Risk factors
The main factors for the development of gingivitis include the following:
- Poor oral hygiene. Because of this, an accumulation of dental plaque is possible, which collects in the root areas and provokes the growth and development of pathogenic microorganisms.
- Chronic foci of infection in the oral cavity. These include caries, chronic tonsillitis and pharyngitis.
- Children under 3 years of age. Young children learn about the world around them through their mouths, and this can lead to inflammation. In addition, active tooth growth occurs during this period, which can also increase the risk of developing gingivitis.
- Adolescence. The high risk of developing pathology at this age is explained by active hormonal changes in the body.
- Pregnancy.
- Elderly age. At this age, people usually experience tooth loss and changes in metabolism in the body.
- Decreased immunity due to acute and chronic diseases.
- Chronic stress.
- Unbalanced diet, prolonged fasting.
- Smoking.
- Eating spicy and salty foods.
- Insufficient saliva production. The cause may be diabetes mellitus, abnormalities in the development of the salivary glands and Sjögren's syndrome.
- Menopause.
Causes
The causes of gingivitis can be different, let’s look at what can cause this disease:
- Pathogenic microorganisms. Most often these are staphylococci and streptococci. These are microorganisms that live in the oral cavity for a long time, but when unfavorable factors develop, they cause inflammation.
- Traumatization of the gums. Often occurs when wearing dentures for a long time, or malocclusion.
- Stomach diseases. With the development of stomach pathology, acidic contents may be thrown into the oral cavity. Because of this, a chemical burn of the gums and inflammation occurs.
- Intestinal diseases. The most common cause of gingivitis is acute Crohn's disease.
- Diabetes. Gingivitis against the background of diabetes mellitus develops due to impaired microcirculation in the mucous membranes and decreased immunity.
- Leukemia (cancer of the bone marrow). In the development of this disease, gingivitis is the main clinical manifestation.
- HIV infection (AIDS).
- Intoxication of the body. Occurs against the background of an overdose of drugs or when the body is poisoned with heavy metal compounds (mercury, lead).
- Side effects of medications. During chemotherapy in cancer patients, gum inflammation is a fairly common side effect.
- Avitaminosis. It occurs against the background of insufficient intake of vitamin E and B vitamins into the body.
- Scurvy (a disease caused by too much vitamin C in the body).
- Acute diseases of the oral cavity. Stomatitis may be accompanied by gum inflammation. This phenomenon often occurs in children in the first year of life.
- Anemia (most often iron deficiency).
Stages of development of gingivitis and gum disease
Classification
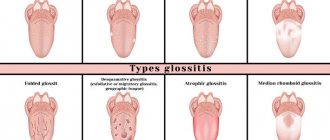
Gingivitis, the treatment and symptoms of which may vary, is divided into the following types:
- Catarrhal gingivitis
. Symptoms are characterized by hyperemia of the gum tissue, enlarged papillae, swelling and bleeding even with light pressure on the gums. Catarrhal gingivitis is the most common clinical case of the pathology.
- Ulcerative gingivitis
. Symptoms of this form are characterized by the appearance of ulcers on the gums, which are initially covered with a film, and when opened, reveal an erosive surface.
- Ulcerative-necrotizing gingivitis
. This type is a complication of ulcerative gingivitis, but in addition to erosions, necrotization of areas of inflammation occurs.
Necrotizing ulcerative gingivitis, photo
- Hypertrophic gingivitis
. Symptoms cause discomfort: there is an increase in gingival papillae, deepening of periodontal pockets by more than 2 mm. The gums in this form are swollen, and slight hyperemia is observed.
Hypertrophic gingivitis, photo
- Atrophic gingivitis
. Symptoms of this form are characterized by a decrease in gum tissue, the papillae shrink, and are less noticeable upon examination.
According to the course, gingivitis is divided into:
- acute gingivitis;
- chronic gingivitis;
- recurrent gingivitis.
According to the severity of gingivitis:
- mild severity;
- moderate severity;
- severe gingivitis.
