Detection of the immunodeficiency virus is an important task of modern medicine
HIV is a common disease. Every year in Russia the number of infected people is growing. Every day in Russia 80 people with HIV die (HIV in numbers). More than half of all cases of infection were recorded in 13 constituent entities of the Russian Federation, Rosstat, p.228.
In most cases, the disease is transmitted sexually, through unsterile medical instruments (for example, through intravenous drug administration with a shared syringe), and it is impossible to vaccinate against it or develop immunity. These facts determine the virtual defenselessness of every person against the immunodeficiency virus.
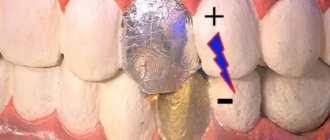
Timely initiation of antiviral therapy and constant monitoring make it possible to extend a person’s life to 70-80 years. The sooner treatment is started, the more favorable the prognosis will be. Manifestations of HIV infection in the oral cavity appear in the early stages. At the same time, the oral cavity is easily accessible for examination (unlike the lungs and stomach), which makes it possible to detect suspicious symptoms in a timely manner. Therefore, it is extremely important for every person to have at least a minimal understanding of the symptoms of HIV infection in the oral cavity.
Symptoms of HIV in the mouth with photos
There is a conditional gradation of HIV symptoms in the oral cavity, depending on the degree of their relationship:
In HIV patients, the painful condition of the oral cavity is chronic with periodic exacerbations, relapses and remissions. Gradually, the situation worsens, clinical symptoms intensify, and periods of rest are practically absent. The mucous membrane suffers even from minor pathogens, which the immune system of healthy people immediately rejects.
In medical photographs, characteristic symptoms can be seen very clearly:
Provoking factors - why infection occurs
The immunodeficiency virus enters the body through microtrauma to the mucous membrane during unprotected sexual intercourse, or into the bloodstream when the integrity of the skin is violated with a non-sterile syringe. Virions are delivered through the bloodstream to the lymph nodes, where they are integrated into the RNA of immune cells - lymphocytes. Reproduction of the virus inside the cell blocks its ability to protect the body from foreign agents, which leads to multiple diseases of the organs and systems of the infected person.
The virus gradually reduces the ability of the mucous membrane in the mouth to resist fungi and bacteria. The possibility of destruction of atypical malignant cells by lymphocytes of the dentofacial area is also blocked. HIV-associated lesions in the mouth arise as a result of failure of the general immune system.
Complex clinical picture
The presence of an infection in the mouth of any location (stomatitis, cheilitis, glossitis, gingivitis), which is difficult to treat, is an alarming sign and may be a manifestation of HIV. This is a signal that the immune system cannot cope with the infection and the person may be a carrier of immunodeficiency viruses.
You should suspect something is wrong if the listed diseases are protracted and cannot be treated with antibacterial and antifungal medications.
General view of the oral cavity
HIV and AIDS are characterized by various inflammatory reactions in the oral cavity - erosions, ulcers, blisters, which often occur in the mouth and are poorly treated with standard medications. There is often severe odor from the mouth due to the addition of a secondary bacterial infection.
Appearance of the tongue in HIV
The tongue is covered with a white coating, densely populated by a colony of fungi of the genus Candida. It does not clean off on its own; after removal with instruments, a reddened and bleeding mucous membrane is revealed underneath.
The lateral surfaces are affected by leukoplakia. It forms growths of the epithelial layer that look like whitish or light yellow thin villi.
In the photo, the main symptoms on the tongue for HIV are candidiasis, leukoplakia:
Throat view
The mucous membrane of the throat with HIV is hyperemic, covered with erosions and white ulcers, 3-5 mm in diameter. Sometimes abscesses appear on it, which look like yellow blisters with thick contents.
Cheek view
On the mucous membrane of the cheeks in the area where the teeth meet, areas of compaction of the epithelial layer form in the form of a white film. Hemorrhages are observed in the submucosal tissues - multiple red dots with a diameter of 1-2 mm.
Type of gums
Gingival papillae are deformed due to ulcerative necrotizing gingivitis. The mucous membrane is covered with a dense white coating that emits an unpleasant odor.
However, the immunodeficiency virus affects the entire body, and not local organs. Therefore, in order to suspect a diagnosis of HIV, it is necessary to pay attention to the following accompanying symptoms:
- sudden unexplained weight loss;
- fever lasting longer than 1-1.5 months, for no apparent reason;
- simultaneous enlargement of lymph nodes in different parts of the body (cervical, axillary, inguinal).
