increase in leukocytes and an increase in the erythrocyte sedimentation rate, which clearly indicates a pronounced inflammatory process. Upon examination, newly formed foci of ulcers of various sizes are noticeable.
How can you relieve your baby's condition?
Before taking any medications, be sure to consult with your pediatrician. Depending on the severity of the manifestations and the cause of stomatitis in your child, treatment tactics will depend.
Medications are applied to the mucous membrane after feeding.
Thrush can be treated with a soda solution. Prepare the solution yourself by stirring a teaspoon of baking soda in 200 ml of warm water.
After wrapping a bandage around your finger, soak it in the solution and wipe the baby’s mouth after each feeding. You can alternate a soda solution with vitamin B12 (cyanocobalamin). If there is no result within three days, local use of nystatin or systemic use of other antifungal agents is necessary (only as prescribed by a doctor).
For herpetic stomatitis, antiviral ointments are used (Oxolinic ointment 0.25%).
To treat the oral cavity after feeding, you can use a 0.05% solution of chlorhexidine digluconate, a decoction of calendula, chamomile, oak bark, or freshly brewed tea.
To reduce pain, a gel based on benzocaine or lidocaine, which are used for teething, will help. The gel is applied to the affected areas. Before use, be sure to read the instructions for the drug, paying attention to the age at which it is allowed to be used.
At the resolution stage, Actovegin gel, Solcoseryl gel and ointment are used to speed up the healing process.
Acute herpetic gingivostomatitis in children
AHS in children is the most common and common infectious disease in childhood and infancy. It begins with an inflammatory process of the oral mucosa with the appearance of blistering rashes, an increase in temperature and a decrease in general immunity.
Most often, primary infection with the virus occurs after six months of a child’s life. This is explained by the fact that before this, antibodies to the virus acquired in utero are present in the newborn’s blood, so infants are considered protected by maternal immunity.
The incidence of infection in children is as follows:
- from 1 year to 5 years - 62-65%;
- from 5 to 7 years - 13-25%, after which the incidence decreases;
- in adolescents 1-2%.
Repeated infection from six months to 3 years is explained by the disappearance of antibodies acquired from the mother transplacentally, as well as the immaturity of the immune system. The disease rarely occurs in newborn premature babies.
The disease manifests itself in the following forms:
- Acute herpetic gingivostomatitis is a primary herpetic infection caused by a virus for the first time.
- Chronic recurrent herpes.
- Generalized herpes - manifests itself in an infant born to a mother who did not have antibodies to the Herpes simplex virus. That is, the baby did not receive passive maternal immunity. Extensive necrosis appears in the oral cavity. This form provokes the development of a complex septic disease with damage to internal organs and serous meninges. Possible death.
Symptoms of acute herpetic gingivostomatitis in children, depending on the severity, are divided into the following forms:
Mild illness
The general condition of the child is slightly disturbed, the temperature is often within normal limits. The first symptom is pain when swallowing. During the examination, swelling of the mucous membrane and the formation of small erosions covered with a light coating can be observed. The disease lasts no more than five days.
Medium to heavy
These forms of the disease are the most common. The disease begins acutely with a body temperature of more than 38 degrees, and in severe situations reaches 40 degrees. The child becomes lethargic and capricious. Complaints of pain appear, and appetite sharply decreases. There is a possibility of nausea and vomiting. Later, symptoms of ARVI appear.
In this case, the help of a pediatrician is needed, who, after a thorough examination, will notice an enlargement of the lymph nodes. During the period of 2-4 days of illness, individual or grouped rashes appear in the mouth and face. At first the bubbles are transparent, then become cloudy. When ulcers are damaged, erosions of the skin are formed. Erosion ulcers are painful and cause severe discomfort, causing swelling of the mouth and a coated tongue. Saliva is viscous with an unpleasant odor.
Intoxication of the body increases. Most children develop deep ulcers. The disease, depending on the severity, can last up to 15 days. Erosion ulcers heal without scarring. Relapse of the disease does not recur if there is a stable immune system.