According to the degree of affected areas, gingivitis is:
- localized (separate areas of inflammation);
- generalized (the entire gum area is affected).
Gingivitis - classification
Gingivitis is classified into the following types:
By shape
Acute gingivitis. Inflammation of the gums is accompanied by frequent pain, bleeding and other signs of the disease, almost without stopping.
Chronic gingivitis. The inflammatory process worsens mainly in winter and spring, which is primarily due to a lack of vitamins in the body.
By severity
Mild degree. Characterized by a mild course of the disease. The interdental papillae are predominantly affected.
Average degree. In addition to the interdental papillae, the inflammatory process also affects the marginal (free) gum.
Severe degree. Inflammation spreads to the entire gum, including its alveolar part.
Read also: Extrasystole - causes, symptoms, diagnosis, treatment and prevention
By localization
Localized gingivitis. One or several sections of the gum, independent of each other, are subject to inflammation.
Generalized gingivitis. The inflammatory process spreads to the gums in the area of all teeth, one or both jaws.
By the nature of the lesion
Catarrhal gingivitis. It is characterized by swelling, redness, bleeding, slight itching in the affected area, pain when eating, bad breath, impaired taste, cyanosis of the gums and a slight increase in body temperature (up to 37-38°C).
Atrophic gingivitis. It is characterized by a decrease in inflamed gum tissue, gradually exposing the root of the tooth. The main signs of atrophic gingivitis are pain when the inflamed gums come into contact with cold and hot. Some of the main reasons are underdosed orthodontic treatment, insufficiency of the alveolar base, as well as disturbances in the growth and development of parts of the gums (frenulum, gingival ligaments).
Hypertrophic gingivitis. It is characterized by an increase in gingival papillae, which, depending on the severity, can cover from 1/3 to 2/3 of the tooth, and even completely cover it. The insidiousness of this type lies in the absence of clinical symptoms of the disease in the initial stages, so this type of disease can be classified as a chronic form. Signs of hypertrophic gingivitis are bleeding and soreness of the gums when it comes into contact with food, bad breath, and rarely, death of the tips of hypertrophied gingival papillae. Among the most common causes are hypovitaminosis C, diseases of the endocrine and circulatory systems, taking diphenin drugs, and malocclusion. According to localization, it most often appears on the frontal part of the gingival margin of the vestibular surface of the front teeth.
Ulcerative or ulcerative-necrotizing gingivitis. It is characterized, first of all, by the appearance of ulcers and necrotic areas at the site of inflammation. In addition, ulcerative-necrotic gingivitis is characterized by the presence of an unpleasant odor from the oral cavity, severe soreness of the gums when eating, general weakness, enlarged lymph nodes, bluish gingival margins, swelling, bleeding of the inflamed gums at the slightest injury and an increase in temperature, up to 39 ° C , coating on the tongue, viscous and viscous saliva. When complications occur, the gingival papillae and marginal gums die. Children with ulcerative gingivitis may behave nervously, sleep poorly, and rapidly lose weight. Ulcerative gingivitis develops due to serious disturbances in the body's reactivity, which may be caused by general diseases or a decrease in the resistance of gingival tissue. This type appears mainly after the catarrhal type of gingivitis. Thus, doctors note that ulcerative gingivitis is often observed in people who have suffered from diseases such as influenza, ARVI, stomatitis, after hypothermia, teething, etc.
Gingivitis according to ICD-10
In accordance with the International Classification of Diseases, 10th revision (ICD-10), gingivitis is assigned code K05 - “Gingivitis and periodontal diseases.” Classification according to ICD-10:
- K05.0 – Acute gingivitis;
- K05.1 – Chronic gingivitis: NOS;
- desquamative;
- hyperplastic;
- simple marginal;
- ulcerative gingivitis.
