Internal staining of teeth is often due to several main reasons - the death of the pulp and the diffusion of hemoglobin breakdown products into the thickness of the dentin (such teeth have a grayish-black color) and an iatrogenic factor - the consequences of endodontic dental treatment (coloring is due to the diffusion of the constituent components of the sealer - eugenol, iodoform, oxidation products resorcinol).
Unlike external, superficial staining of teeth, this type of staining is very resistant to mechanical cleaning agents (abrasive polishing pastes, ultrasonic scaling, AirFlow), with great difficulty and is not always eliminated by methods of professional teeth whitening with peroxide compounds Professional whitening, pros and cons bleaching.
Internal staining of teeth caused by nutritional factors.
- Abuse of strong tea and smoking, especially in the presence of tooth abrasion, causes persistent and irreversible staining of dentin with tobacco resins and pigments (tannin) of tea.
- Tooth trauma accompanied by damage to the pulp vessels. Over time, hemoglobin in the blood stains the dentin of the tooth in a gray-blue color.
- A chronic inflammatory process in the pulp, pulp necrosis will lead to a change in the color of the tooth to a gray-brown-black color, the internal structure of the tooth - dentin - is stained. Removable so-called internal tooth whitening, performed only in a clinic setting.
- Taking tetracycline drugs in childhood, during the formation and growth of permanent teeth, causes a characteristic “tetracycline” staining of both dentin and tooth enamel in a greenish-yellow color. Removable by chemical bleaching methods, professional “office” bleaching with peroxide compounds, supported and supplemented by mandatory “home” bleaching with lower concentrations of peroxide compounds.
Gallery, teeth discolored after endodontic treatment.
The result of staining is inadequate endodontic treatment when using materials with iodoform as a sealer (root filling).
The photo gallery below shows the stages of whitening previously treated teeth step by step.
Methods of teeth whitening, when, how is it done and is it necessary to whiten teeth?
If a tooth becomes stained after treatment, what should you do?
I immediately warn “experimenters, fans of home whitening and self-taught chemists” - if your teeth have changed color after dental treatment (not for the better) - contact a dental clinic for a consultation with a qualified certified specialist, a dentist.
It is dentists (and not Internet Answers MailRu and the almighty Yandex + Google) who will help you determine what happened to the color of your teeth, the reasons for the color change and methods of correction. Don’t rush to whiten your teeth using “folk methods proven by thousands of years of experience.”
Do not pour “White”, “Parus” or “Vanish” into your mouth, do not smear your teeth with advertised SUPER-WHITENS. This will bring you nothing but severe chemical burns and disappointment.
External staining of teeth can be eliminated by professional hygiene - cleaning with ultrasonic scalers, soda blasting, polishing with special abrasive pastes.
Alternatively, discolored teeth can be restored using:
- production of direct veneer from composite material,
- production of a metal-ceramic crown (especially important if the tooth consists of 50% or more restorations),
- production of metal-free ceramics,
- production of ceramic veneer.
Teeth whitening. A marketing slogan that has sunk into the weary consciousness of the consumer: “What else could I do with myself to get people to pay attention to me?”
Teeth whitening is one of the fashionable trends of modern life. Snow-white teeth and a shining white smile are associated with success, projected as the image of a business person, white teeth guaranteed by advertising anticipate the ascent to the Olympus of fame.
Attention! Professional oral hygiene is necessary before any teeth whitening procedure , whether you are planning home or office whitening, carried out independently or under the supervision of a specialist. It is impossible for a concentrated solution of hydrogen peroxide to penetrate the layer of plaque or tartar on the surface of the teeth, so whitening may proceed unevenly and the resulting result on the surface of the tooth will create “leopard spotting”, which is very unsightly in appearance and is ambiguously perceived by others.:down:
Facts: a high concentration of hydrogen peroxide in a whitening gel destroys gums and tooth enamel; a low concentration does not give a noticeable and quick result. The use of “whitening” chewing gum, pencil brushes, and Velcro patches is a waste of your time and money.
Teeth can be whitened only with aggressive means; most whitening compositions contain peroxide compounds - hydrogen peroxide or urea in high concentration!