Severe form (Pospischilla aphtoid)
It is observed in children with weakened immunity, depleted by viral infections. Erosion ulcers affect not only the mouth and facial skin, but also the skin of the hands and genitals.
Kinds
Depending on the virus that got inside, the disease manifests itself in several forms, each of which has its own characteristics in clinical manifestation.
Ulcerative-necrotizing gingivostomatitis
This type of disease is called Vincent gingivostomatitis, which can manifest itself in an acute or chronic form. The pathology clinic depends on the severity and localization of the process.
The disease most often affects young men from 17–18 to 30–35 years old. This disease is rare in children and older people. In its development, Vincent's ulcerative - necrotizing gingivostomatitis can occur in mild, moderate and severe forms.
At the initial stage of the disease, the following symptoms appear:
- symptoms of intoxication: malaise, weakness, headache, joint pain;
- discomfort in the oral cavity;
- bleeding gums;
- enlargement and pain of regional lymph nodes.
This condition may last for several days. As ulcerative-necrotizing gingivostomatitis progresses, the symptoms of intoxication worsen. There is an increase in weakness, fever up to 39 degrees, the patient becomes unable to work. The pain syndrome increases sharply. The feeding process becomes extremely difficult.
Against this background, focal symptoms appear and develop:
- severe swelling of the gum tissue;
- hyperemia and severe pain at the slightest physical impact on the oral cavity;
- bleeding gums;
- the appearance of necrotic masses of interdental papillae with the subsequent spread of the process to the entire gum.
The progression of gingivostomatitis provokes the formation of necrotic masses that cover the gums in the form of a gray-brown coating. Against this background, there is a sharp increase in salivation and the appearance of a putrid odor from the mouth.
If inflammation and ulcers in the mouth appear in the area of the wisdom tooth, trismus develops, that is, a sharp limitation in the ability to open the mouth. The ulcerative process can be localized not only on the gums, but also on the cheeks . It can spread deep into bone and muscle tissue, which is often complicated by osteomyelitis of the jaw.
If gingivostomatitis occurs in a mild form, then the patient’s general condition practically does not suffer and the ability to work is preserved. Often the necrotic process affects only the tops of the papillae between the teeth, and the disease is localized.
Herpetic gingivostomatitis
The herpes simplex virus, penetrating into the mucous membrane, causes herpetic gingivostomatitis, which manifests itself in the form of an acute primary infection and a chronic recurrent form. Characteristic manifestations of aphthous gingivostomatitis are:
- The appearance of aphthae against the background of an inflammatory process of the mucous membrane, which has a surface epithelial defect up to 0.5 mm in size. The formation is covered with a white fibrinous effusion and surrounded by a bright red rim.
- Enlarged submandibular lymph nodes;
- Swelling of tissues.
- Fever.
- Bleeding gums.
- Hyperfunction of the salivary glands.
Against the background of pronounced hyperemia of the mucous membrane and an increase in temperature, a massive eruption of elements in the oral cavity occurs, numbering up to 25 pieces. Upon recovery, the manifestations of viral gingivostomatitis are stopped, that is, aphthae regress, and the oral mucosa is cleared.
Treatment methods for different forms of the disease
When you first identify symptoms of herpetic gingivitis or stomatitis, you should seek help from a qualified specialist: an infectious disease specialist and a dentist. The doctor diagnoses the disease through a survey and visual examination of the patient. Assess the nature of the rash and prescribe treatment.
Therapy is reduced to the use of the following medications:
- antipyretic and painkillers;
- antiseptics;
- antiviral ointments and gels;
- decoctions of medicinal herbs for treating wounds.
At the moment of extinction of the disease, it is recommended to regularly treat the ulcers with an antiseptic solution, then with an oil solution (vitamin A). Be sure to adhere to proper nutrition, feed the patient soft foods, and give plenty of fluids. The sick person should be restricted from visiting institutions and crowded places due to the contagiousness of the disease. Those caring for the patient should follow basic hygiene rules.