- Periodontal abscess
- Chronic pericoronitis
- NOS;
- Juvenile periodontal disease
Symptoms of gingivitis
Let's look at the symptoms of gingivitis depending on the type and form in the table below.
| Kinds | Symptoms of gingivitis |
| Acute gingivitis (catarrhal) | Pain syndrome, hyperemia (redness) of the gum tissue, itching, bleeding of the gums when brushing teeth or while eating, sensation of a foreign body in the area of inflammation. In young children, there may be an increase in body temperature and increased salivation. |
| Chronic gingivitis (catarrhal) | Chronic catarrhal gingivitis causes mild pain in the gums when brushing teeth or when eating solid food, and periodic bleeding of the gums. |
| Ulcerative gingivitis | Ulcerative gingivitis is characterized by the following symptoms: severe pain, difficulty eating, sharp pain when brushing teeth, severe bleeding of the gums, increased body temperature, unpleasant odor from the mouth, and the appearance of ulcers on the gum mucosa. |
| Hypertrophic gingivitis (edematous form) | Hypertrophic gingivitis causes pain when brushing teeth, swelling of the gum tissue, and bleeding. |
| Hypertrophic gingivitis (fibrous form) | Pain when brushing teeth and while eating, overgrowth of gum tissue, unusual appearance of gums (hypertrophy), bleeding, unpleasant odor. |
| Atrophic gingivitis | There is a decrease in gum tissue, and dental pockets are exposed. The gum papillae are smoothed. On examination there was moderate hyperemia. |
| Ulcerative-necrotizing gingivitis | The pain syndrome is pronounced, there is pain when swallowing, increased body temperature, putrid odor from the mouth, intoxication of the body (weakness, lack of appetite). The formation of areas of necrosis in the gum tissue and sometimes on the mucous membrane of the inner surface of the cheeks is observed. |
Features of gingivitis in various conditions
Let's look at some of the features that gingivitis symptoms may have in various conditions.
| State | Peculiarities |
| Pregnancy | Manifests itself in the form of swelling of the gum papillae. The appearance of edema in the first trimester of pregnancy is typical. The appearance of granulomas (benign growths on the gums) is observed, which disappear after childbirth. |
| Leukemia | The gums look like “blood engorged” due to the presence of leukemic infiltration. |
| Diabetes | Ulcerative gingivitis is characteristic. |
| Scurvy | Pronounced inflammation, hematomas on the gums, severe bleeding. |
Symptoms
In the initial stage of generalized periodontitis, bleeding gums, their swelling and looseness are noted; itching, pulsation and burning in the gum area, pain when chewing food, unpleasant odor from the mouth. Dental pockets are shallow and located mainly in the interdental spaces. There is no mobility or displacement of teeth; the patient's general condition is not impaired. The clinical picture of developed generalized periodontitis, in addition to the listed symptoms, is characterized by loosening and displacement of teeth, increased sensitivity (hyperesthesia) of teeth to temperature stimuli, and difficulties with chewing food. In severe cases, generalized periodontitis leads to disruption of general well-being - weakness and malaise, increased body temperature, acute pain in the gum area. Regional lymph nodes enlarge and become painful. A dental examination reveals signs of diffuse hypertrophic gingivitis, abundant accumulations of soft dental plaque, supra- and subgingival dental deposits, severe traumatic occlusion, multiple periodontal pockets of various shapes and depths, often with serous-purulent or purulent contents. In advanced stages of generalized periodontitis, tooth loss, formation of periodontal abscesses and fistulas may occur. Metallic taste in the mouth. Malaise. Weight loss.
Diagnostics
The main diagnostic method is an examination of the oral cavity by a dentist. On examination, gum hyperemia and swelling are observed. The structure of the tissues is loose, there is a noticeable increase in the periodontal pockets.
If there is any doubt about making the correct diagnosis, additional research is needed. For example, when the etiology of inflammation is unclear.
The patient is prescribed the following studies:
- Clinical blood test. It is carried out for a general assessment of the body’s condition and identification of inflammatory reactions.
- Blood chemistry. It is performed to assess the level of certain biological substances in the body (glucose, iron).
- Blood test for HIV infection, syphilis and viral hepatitis.
- Immunological blood test.
- Bacteriological examination of saliva. Carried out to identify the pathogen.
- X-ray examination of teeth (to exclude the development of periodontitis).