Attention! You cannot whiten your teeth once and for all. Over time, teeth change color again. To ensure long-lasting teeth whitening results, it is recommended to avoid coffee, tea, red wine and other coloring drinks. Smoking also affects tooth discoloration. Proper oral hygiene and a “white diet” - (nothing colored!) will prolong the effect of teeth whitening.
You can't whiten your teeth:
- If teeth are damaged by caries.
- If the teeth are not sealed tightly or there is a violation of the marginal seal of old fillings.
- If the teeth are filled in the aesthetic zone (the color of the fillings and the color of the whitened teeth will differ, so it is recommended to carry out teeth whitening before aesthetic filling and restorations).
- If you have periodontal disease (in 75-80 adults).
- During pregnancy and lactation, any bleaching is contraindicated.
- If your teeth or necks of your teeth are sensitive before bleaching, after bleaching your teeth will definitely have severe sensitivity to both temperature and chemical irritants.
Expert advice: Teeth whitening should be done in moderation. Teeth appear naturally white if their color matches the color of the white of the eyeball, the sclera. Cosmetologists warn that at an older age, teeth that are too white age you and look unnatural and unnatural.
- Teeth that have changed color as a result of endodontic treatment are NOT subject to external bleaching.
- It is impossible to “whiten” teeth covered with ceramic or plastic crowns with whitening gels; they can be visually made lighter by mechanical means, cleaning with abrasive pastes, or a soda jet.
- Composite restorations cannot be bleached; the discoloration of the composite is irreversible and the restoration must be replaced.
Installation of artificial crowns
The pin is installed in the root canal of the tooth, filled with gutta-percha, at the end of endodontic treatment. To do this, part of the gutta-percha is removed, a pin is inserted into the canal and fixed with cement. The top of the tooth is covered with filling material in order to restore its anatomical shape. If necessary, an artificial crown is placed on the tooth.
Installation of root pins and pin inlays is an important stage in tooth restoration using fixed dentures.
If the crown part of a tooth is completely destroyed, it is restored using standard pins, cast core inlays, standard pins made of carbon fibers, and other structures.
After the post is placed, a dental crown is placed on the top of the tooth. The purpose of dental crowns is to hide tooth defects located above the gum. Thanks to dental crowns, you can not only restore the natural shape of the tooth, but also improve it, giving it the most natural appearance.
To make an appointment for dental restoration after endodontic treatment, write to us on the website of the Stompraktika.rf clinic or call 731-11-11.
We are always glad to see you!
March 15, 2016
This site is for informational purposes only and is intended for educational purposes; site visitors should not use the materials posted on the site as medical advice.
Darkening of the tooth after endodontic treatment.
Teeth staining, internal whitening.
The problem of multi-colored, tarnished, discolored teeth after endodontic treatment is relevant for many patients.
From the anamnesis - treatment occurred for complicated caries about 10 years ago, the tooth canal was filled with a sealer based on COE (paste based on zinc oxide and eugenol, containing a hormonal anti-inflammatory component. Material for filling root canals - "Endomethasone", Septodont/France.
Over time, the material (like most COE sealers) undergoes resorption and decay, the derivatives of Endomethasone and eugenol oxidize, decompose, and the diffusion of components (diiodothymol) stains the tooth tissue (dentin) in a persistent orange-brown color.
Regarding the question: should endomethasone be used in modern practice or not?
If the above facts and macro photographs of teeth stained with endomethasone do not convince you of anything... Here Endomethasone is praised, I pulled out a special footnote, I will highlight the necessary one in purple.
The method of its use for temporary filling of canals is quite acceptable: the seal can be checked, anti-inflammatory therapy can be carried out, and upon positive dynamics, repeated treatment can be carried out, the contents of the canal can be easily removed and sealed in accordance with the indications for subsequent restoration.
IMHO. For fans of Endomethasone supporters.
About the magical properties of hormonal drugs in dentistry and endodontics. Lack of manual skills in endodontic treatment, negligence in work, incomplete evacuation of putrid and pulp residues from the root canal system, insufficient disinfection of the root canal (failure to comply with the endodontic intervention protocol, no matter how sad it may sound) on the one hand, and the presence of pronounced antiseptic and anti-inflammatory properties of the drug, on the other hand, will provide a temporary (I focus your attention on the word “temporarily”) effect of the supposedly successful treatment.
Why temporary? I argue with facts.