Therefore, all manifestations of HIV in the oral cavity are accompanied by symptoms of general damage to the body.
Classification of common lesions
All diseases that occur in the oral cavity due to HIV can be divided into 2 large groups.
Lesions that almost always occur during the development of infection:
- Kaposi's sarcoma is a malignant tumor that looks like purple or dark blue protruding spots on the mucous membrane, with a diameter of 1 to 4 cm, the surface is uneven, lumpy;
- Non-Hodgkin's lymphoma is a malignant tumor of the dentofacial area, accompanied by enlarged lymph nodes, destruction of bone tissue around the teeth, bulging and redness of the mucous membrane in the affected area;
- hairy leukoplakia – forms on the tongue (on the lateral surface), has the appearance of white villi;
- candidiasis is a fungal infection, manifested by hyperemia of the mucous membrane and abundant white or yellow plaque that does not come off on its own;
- ulcerative-necrotizing gingivitis associated with HIV is of a bacterial nature, occurs suddenly, with acute manifestations, after some time the gum tissue dies, forming a defect, and relapses often occur.
In the photo, Kaposi's sarcoma is a common manifestation of AIDS in the oral cavity
. More rare manifestations:
- thrombocytopenic purpura is a disease of the hematopoietic system, manifested by hemorrhages in the mouth, looking like a pinpoint red rash;
- bacterial and viral infections - affect the gums, periodontium, lips, tongue, are resistant to antibiotics and antiviral drugs, and have frequent relapses;
- salivary gland diseases.
In the photo, cheilitis is a common lesion of the lips during the development of HIV infection
HIV infection and candidiasis
Candidiasis is one of the fungal infections caused by a fungus of the genus Candida.
Candidiasis with HIV can be more intense and pose a direct threat to life. This fungus is present in moderate quantities in the microflora of every healthy person. Some people are active carriers of the fungus without experiencing any discomfort. But the pathology in HIV-infected people has obvious manifestations and can cause death.
In a supposedly healthy person, it may be a sign of HIV infection.
Reasons for development
Everyone has a fungus of the genus Candida, but it may not cause diseases or pathologies in a healthy person with sufficient body resistance.
The development can be triggered by a weakening of the body’s protective function (local immunodeficiency) or by the human immunodeficiency virus (HIV).
Therefore, oropharyngeal candidiasis (affects the mucous membrane of the nasopharynx), which manifests itself in the first stages in 90% of HIV-infected people, is considered one of the markers of a fatal disease.
Candida albicans does not only appear in AIDS. Even those strains and manifestations of the fungus that are found in patients with HIV can be signs of hypovitaminosis, dysbacteriosis, or a consequence of taking antibiotics in a person who is not a carrier of HIV infection.
What symptoms are you worried about?
The most common cause of HIV is candidiasis of the oral mucosa.
Most often, Candida affects the mucous membranes of the body - the mouth, genitals, and can also develop in the corners of the mouth, causing angular cheilitis, in the folds of the skin - under the breasts in women, in the axillary and buttock folds, in the perineum and even in the interdigital folds on the hands. More rare is the manifestation of Candida fungus on smooth skin. The symptoms of the disease are shown in the table:
| Type of candidiasis | Characteristic symptoms |
| Oral candidiasis | It appears as a white coating on the tongue, palate and buccal mucosa. Painful sensations when eating, a burning sensation in the mouth are possible. |
| Thrush in women | Regular cheesy discharge, itching, pain during sex, discomfort when urinating, unpleasant odor. |
| Candida cheilitis | Painful cracks (jams) in the corners of the mouth, covered with a whitish coating that can be easily removed. |
| Candidiasis of the folds | It manifests itself as crimson-colored erosions, which may have a bluish tint and peeling of the skin at the edges. |
| Candidiasis of smooth skin | It manifests itself in the same way as candidiasis of the folds and is usually its consequence. |
Feature of the flow
Candidiasis in HIV-infected people often forms in the oral cavity. Later it may manifest as candida cheilitis. In people infected with AIDS, the fungus is prone to rapid development, relapse and the manifestation of obvious symptoms of the disease in a short time.