- Consultations with specialist doctors (if there are concomitant diseases). Consultation with an endocrinologist, hematologist and gastroenterologist may be required.
- Schiller-Pisarev test. It is stained with an iodine-containing solution. If inflammation is present, pigment will accumulate in the area.
- Probing. This procedure allows you to determine the integrity of the dentogingival junction and exclude the development of periodontitis.
Differentiated diagnosis
Carry out with the following diseases:
- Mild periodontitis.
- Acute leukemia.
- Stomatitis, including a combination of these two pathologies (Vincent gingivostomatitis).
- Agrunolocytosis (decreased immunity due to the patient receiving radiation or chemotherapy).
Differences between gingivitis and periodontitis
Since gingivitis is an inflammation of the gum tissue, an x-ray will not reveal changes in the bone tissue. With the development of periodontitis, the formation of dental pockets and tooth mobility occurs. If the disease progresses, tooth loss may occur.
Gingivitis is often the initial stage of periodontitis.
Prevention
Early and adequate initiation of treatment for generalized periodontitis allows one to achieve stable clinical remission and prolong its duration. Subsequent compliance with recommendations for preventive measures plays an important role in the restoration of periodontal tissue and preservation of the function of the dental system. In advanced stages of generalized periodontitis, an unfavorable prognosis may be associated not only with tooth loss, but also with the development of severe systemic complications from the cardiovascular system.
Source
Treatment of gingivitis
For each type of inflammatory process, treatment has its own characteristics.
Catarrhal gingivitis
Treatment during the acute period of the disease (if symptoms develop that cause concern to the patient) is symptomatic therapy. Let's look at how to treat catarrhal gingivitis.
- Preparations based on lidocaine. Available in the form of ointments or gels. Their use is necessary if the pain syndrome in the area of inflammation is pronounced. It is necessary to apply this drug until pain is completely eliminated.
- Antibacterial ointments or gels. To stop the development of inflammation in the gum tissue, anti-inflammatory drugs are prescribed. These include Mitrogil - Denta or Cholisal. The course of treatment with these drugs usually takes up to 10 days.
- Rinse with antiseptic solutions. You can use chlorhexidine, decoctions of medicinal plants and other drugs with antimicrobial properties. You need to rinse your mouth after every meal. This will help remove food debris and relieve inflammation from the gum tissue. The course of treatment can take a period of time from 14 days to 1 month.
After the main symptoms subside, professional teeth cleaning is recommended. In this case, the doctor will remove all dental deposits (stones, plaque). After professional cleaning, be sure to rinse with antiseptic solutions.
In addition, complete rehabilitation of chronic foci of inflammation in the oral cavity is necessary. This will help in the future to avoid inflammation becoming chronic.
Ulcerative gingivitis
Treatment of this type of pathology is generally similar to the treatment of catarrhal gingivitis. But still, ulcerative gingivitis has its differences:
- Antibacterial therapy. Includes the use of antibiotics; the choice of a specific drug occurs after identifying the pathogen. But during the height of the disease, with a high risk of complications, broad-spectrum antibiotics (Amoxiclav, Cefepime) are used.
- Antipyretic drugs (at temperatures above 38℃).
- Rinsing the mouth with antiseptic solutions.
- Treatment of inflammation areas with anti-inflammatory ointments.
- Refusal of solid food.
- Drink plenty of fluids (to reduce symptoms of intoxication).
After the patient’s condition improves and symptoms disappear, cleaning the oral cavity and sanitation of chronic foci of infection are recommended.
Ulcerative-necrotizing gingivitis
Treatment of this form has a peculiarity - at the very beginning of the disease it is necessary to follow the principles of symptomatic, antibacterial therapy, as well as surgical intervention, since the patient’s condition with this form of gingivitis suffers the most.
Symptomatic treatment of necrotizing ulcerative gingivitis includes:
- Antipyretic drugs (ibuprofen, paracetamol).
- Pain relieving gels or ointments.
- Drink plenty of fluids.
- Mechanically gentle food.
Antibacterial therapy includes not only local, but also systemic use of drugs.