- the remains of the pulp, putrid, microbial association (fungi, anaerobes, spores and aerobic forms) in the lumen of the canal and in the microtubule system have not disappeared ANYWHERE. Fact? Fact.
- the hormonal component of the temporary root sealer inhibits the phagocytic reaction of the body and indirectly stimulates the vital activity of microorganisms, especially mycete fungi,
- humidity, constant temperature, the presence of a nutrient medium and microbial alliance, the absence of a protective phagocytic reaction of the macroorganism, suppressed by a hormonal component provokes destructive processes in the periodontium caused by microbial toxins
- leaching of the components of the drug and a decrease in its magical and unique antiseptic and other beneficial properties of “Endomethasone”
- staining of tooth dentin with decay products of the microbial-putrid complex and the components of the drug (I’m more guilty of diiodothymol, the specific coloring of “endometazonized” teeth is caused, it seems, by them)
- the formation of a granuloma (in the case of a chronic course of the process) or an exacerbation with periostitis (a great variety of reasons that doctors know about).
Treatment plan and stages.
- Endoretriment - retreatment of root canals. Removal of COE-sealer residues, therapy of periapical changes in the periodontium (toxic damage to the ligamentous apparatus)
- Thorough multiple and multi-stage disinfection of the root canal with halogen-containing antiseptic solutions, read - Irrigation and antiseptics of the root canal
- Adequate filling of the root canal with gutta-percha and sealer based on epoxy resins, advantages of epoxy sealers.
- After complete polymerization of the root filling (sealer and gutta-percha into a single block), removal of the long-term filling, cleaning the coronal part of the tooth from traces of sealer
- Etching with polyacrylic acid to open the dentinal tubules and improve the effect of peroxide compounds in the bleaching composition, sealing the mouth of the root canal with a light-curing liquid composite (to eliminate the effect of peroxide compounds on the tooth root).
- Introduction of a whitening composition into the coronal part of the tooth, sealed long-term filling made of light-curing composite material, exposure 5-7 days
- If necessary, the intracoronal bleaching procedure is repeated until the desired result is achieved.
- After 14-15 days, the temporary filling is removed, the coronal part of the tooth is freed from the bleaching composition, thoroughly washed with sodium hypochlorite to neutralize traces of peroxide compounds, if possible, the coronal part is filled with calcium hydroxide paste and closed for at least 7-10 days with a temporary filling.
- Removal of a temporary filling, cleaning the coronal part of the tooth from traces of calcium hydroxide using organic acids (citric, polyacrylic) and activation with an ultrasonic endochak, adhesive preparation, filling the coronal part of the tooth with a composite material, grinding the filling, polishing, insulating with varnish.
Therapeutic (composite) restoration of the color of stained teeth.
Case No. 1.
A 56-year-old patient is dissatisfied with his dark and ugly teeth. An example of tooth staining due to chronic abfraction and removal of staining by professional cleaning followed by the production of direct composite veneers, Charisma Opal composite (Heraeus Kulzer).
Staining of dentin exposed as a result of abfraction of the anterior teeth with alimentary (food) pigments and combustion products of tobacco.
Errors and complications during endodontic treatment
Errors and complications of endodontic treatment can be divided into two groups: diagnostic errors and errors during the treatment process [KodukovaA.
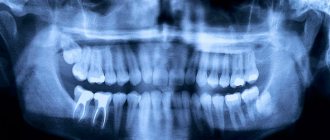
et al., 1989]. Diagnostic errors. Often occur in the presence of facial pain, which often radiates to a particular tooth. Many doctors encounter in their practice cases of neuralgia II, 111 branches of the trigeminal nerve with extracted teeth. With stomalgia (glossalgia), the patient often points to the “causative” tooth, demanding its treatment or removal. In such cases, the main criterion for the need to remove the pulp or tooth is a thorough clinical examination using odontometry. On the other hand, the presence of an undetected tooth with an inflamed pulp (usually a molar, less often a premolar) is diagnosed as neuralgia of the II or III branches of the trigeminal nerve. It should become a rule that in case of suspected neuritis, neuralgia, stomalgia, it is necessary to completely exclude the possibility of inflammation of the pulp or periodontium.