From the mouth it can very quickly pass into the esophagus and cause digestive problems, even blocking the digestive tract due to swelling of the mucous membrane. Also, patients with AIDS are characterized by atypical forms of the fungus.
For example, folliculitis, which can cause ulcers at the site of the follicles, and later, partial baldness.
Candidiasis in this combination is rarely curable due to weak immunity.
Features of the course in HIV-infected people:
- It appears more often in men with HIV than in women.
- Treatment rarely works.
- Oral candidiasis in HIV occurs in 20% of cases, less often in the genital and perigenital areas.
- Manifestations of cheilitis spread faster and with high intensity.
- HIV-infected people may develop atypical strains of the fungus.
Diagnosis of candidiasis in HIV
If there are obvious symptoms, a series of tests are carried out for the presence of fungi of the genus Candida. First of all, fungi are detected in the blood and urine. This helps determine how much the body is affected by the fungus. A swab of the throat and other affected mucous tissues is also taken. Skin and nail samples may be taken.
Serological reactions in HIV-infected people remain negative, so isolation of the fungus from the spinal cord, intra-articular fluids and blood is of diagnostic importance.
After collecting the material, a culture is performed to determine the type and genus of the fungus, as well as the number of pathogenic microflora microorganisms.
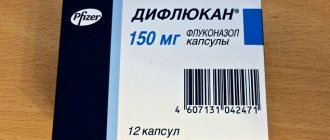
What treatment is indicated?
Typically, epitropic treatment of candidiasis in HIV infection is quite effective. It is very important to eliminate the causes of Candida in the body. It is also necessary to increase the amount of B vitamins. Candidiasis of folds and smooth skin should be treated with antimiotics, which are included in ointments for external use.
Treatment of mucous membranes (thrush) occurs with the help of topical suspensions containing nystatin. You can also treat the fungus with tablets or injections. Depending on the number of colon-forming microorganisms, the doctor can vary the intensity of treatment, up to intravenous injections of Amphotericin.
Therefore, it is very important that the doctor prescribes treatment based on test results.
Source: https://EtoGribok.ru/molochnica/vidy/kandidoz-pri-vich.html
Stages of infection development
HIV occurs in several stages, which manifest themselves in different ways:
- The incubation period begins from the moment the virus enters the blood and lasts up to 6 months. There are no manifestations in the oral cavity.
- The period of acute manifestation of infection is manifested by symptoms of a respiratory disease - increased body temperature, runny nose, sore throat. On the part of the oral cavity - enlargement of the submandibular, sublingual, parotid, peripharyngeal lymph nodes.
- Latent stage – lasts from 5 to 7 years. The oral cavity is affected by viral and bacterial infections, mycoses. The frequency of diseases can be 3-4 times a year.
- Stage of AIDS - specific lesions appear in the mouth: Kaposi's sarcoma, Non-Hodgkin's lymphoma, hairy leukoplakia, persistent mycoses and candidiasis.
In the photo, hairy leukoplakia - often manifests itself on the tongue and mucous membranes with HIV
Stages of HIV infection in the oral cavity
The medical literature identifies several typologies of HIV stages. One of the most understandable and widespread is the classification, which involves 4 stages of disease development, and each of them is accompanied by different manifestations.
Stages of immunodeficiency:
- incubation period
- period of primary manifestations (acute, then asymptomatic infection),
- persistent generalized lymphadenopathy,
- stage of irreversible secondary immunodeficiency.
Diagnosis, examination and differential diagnosis
The only reliable way to diagnose HIV is a blood test. The most widely used method is enzyme-linked immunosorbent assay (ELISA), which shows the presence of HIV antibodies in the blood. If less than 6 months have passed since infection, antibodies to the virus will not have time to develop, and the analysis will show an erroneous negative result.
If a positive result is obtained after ELISA, the second stage of the examination is prescribed - immunoblotting. The principle of its operation is the presence of an electric field, which detects antibody molecules with a guarantee of an accurate result.
Manifestations of HIV in the oral cavity must be differentiated from other bacterial and viral diseases (herpes, tuberculosis, syphilis), from some autoimmune diseases (lichen planus). Laboratory tests are crucial for the final diagnosis.
Candida fungi and human immunodeficiency virus
Candida fungi are a single-celled microorganism that is present in the body of any person. But with a positive HIV status, a laboratory test for the presence of candidiasis may show a negative result. The main sign of the disease is the presence of plaque on the oral mucosa.