Antimicrobial drugs are prescribed both for oral administration and for intramuscular or intravenous use.
In addition, for this form of gingivitis the following is prescribed:
- Surgical removal of areas of necrosis using a laser.
- Rinse with antiseptic solutions.
- Careful oral hygiene.
With this form, concomitant pathology is often observed, so an important role is assigned to its treatment.
Often, against the background of ulcerative-necrotic lesions of the gums, fungal and herpetic inflammation occurs, the cause of which is gingivitis. Treatment for these pathologies is described in the table below.
| Type of concomitant pathology with gingivitis | Treatment |
| Candida inflammation | Antifungal drugs (tablets, lozenges, antifungal creams). |
| Herpetic rashes | Antiherpetic drugs (tablets and ointment Acyclovir). |
Hypertrophic gingivitis
Treatment prescribed upon diagnosis of hypertrophic gingivitis involves the use of the following methods:
- Professional teeth cleaning to remove plaque.
- Gum treatment.
- Rinsing.
- Physiotherapeutic procedures.
- Gum massage.
- Introduction of medicinal solutions into the gingival papillae.
- Hormonal ointments.
- Systemic use of glucocorticosteroids or drugs containing sex hormones (during menopause).
- Surgical intervention (if conservative treatment is ineffective).
Atrophic gingivitis
Its treatment involves a combination of conservative and surgical therapy.
Conservative treatment includes:
- Professional teeth cleaning.
- Physiotherapeutic treatment (electrophoresis, ultrasound).
- Gum massage.
- Rinse with antiseptic solutions.
- Careful oral hygiene.
Surgical treatment involves the reconstruction of gum tissue to close open areas. This operation is called gingivoplasty.
Traditional methods of treatment
To treat gingivitis, you can also use various medicinal preparations, essential oils, lotions from medicinal plants, and rinsing the mouth with decoctions.
Decoctions for rinsing can be prepared from eucalyptus, St. John's wort and yarrow and from oak bark. They have anti-inflammatory, healing and antiseptic effects.
For rinsing, use alcohol tincture of propolis. You can buy it at the pharmacy or prepare it yourself. For preparation you will need propolis and alcohol. Propolis needs to be cleaned and soaked in warm water. Then blot well and fill with alcohol. After this, let it brew for several days.
The remedy made from alder cones has proven itself well. To prepare, you need to take a small amount of cones, grind them using any convenient method and pour boiling water over them. Then let it brew for several hours. After which the finished infusion must be strained. You need to rinse 2 times a day for 10 days.
Infusions for rinsing should be comfortable in temperature and quite warm, but not scalding.
In addition to rinsing agents, you can use lotions. To prepare them, you need to take some juniper berries, chop them well and soak in boiling water for several hours. Then squeeze well and grind again to a paste.
The product should be applied to a cotton pad and rubbed into the gums. The course of treatment is about 14 days.
Treatment
TREATMENT Local treatment • It must begin with careful removal of dental plaque, especially subgingival plaque using a scaler (Pieson - master - 400). It includes the whole range of local effects: medication, orthopedic and physiotherapeutic. Eliminate local causes that led to the development of inflammation. For longer contact of drugs with periodontal tissues, gingival dressings or forms with a prolonged action are used. • Of particular importance are surgical methods (curettage, gingivitomy, flap operations, etc.) performed on the gums and bone tissue, which are aimed at removing granulations, eliminating periodontal pockets, restoring defects in the bone tissue of the alveolar process, etc. Surgical intervention is recommended to be combined with drugs , promoting the regeneration of periodontal tissue (keratoplasty). Teeth that have mobility are splinted. It is mandatory to remove teeth that have no functional value. To avoid overloading the existing/remaining teeth, direct prosthetics are recommended. • Physical therapy can be varied, including ultrasound and low-level laser radiation. Hydrotherapy in the form of irrigation of the oral cavity with water saturated with carbon dioxide has not only a therapeutic effect, but also improves oral hygiene.