The second group of diagnostic errors is associated with the interpretation of radiographs in the upper jaw, when the contours of the maxillary sinus (Fig. 9-1) and the incisive foramen are superimposed on the root apex. The preservation of the continuity of the periodontal fissure against the background of the maxillary sinus indicates that this tooth is not the cause of destructive changes in bone tissue. In the lower jaw, the mental foramen is sometimes mistaken for destructive changes in bone tissue. In such cases, careful evaluation of the radiograph is required (Figs. 9-2, 9-3). The presence of continuity of the periodontal fissure at the apex of the root of the “suspected” tooth indicates that it is not involved in the focus of this change. However, the decisive factors are the determination of the condition of the pulp - “electroodontodiagnosis”, as well as an attempt to prepare the tooth, especially in the presence of a carious cavity or filling, without anesthesia. The presence of pain during preparation indicates the normal condition of the pulp.
Rice. 9-1. Preservation of continuity of the periodontal fissure of the second molar and first premolar against the background of the maxillary sinus. X-ray.
Rice. 9-2. The mental foramen is projected onto the apex of the root of the first premolar. X-ray.
Rice. 9-3. Projection of the mental foramen onto the apex of the second premolar of the mandible. The crown of the tooth is without carious damage. The continuity of the periodontal fissure is not broken. X-ray.
Errors and complications during endodontic treatment
Errors and complications of endodontic treatment can be divided into two groups: diagnostic errors and errors during the treatment process [KodukovaA. et al., 1989].
Diagnostic errors. Often occur in the presence of facial pain, which often radiates to a particular tooth. Many doctors encounter in their practice cases of neuralgia II, 111 branches of the trigeminal nerve with extracted teeth. With stomalgia (glossalgia), the patient often points to the “causative” tooth, demanding its treatment or removal. In such cases, the main criterion for the need to remove the pulp or tooth is a thorough clinical examination using odontometry. On the other hand, the presence of an undetected tooth with an inflamed pulp (usually a molar, less often a premolar) is diagnosed as neuralgia of the II or III branches of the trigeminal nerve. It should become a rule that in case of suspected neuritis, neuralgia, stomalgia, it is necessary to completely exclude the possibility of inflammation of the pulp or periodontium.
The second group of diagnostic errors is associated with the interpretation of radiographs in the upper jaw, when the contours of the maxillary sinus (Fig. 9-1) and the incisive foramen are superimposed on the root apex. The preservation of the continuity of the periodontal fissure against the background of the maxillary sinus indicates that this tooth is not the cause of destructive changes in bone tissue. In the lower jaw, the mental foramen is sometimes mistaken for destructive changes in bone tissue. In such cases, careful evaluation of the radiograph is required (Figs. 9-2, 9-3). The presence of continuity of the periodontal fissure at the apex of the root of the “suspected” tooth indicates that it is not involved in the focus of this change. However, the decisive factors are the determination of the condition of the pulp - “electroodontodiagnosis”, as well as an attempt to prepare the tooth, especially in the presence of a carious cavity or filling, without anesthesia. The presence of pain during preparation indicates the normal condition of the pulp.
Rice. 9-1. Preservation of continuity of the periodontal fissure of the second molar and first premolar against the background of the maxillary sinus. X-ray.
Rice. 9-2. The mental foramen is projected onto the apex of the root of the first premolar. X-ray.
Rice. 9-3. Projection of the mental foramen onto the apex of the second premolar of the mandible. The crown of the tooth is without carious damage. The continuity of the periodontal fissure is not broken. X-ray.
A special approach is required in the first days after a tooth injury. If there is a fracture of the crown exposing the pulp or a horizontal fracture of the root at any level, then the pulp is removed under anesthesia. Removal of the pulp is also necessary in case of rupture of the vascular bundle, which is determined by a change in the color of the crown, it becomes pink. If there is no confidence in the rupture of the vascular bundle, although there is pain and percussion is painful, then you should wait 3-4 days. Then it is necessary to determine the condition of the pulp. Then they decide whether to save or delete it. If there is no sensitivity of the pulp, then trepanation is performed to remove the necrotic pulp and subsequent endodontic treatment. It is important to remove it in the days following the injury to avoid the possibility of dentin staining. It should be remembered that in case of a horizontal fracture, the tooth can be saved. To do this, it is necessary to remove the pulp from the root canal along its entire length and prepare a pin for immobilizing root fragments. Currently, thermofil with a titanium or stainless steel carrier is used for this purpose. Medicinal treatment of root canals is performed with calcium hydroxide preparations. We used Biocalex for this. Its liquid consistency ensures penetration into the gap between fragments (Fig. 9-4).