Thrush in immunodeficiency is diagnosed much more often, which is due to reduced immunity. That is why pathology is noted already at the initial stages of infection.
Treatment methods
Therapy for HIV infection and its manifestations in the oral cavity should be comprehensive and carried out with the participation of an infectious disease specialist, dentist, and otolaryngologist. If necessary, doctors of other specialties (surgeons, oncologists) should be involved in treatment. It is mandatory to monitor the patient once every 4 months for timely detection of possible complications.
General
Antiviral therapy is prescribed for treatment. Drugs and dosage are selected individually for each patient by the attending infectious disease specialist.
Modern therapy allows a person to live to a ripe old age, provided that they take prescribed medications and undergo periodic blood tests to determine the effectiveness of treatment and viral concentration in the body.
Maintaining a healthy lifestyle is important - quitting smoking, alcohol, drugs, maintaining a daily routine, balancing nutrition, dealing with stress, moderate physical activity, and physical exercise.
Dental care
Dental care for HIV-infected people is provided on an equal basis with other patients in all dental institutions of the Russian Federation. Treatment is divided into 3 groups:
- Etiological – carried out for bacterial and viral infections. Antibiotics and antiviral drugs are selected and prescribed based on the sensitivity of the pathogen to them.
- Preventive – preventing relapse of the disease. Includes filling of carious teeth, removal of dental plaque, and general sanitation.
- Symptomatic – treatment of ulcers and erosions with anesthetics (Lidocaine spray and gel), antiseptics (Chlorhexidine, Furacilin), prescription of healing drugs (Solcoseryl, sea buckthorn oil).
Treatment of dental diseases caused by HIV
The presence of the immunodeficiency virus requires complex treatment that can maintain the necessary vital functions of the body. It is based on taking various antiretroviral medications.
Dental ailments caused by HIV must be treated promptly and thoroughly. Suppressed immunity and internal microflora cannot resist pathogens, so illnesses progress quickly. Therapy includes treatment in the dentist's office and medication (broad-spectrum antibiotics, antiviral, antifungal medications, corticosteroids, etc.).
Dental diseases
Dental clinics provide safe and high-quality treatment. In this case, disposable instruments are used, and reusable ones are carefully sterilized (in the environment the virus dies at temperatures above 60 degrees). Dentists carry out all the necessary manipulations - treat caries, fill teeth, perform prosthetics. However, they approach the issue of surgical intervention very carefully.
Doctors often encounter HIV periodontitis. It has all the signs of ordinary periodontitis (inflammation of periodontal tissues), but is characterized by rapid progression. This means that the patient can very quickly lose teeth. The therapy represents classical measures to combat periodontitis, taking into account the patient’s main course of medication.
Gingivitis
Gingivitis in the mouth is an inflammatory process in the gums. Depending on the form and degree of development, the patient develops various signs, including swelling, redness, itching or burning, bleeding, atrophy or enlargement of the gingival papillae, and the formation of necrotic ulcers.
Gingivitis is treated comprehensively:
- oral sanitation and professional cleaning;
- thorough treatment with antiseptic drugs;
- taking antibiotics or antiviral medications;
- taking antihistamines;
- use of healing gels and ointments.
Candidal stomatitis
Candidiasis (thrush) is observed in more than 90% of infected people. Stomatitis in this case can be atrophic, hypertrophic or pseudomembranous. The latter type of candidal stomatitis occurs most often.
Thrush is characterized by classic symptoms:
For candidiasis, it is recommended to take antifungal drugs that inhibit the Candida fungus, antimycotics, the use of pharmaceutical antiseptics, careful oral hygiene, and diet. For extensive candidiasis lesions, healing agents are used.
Other diseases
Almost all HIV patients experience hairy leukoplakia (Epstein-Barr virus). It appears as a permanent white or gray coating on the tongue. The mucous membrane becomes covered with folds and rough plaques. The occurrence of pathology is provoked by malfunctions of the immune system.
That is why the treatment has an immunomodulatory focus:
- antiretroviral therapy;
- immunotherapeutic treatment;
- antiviral medications;
- antimycotics;
- medicines based on retinoic acid;
- in advanced cases, the affected areas are excised surgically or using a laser.