Treatment for mild forms
To stop the process of inflammation in the body, antiviral drugs are prescribed at the initial stage of the disease, namely:
- tablets Acyclovir, Zovirax, Biocyclovir, Acik, Gerpevir are prescribed in the first week of illness, 1 piece each. 5 times a day for 5 days;
- drugs Interferon, Acyclovir, Acyclostad in the form of applications of solutions, creams or ointments for 20 minutes 5-7 times a day.
Traditional medicine methods can also be used in parallel with drug treatment. Folk remedies provide a mild effect in the form of preparing decoctions and infusions of medicinal herbs (yarrow, sage, St. John's wort, chamomile and calendula).
The method for preparing a decoction of the above herbs is 1 tablespoon of dry herbs per glass of boiling water. Pour and cover the container with a towel for 10 minutes, then strain. Rinse your mouth before and after meals.
The following folk methods are also used to help with mild forms of the disease:
- propolis infusion to relieve pain in the mouth;
- lemon juice for swelling of the mucous membrane;
- flaxseed or sea buckthorn oil at the stage of ulcer healing.
Treatment for moderate severity of the disease
There is general and local therapy to eliminate the moderate form of the disease. General therapy is aimed at preventing the spread of the virus and improving the general immunity of the patient. The following drugs are prescribed:
- painkillers and antipyretics: Paracetamol for children, Efferalgan, Nurofen, Tylenol;
- antiviral drugs: Acyclovir, Zovirax, Biocyclovir, Virolex, Herperax;
- antihistamines: Claritin, Tavegil, Suprastin, Fenkorol;
- vitamins: Ascorbic acid and Ascorutin;
- immunomodulators: IRS-19, Viferon, Anaferon, Arbidol, Imudon;
- drink plenty of fluids and eat a healthy diet;
Local therapy is aimed at reducing pain and healing of erosive ulcers. The most commonly prescribed topical medications are:
- antiseptics: weak solutions of Furacilin, Miramistin after each meal;
- antiviral and healing ointments and oils: Interferon, Acyclovir, Acyclostad, Socloseryl, Carotolin, oil solution of vitamin A, rosehip and sea buckthorn oils;
- painkillers in the form of lotions and ointments: solution of Lidocaine and Pyromecaine, Cholisal, Mundizal-gel;
- alcohol solution of brilliant green, Fukortsin (“red brilliant green”), hydrogen peroxide for treating ulcers on the skin of the face and hands.
Treatment of a serious illness
In case of severe disease, antibacterial drugs (broad-spectrum antibiotics) are prescribed as the main method of treatment to prevent further development of the disease.
Methods of treating patients
The doctor must pay attention to every symptom. Treatment of herpetic gingivitis can be local or systemic. In the first case, various ointments, antiseptics, antiviral solutions and herbal decoctions are used, which are applied directly to the gums. For severe inflammation, proteolytic enzymes are included in the treatment regimen.
Miramistin and Chlorhexidine can be used to treat gums. Chamomile and sage decoctions have an anti-inflammatory effect. When ulcerative defects form, healing agents (Solcoseryl, sea buckthorn and rose hip oil) help. Plant-based preparations are widely used to treat gingivitis. These include Stomatofit. It contains arnica herb, calamus rhizome, oak bark, mint leaves, chamomile flowers, thyme and sage. When treating gum herpes, systemic antihistamines (Clemastine and Fenkarol) are often used. To increase immunity for colds and chronic gingivitis, thymus preparations or gamma globulin are prescribed.
When treating gingivitis, the dentist may prescribe a gentle diet. Spicy foods, spices, as well as foods that can injure the gums - nuts, seeds, raw vegetables, hard fruits - are excluded.
If the condition is satisfactory, treatment can be done at home. To suppress the herpes simplex virus, systemic antiviral drugs (Acyclovir, Acigerpin, Medovir, Valtrex, Valvir, Herperax and Famvir) are prescribed. The use of interferon inducers is effective.
For the speedy healing of erosions in the gum area, keratoplasty agents are used. For gingivitis in children, physical therapy (UFO) can be performed. With frequent relapses of the disease, antiherpetic vaccination may be required. At high temperatures, patients are prescribed antipyretic medications.