Rice. 9-4. Horizontal subgingival fracture at the level of the tooth neck. X-ray: a - a verifier is inserted into the root canal over the entire working length; b — filling the root canal with thermophile.
Rice. 9-5. Perforation of the bottom of the lower molar cavity and introduction of filling material to the depth of the root length. X-ray.
A tooth may be slightly dislocated. In such cases, it is important to determine the condition of the pulp and make a decision based on this. In case of injury accompanied by tooth loss (as a rule, these are incisors), the tooth is trepanned through the crown, the pulp is removed, the canal is processed and filled using the generally accepted method. Then, under anesthesia, the tooth socket is treated, washed with antiseptic solutions, and a tooth with an obturated canal is inserted into it. The final stage is splinting the tooth, which is not difficult if composites are available. As a rule, the clinical course is calm and the tooth functions normally. X-ray control is carried out after 3, 6, 12 months. On the other hand, as a rule, an unfavorable outcome is observed when the dislocated teeth are well fixed in the socket, but the tooth pulp is not removed. In all observed cases, there was inflammation with destruction of bone tissue and tooth rejection. Errors in the treatment process.
1. Perforation of the walls and bottom of the tooth cavity.
1.1. Perforation of the bottom of the tooth cavity as a result of poor orientation and visibility. Most often, this is observed when the canopies over the tooth cavity are insufficiently removed (Fig. 9-5).
1.2. Perforation at the level of the tooth neck (sub- or supragingival), which is also observed with poor visibility, as well as as a result of preparation without taking into account the position of the tooth (Fig. 9-6, 9-7).
Rice. 9-6. Cervical perforation of the crown of a mandibular molar as a result of preparation without taking into account the inclination of the tooth. X-ray.
Rice. 9-7. Perforation of the medial root of the mandibular molar and introduction of filling material into the mandibular canal. The preparation was carried out without taking into account the inclination of the tooth. X-ray.
It should be noted that diagnosing perforation is not very difficult. The appearance of profuse bleeding in combination with greater or lesser pain clearly indicates the creation of perforation. In this case, it is necessary to perform x-ray control. In this case, it is advisable to introduce radiopaque material into the suspected perforation hole. The most suitable material is a gutta-percha point. In most cases, the doctor does not consider it necessary to inform the patient about this and make an appropriate entry in the medical history, which is also a mistake.
2. Perforation of the root canal. According to some data, it occurs in up to 9% of all errors. The reasons for this may be as follows.
2.1. Insufficient opening of the tooth cavity or an attempt to prepare a root canal without providing direct access to the endodontic instrument into the canal.
2.2. Wrong choice of endodontic instruments. When expanding curved canals, it is advisable to use instruments with a blunt tip made of nickel-titanium alloy (profiles), which are highly flexible (Fig. 9-8).
Rice. 9-8. Perforation of the medial root resulting from the use of a non-flexible file with an active (sharp) tip. X-ray.
3. Fracture of the endodontic instrument in the root canal (Fig. 9-9).
Rice. 9-9. Fracture of the canal filler in the root canal (a) (the file managed to bypass the fracture of the instrument) and fracture of the instrument in the second premolar (b). Radiographs.
3.1. Lack of direct access to the root canal.
3.2. Violation of the sequence of use of endodontic instruments.
3.3. Lack or insufficient control over the condition of endodontic instruments. At the first sign of a change in the structure of the coils (unwinding or twisting), the tool must be replaced.
3.4. Applying significant force to the tool during manual or machine processing.
3.5. Violation of technology for using the tool. Inserting a tool to a significant depth while rotating the tool several revolutions often leads to jamming and then breakage of the tool. The tool should rotate no more than 120-180 degrees.
3.6. Attempting to enlarge the root canal with a non-endodontic handpiece. When rotating only clockwise, deep penetration into the root canal occurs and, as a result, breakage occurs.
3.7. Working in a dry canal.
3.8. Haste in work.