Pathological changes in the oral cavity observed in patients infected with the immunodeficiency virus. With secondary immunodeficiency, active reproduction of opportunistic and pathogenic flora begins. This leads to the development of infectious-inflammatory, degenerative and oncological processes in the oral cavity: gingivitis, periodontitis, cheilitis, viral and fungal infections, Kaposi's sarcoma, etc. HIV diagnosis is carried out by laboratory methods and is aimed at detecting the virus itself, antibodies to it and assessment of the state of the cellular component of the immune system. Effective treatment has not been developed to date; the basis of therapy is antiretroviral drugs.
If examination reveals a rash with painful pink, purple, red spots or nodules on the mucous membrane of the hard palate, you can think about Kaposi's sarcoma. It is a malignant lymphangioma. Thanks to advances in modern therapy, Kaposi's sarcoma is now much less common in clinical practice. In addition, there are a number of pathological processes in the oral cavity that indicate the presence of the HIV virus (cheilitis, glossitis, ulcers, telangiectasia, etc.), but their prevalence is less great.
Preventive measures
Prevention of HIV infection is the use of personal protective equipment during sexual intercourse, the use of sterile instruments when performing manipulations associated with violating the integrity of the skin and mucous membranes (injections, blood collection and transfusion, dental treatment).
Prevention of possible manifestations of HIV in the oral cavity is a timely visit to the dentist, treatment or removal of teeth as necessary, and hygienic cleaning at the dentist.
HIV and AIDS
>The source of infection is a person with AIDS or a virus carrier - infected with HIV. HIV-infected persons include all those infected with the virus, regardless of their clinical condition, as evidenced by positive serological tests: immunosorbent assay (ELISA), confirmed by immunoblotting (Western blotting), immunofluorescence reaction or radioimmunoassay and virus isolation.
After HIV infection, AIDS develops in 20% of infected individuals within the first 5 years, and in approximately 50% within 10 years.
In people infected with HIV, the pathogen is found in various biological fluids (blood, semen, vaginal secretions, breast milk, saliva, tear fluid, sweat, etc.), but transmission of the infection occurs only through blood, semen, vaginal secretions and breast milk.
There are 3 known ways of transmitting HIV infection: sexual, parenteral and perinatal.
Most often, HIV is transmitted sexually: from an infected person to his sexual partner. Parenterally, the infection is transmitted through the transfusion of infected blood or blood products, as well as through the use of needles, syringes, dental or other instruments to pierce the skin or oral mucosa if these objects are contaminated with blood. Transmission of HIV infection from a woman to her fetus or child can occur in utero, less commonly during childbirth and through breast milk.
HIV can also be isolated from other biological fluids (saliva, tear fluid, etc.). Currently, there is no data indicating other routes of transmission (respiratory, contact, food, etc.).
Viral infections
HIV-infected patients are characterized by damage to the oral mucosa by herpes simplex. It occurs in the form of frequent and painful exacerbations of recurrent herpetic stomatitis, sometimes without remissions. Along with intraoral lesions, lesions of the genital organs are often observed, atypical in localization, long-lasting and painful. Vesicles appear on the tongue, soft palate, floor of the mouth, on the lips, and very quickly transform into erosions, which often turn into large ulcers (0.5-3.0 cm in diameter). Ulcers can take the form of a crater with raised, irregularly shaped edges and a brightly hyperemic bottom, which can be covered with a grayish-white coating. Without timely treatment, the process progresses, the size of the ulcers increases, which can subsequently lead to dissemination of the viral herpetic infection into the visceral organs. The severity of the clinical course of the disease increases, which can sometimes cause death.
The oral mucosa of HIV-infected patients is also quite often affected by herpes zoster. The disease occurs more often with AIDS. The clinical picture of herpes zoster in HIV infection can be different: from mild localized forms without postherpetic neuralgia to severe disseminated forms, with frequent relapses.
People infected with HIV have an increased incidence of lesions caused by human papillomavirus (papovaviruses). Most often the mucous membrane of the mouth, facial skin and perianal area are affected. These are nodular lesions: papillomas, epithelial hyperplasia, condylomas. In the oral cavity, nodular lesions are covered with multiple projections in the form of papillae. They are most often localized on the mucous membrane of the hard palate and gums.
“Hairy” leukoplakia (villous leukoplakia, flat condyloma, oral viral leukoplakia) is observed in HIV-seropositive patients and is a lesion associated with immunodeficiency and HIV infection. The presence of “hairy” leukoplakia is an indicator for screening for the presence of HIV. According to the latest literature data, 75% of the examined patients with “hairy” leukoplakia were HIV-seropositive.