After eliminating the main symptoms, treatment of diseased teeth is carried out. The use of mouth rinses is recommended. In the acute phase, you need to avoid spicy and hot foods and drinks. If your gums are bleeding, use soft toothbrushes. Balms and strengthening pastes are used.
You need to brush your teeth after every meal and rinse your mouth. Maintaining good hygiene will speed up your recovery. In case of chronic herpes of the gums with frequent relapses, it is necessary to increase immunity. Thus, gingivitis is a common pathology. It often develops against the background of a herpetic infection.
Tweet
Pin It
- How to quickly cure herpes on the lips
- How does herpes in a child’s throat manifest and be treated?
- How to effectively treat herpes on the lips
- Are antibiotics used for herpes on the lips?
What consequences and complications can there be?
It is important to remember that gingivostomatitis is the most popular form of the disease, caused by staphylococci, streptococci and diplococci. Most often, the disease is observed in children's educational institutions. Inappropriate and untimely treatment leads to tooth loss.
If recovery is not complete, the disease may become chronic. The danger of the disease is that inflammation slowly affects the deep tissue layers, resulting in an increased likelihood of developing periodontal disease, the manifestations of which can be seen in the photo on the left. In this case, partial damage or complete destruction of the ligamentous dental apparatus occurs.
Delaying treatment can lead to more serious viral infections such as diphtheria, measles and influenza. Failure to comply with hygiene and safety rules in the event of illness can reach epidemic proportions.
general information
HERPETIC STOMATITIS IN CHILDREN
Herpetic stomatitis is an acute contagious infectious disease caused by the herpes simplex virus, occurring with symptoms of general toxicosis of the body and local lesions of the oral mucosa [1,2,5,6].
| GP – general practitioner HSV – (genome) of the herpes simplex virus HSV – herpes simplex virus ELISA – enzyme immunoassay ICD – international classification of diseases CBC – complete blood count OAM – general urine test PCR – polymerase chain reaction OB – oral mucosa ESR – erythrocyte sedimentation rate Ig M – class M immunoglobulins |
Users of the protocol: pediatricians, general practitioners, pediatric dentists, pediatric infectious disease specialists.
Assessment of the degree of evidence of the recommendations given [7]
Level of evidence scale:
| A | A high-quality meta-analysis, systematic review of RCTs, or large RCTs with a very low probability (++) of bias, the results of which can be generalized to an appropriate population. |
| IN | High-quality (++) systematic review of cohort or case-control studies or High-quality (++) cohort or case-control studies with very low risk of bias or RCTs with low (+) risk of bias, the results of which can be generalized to an appropriate population . |
| WITH | Cohort or case-control study or controlled trial without randomization with low risk of bias (+). |
Results that can be generalized to the relevant population or RCTs with very low or low risk of bias (++ or +) whose results cannot be directly generalized to the relevant population.
Features of treatment during pregnancy
During pregnancy, most medications are prohibited for use. When symptoms of herpetic pharyngitis appear, interferons are prescribed. Sometimes medications of this series are taken even before the causative agent of the disease is identified. Due to the fact that the herpes virus can cause severe consequences for the development of the unborn child, the doctor must quickly determine the history of the pathology. To do this, a pregnant girl is sent for an ELISA test in order to determine the timing of the entry of infectious agents into the body.
Elimination of herpetic pharyngitis in pregnant women and during lactation should consist of treating the throat with healing solutions, drinking plenty of fluids and taking vitamin complexes. Inhalation of the pharynx with alkaline liquids is also indicated. If the pathology is severe, the woman is admitted to the hospital.
An important point is not only the timely elimination of the symptoms of the disease, but also the prevention of its development.
- To do this, you need to strengthen the body's protective properties and take immunomodulators.
- It is worth observing hand, oral and body hygiene.
- Avoid contact with carriers of pathogenic microorganisms and herpes.
If all the rules are followed, a stronger body will cope with the viruses that have entered it on its own and will not allow the disease to develop.
Features of treatment during pregnancy.