Manifestations of “hairy” leukoplakia can vary in size and location, and can be unilateral or bilateral. The most typical localization is the lateral surfaces of the tongue, less often the process spreads to its entire surface and cheek.
Persons infected with HIV are infected for life. Most of them may not show any symptoms of the disease for several years and therefore will not suspect that they have an infection. During this period, they are a source of transmission of the virus to other people.
Clinical symptoms of HIV infection are numerous and varied. It can occur with aggressive secondary infections and various neoplasms.
HIV infection is characterized by alternating relapses and remissions, a staged course, and increasing severity of clinical symptoms and laboratory parameters. At the final stage of the disease, a complete acquired immunodeficiency syndrome is formed, which is irreversible and ends in death after various periods.
Taking into account WHO recommendations, V.I. Pokrovsky in 1989 proposed a clinical classification of HIV infection, according to which the course of this disease can be divided into 4 stages, although not all of them are necessarily observed in every infected person.
Clinical classification of HIV infection
- Incubation stage.
- Stage of primary manifestations.
- Acute infection.
- Asymptomatic infection.
- Persistent generalized lymphadenopathy.
- Stage of secondary diseases.
Decrease in body weight by less than 10%; fungal, viral, bacterial lesions of the skin and mucous membranes; shingles; repeated pharyngitis, sinusitis.
Reduction of body weight by more than 10%; unexplained diarrhea or fever that persists for more than 1 month; “hairy” leukoplakia; pulmonary tuberculosis; repeated or persistent viral, bacterial, fungal, protozoal lesions of internal organs; lesions of the skin and mucous membranes, accompanied by ulcerations; localized Kaposi's sarcoma.
Generalized bacterial, viral, fungal, protozoal and parasitic diseases; Pneumocystis pneumonia; lymphoid interstitial pneumonitis; esophageal candidiasis; generalized tuberculosis; atypical mycobacteriosis; cachexia; disseminated Kaposi's sarcoma; lesions of the central nervous system of various etiologies.
Terminal stage
The duration of stage I - the incubation stage - ranges from 3 weeks to 3 months, although in some cases it can be reduced to several days or increased to 1 year or more.
Acute infection (PA stage ) usually lasts 2-3 weeks. Typical clinical manifestations of this period are fever, lymphadenopathy, night sweats, skin rash, headaches and cough, nausea, vomiting, stool disorder, arthralgia, myalgia. Acute HIV infection is also characterized by the presence of leukopenia (lymphopenia) and thrombocytopenia. Serological tests for the presence of HIV become positive approximately 5-8 weeks after the onset of the acute phase of the disease.
Then HIV infection spontaneously turns into an asymptomatic infection or persistent generalized lymphadenopathy (PGL) develops, and sometimes the stage of secondary diseases immediately appears.
Asymptomatic infection occurs without any clinical manifestations. The duration of this stage can range from 2 to 10 years or more. The prevalence of such an infection is extremely high and exceeds the number of patients with manifest forms of the disease by hundreds and thousands of times.
Persistent generalized lymphadenopathy develops following an acute infection or against the background of an asymptomatic one. HIV infection is characterized by enlargement of lymph nodes of various groups (two or more) for at least 3 months. Most often, the process involves the cervical, axillary, inguinal, femoral and even popliteal lymph nodes. Their diameter is from 0.5 to 2 cm, sometimes 4-5 cm or more. As the disease progresses, lymphoid tissue atrophies. Lymph nodes become denser and decrease in size, usually already in the terminal stage.
As the immune system deficiency deepens, secondary diseases begin to appear. Stage 3 usually develops 3-5 years from the moment of infection, when the number of CO4 lymphocytes decreases to 400 cells per 1 mm3.
Subsequently, as the immune system disorders worsen, the severity of clinical symptoms increases. After about 5-7 years, HIV infection transforms into stage IIIB, and after 7-10 years from the moment of infection - into stage IIIB.
The transformation of the stage of secondary diseases into the terminal stage is elusive and is objectively characterized by a decrease in the number of helper cells to 200 cells per 1 mm3. As a result of irreversible immunodeficiency, the number of Thelpers continues to decrease until complete elimination, resulting in severe pathology of vital organs and systems (respiratory, digestive, central nervous system). The terminal stage inevitably ends in death.
A special place in the clinical symptom complex of HIV infection is occupied by lesions of the skin and mucous membranes. These changes can have important diagnostic significance, since they often make it possible to first suspect HIV infection in patients at an appointment with a dentist.
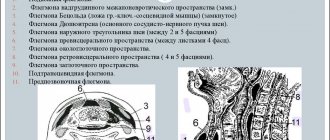
Diseases of the oral mucosa associated with HIV infection include the following:
- various clinical forms of candidiasis;
- viral infections;
- “hairy” (villous) leukoplakia;
- necrotizing ulcerative gingivostomatitis;
- progressive form of periodontitis (HIV periodontitis);
- Kaposi's sarcoma.
Diseases such as squamous cell carcinoma of the oral mucosa and lymphoma (non-Hodgkin's) should alert the dentist to the possibility of a patient being infected with HIV.
Candidiasis is a common intraoral symptom of HIV infection. The most typical is acute pseudomembranous candidiasis. In HIV-infected people, it lasts for a long time (months), so the term “acute” loses its meaning. Clinical manifestations are completely consistent with those of ordinary candidiasis. On the mucous membrane of the mouth there is a grayish-white coating, reminiscent of curdled masses. It is easily removed with a spatula, revealing a hyperemic mucous membrane underneath. Plaque is localized mainly on the mucous membrane of the cheeks, palate, tongue, floor of the mouth, and gums. Candidiasis should be distinguished visually from similar changes in leukoplakia and lichen planus.
Acute atrophic candidiasis resembles lesions of the oral mucosa due to allergies, hypovitaminosis C, B, B2, B6. The lesion is usually localized on the tongue as an area of hyperemia along its midline; filiform papillae are atrophied.
Chronic hyperplastic candidiasis is less common. The lesion is usually localized on both sides on the mucous membrane of the cheeks, hard and soft palate. In the corners of the mouth, candidal angular cheilitis and cracks with pronounced symptoms of epithelial hyperplasia often occur. Over time, cracks increase in size, become hard, and become crusty. Painful sensations may be absent or insignificant; patients note a burning sensation.
When differential diagnosis of candidiasis, symptoms of similar diseases should be taken into account:
- leukoplakia;
- lichen planus;
- allergic stomatitis;
- traumatic injuries.
Clinically, “hairy” leukoplakia is a thickening of the mucous membrane in the form of folds or white villi, rising above the surface of the oral mucosa and tightly attached to it. The lesions are in the form of a plaque formation of a grayish-white color (from 2 mm to 2-3 cm in height), have an uneven, wrinkled (“corrugated”) or with hyperkeratotic growths surface, which is as if covered with “hairs” or “villi” (due to thread-like epithelial growths). Subjective sensations are usually absent; sometimes mild pain or burning may occur.
- Ulcerative-necrotizing gingivostomatitis
A sign of HIV infection in the oral cavity is necrotizing ulcerative gingivostomatitis. The disease begins acutely or imperceptibly with bleeding gums when brushing teeth. The acute course of necrotizing ulcerative gingivostomatitis can last 3-4 weeks, after which the disease in many patients becomes chronic and often recurs. HIV-associated necrotizing ulcerative gingivostomatitis is characterized by a progressive course, leading to loss of gum tissue and bone structures, often with sequestration.
HIV-infected people may experience an aggressive form of periodontitis with generalization of the process in periodontal tissues. Severe bleeding and hyperplasia of the gums are noted, tooth mobility increases, diffuse destruction of the bone tissue of the alveolar process occurs, which is often accompanied by sequestration of the interdental septa.
- Kaposi's sarcoma
This is one of the most characteristic clinical manifestations of AIDS. The tumor is formed from lymphatic vessels. The skin of the extremities at the shin level is most often affected. It is more common among homosexual drug addicts (46%) than among heterosexuals (3.8%). The mucous membranes of the mouth and genitals, and the conjunctiva are affected in 30% of AIDS patients.
In the oral cavity, in most cases, Kaposi's sarcoma is localized on the hard and soft palate, in the area of the circumvallate papillae of the root of the tongue, and less often on the gums.
At the beginning of its development, Kaposi's sarcoma appears as erythematous spots with a diameter of 0.5-3.0 cm or dense elastic pale pink or brown nodules measuring 5x8 mm. Gradually, the nodes enlarge, an infiltrate forms under them, their color becomes cherry red, purple or brown.
Subsequently, the nodes are often divided into lobes and ulcerate. Ulcerations on the oral mucosa are observed much more often than on the skin. Lesions in the oral cavity are painful to the point of ulceration. Kaposi's sarcoma, localized on the gum, resembles epulis in appearance.
- Other manifestations
During any period of HIV infection, telangiectasias may appear in the oral cavity against the background of mild erythematous spots, as well as petechial and purpuric rashes.
Often, HIV-infected people develop desquamative glossitis, which may be associated with changes in microbiocenosis in the oral cavity against the background of secondary immunodeficiency.
With HIV infection, manifestations of Hodgkin's disease, characterized by inflammatory neoplastic processes (lymphogranulomatosis), are often found in the oral cavity. In addition, due to severe secondary immunodeficiency, trauma to the oral mucosa leads to the formation of long-term non-healing, sharply painful ulcers covered with putrefactive, necrotic plaque.
A critical part of effective routine HIV prevention is the use of traditional principles of sterilization and disinfection. To prevent the transmission of HIV, it is more than enough to follow recommendations for the prevention of infection with blood-borne infectious agents such as the hepatitis B virus.
The fight against HIV infection includes:
- precautions regarding blood and other body fluids (saliva, tear fluid, etc.);
- precautions during injections and procedures involving piercing the skin and mucous membrane of the mouth;
- effective sterilization and disinfection.
Most dental procedures are invasive, so they often result in bleeding. It is known that HIV is a blood infection, as a result of which the dentist is at risk of contracting HIV infection. Therefore, dentists, paramedics and paramedics must take precautions regarding blood and other body fluids (pus, saliva). Hands and other parts of the body contaminated with blood or other body fluids should be thoroughly washed with soap and water. After removing protective gloves, hands should also be washed immediately. Gloves should be worn for all direct contact with blood and other body fluids. During procedures that may produce splashes or suspensions of blood (for example, dispersal of aerosols from high-speed dental units and ultrasound machines), the eyes, nose, and mouth should be protected with a mask and goggles or a plastic visor. Needles, scalpels, discs, endodontic and other sharp instruments should be handled with extreme care to prevent punctures, cuts and other injuries. Disposable instruments must be destroyed after use. If injury from sharp instruments is possible (for example, during cleaning), it is recommended to wear additional thick gloves and handle the instruments with care. It is advisable to use special ultrasonic installations for mechanical cleaning of small instruments from dirt. Physicians with exudative skin lesions should not perform invasive procedures or treat infected patients.
An important condition for the prevention of HIV infection through instruments used to pierce the skin, mucous membrane, as well as other invasive procedures is their reliable sterilization. HIV is very sensitive to conventional sterilization and high-intensity disinfection methods. It is inactivated by methods designed to inhibit other pathogens (eg, hepatitis B virus). An effective method of inactivating HIV is high temperature. The most reliable methods for sterilizing instruments (including dental ones) are high-intensity sterilization and disinfection based on heating (boiling, autoclaving, sterilization with dry hot air).
High intensity disinfection can also be carried out using disinfectants: 2% glutaral solution (glutaraldehyde), 30% hydrogen peroxide solution. Soaking cleaned instruments in these solutions for 30 minutes provides high intensity disinfection.
Treatment of medical tables, drill tips and other surrounding surfaces is carried out with a solution of medium or low intensity disinfectants, such as chlorine-releasing compounds such as sodium hypochloride, calcium hypochloride, 4% chloramine solution, sodium dichloroisocyanurate, 4% chlorhexidine solution. The disinfecting ability of chlorine-releasing compounds is measured by the presence of “active” chlorine in them (as a percentage). For example, sodium hypochloride contains 5% “active” chlorine, calcium hypochloride – 70%, chloramine – 25%.
To treat body tissues, bactericidal agents are used - antiseptics (70% ethyl alcohol, 70% isopropyl alcohol, 1% iodine solution, 10% iodoform solution).
Dental material (impression material, material for determining bite, etc.) is disinfected by cleaning it from saliva and blood. Casts and intraoral orthodontic and orthopedic structures should be cleaned and disinfected before being sent to the laboratory.
After use, handpieces for drills are washed under a strong stream of water, and detergents are used to remove adhering material. They are then wiped with a material soaked in a disinfecting detergent, which is then washed off with distilled water.
Source: www.eurolab.ua