General treatment is mainly carried out for exacerbations of chronic generalized periodontitis and in the presence of severe general somatic pathology (hereditary neutropenia, type 1 diabetes, etc.). It includes: broad-spectrum antibiotics, desensitizing and sedatives, immunotropic drugs (imudon, xymedon). Sometimes hormonal therapy and drugs that affect mineral metabolism (thyrocalcitonin) are prescribed. General treatment is combined with specific therapy for the general disease and vitamin therapy. Prevention • Timely treatment of gingivitis • Careful oral hygiene • It is advisable to use resort factors (balneotherapy and peloid therapy). The physical and chemical properties of mineral waters, therapeutic mud and climatotherapy have a healing effect on the oral cavity and the entire body.
ICD-10 • K05.2 Acute periodontitis • K05.3 Chronic periodontitis.
Features of the course of gingivitis in children
Gingivitis in children is considered one of the most common dental diseases. Most often it occurs against the background of teething in children under 3 years of age. This type is called "eruptive gingivitis."
When teething, inflammation of the gums occurs in the place where a new tooth should erupt. The inflammation affects only this area and does not spread to the rest of the gum.
When teething, gingivitis can be provoked by insufficient oral hygiene in the child or injury from eating solid food, using a rough brush, or if the child has the habit of putting various toys in his mouth.
If the child is older, a situation may occur when, when brushing teeth, the child diligently avoids the site of inflammation (due to pain). As a result, plaque accumulates and pathogenic microorganisms spread. In this case, inflammation can also spread to the oral mucosa and we can talk about the development of gingiostomatitis.
In addition, gingivitis in children can occur due to immaturity of gum tissue, decreased immune defense (including during teething), and gastrointestinal diseases.
The course of gingivitis in children also differs compared to presentation in adulthood. In childhood, the disease is more pronounced. The symptoms are more severe and can cause significant discomfort to the child.
Symptoms of gingivitis in children
Catarrhal gingivitis occurs most often in children.
. It can be local (at the site of tooth eruption, injury) and generalized. The severity of clinical manifestations will depend on the prevalence of the pathology. As a rule, in children, catarrhal gingivitis is accompanied by the following symptoms:
- Increased body temperature (37-37.5℃). Fever above these values with catarrhal gingivitis is not observed in most cases. If the temperature is higher than these values, then we can talk about the addition of a bacterial infection or the development of a viral disease.
- Breast refusal in children under 1 year of age or sluggish sucking reflex.
- Poor appetite, refusal to eat.
- Pain when chewing and swallowing.
- Profuse salivation.
- Itching in the affected gum.
- Lethargy, poor sleep.
Catarrhal gingivitis in a child, photo
All these symptoms disappear within 3-4 days with proper treatment. Hospitalization of a child with the development of catarrhal gingivitis is not required. Treatment of gingivitis occurs at home.
Ulcerative gingivitis
occurs in children against the background of a viral or bacterial infection and is more pronounced in nature compared to catarrhal. Symptoms may be accompanied by pronounced intoxication.
Clinical picture of ulcerative gingivitis in children:
- Increased body temperature above 37.5℃. Can reach values of 38.5-39.5℃.
- Intoxication syndrome (weakness, lethargy, feeling of muscle pain, poor sleep, thirst).
- Inability to eat due to pain.
- Poor appetite.
- Pain when swallowing.
- Salivation.
- Bad breath.
- Enlarged submandibular lymph nodes.
- Itching at the site of inflammation.
Upon examination, extensive hyperemia (redness) and the appearance of ulcers at the site of inflammation are revealed.
Ulcerative gingivitis is often complicated by stomatitis. Treatment of this disease is difficult, especially in young children. If the condition worsens, hospitalization may be indicated. But this usually happens if there is any concomitant disease, for example, a severe viral or bacterial infection. Gingivitis is often provoked by tonsillitis, scarlet fever, infectious mononucleosis, and measles.
Gingivitis is also not uncommon in adolescence. Children of this age are susceptible to any type of pathology. But hypertrophied gingivitis
. It occurs under the influence of hormones that are actively produced during puberty.
It usually manifests itself in an edematous form. The gums change their shape, swell, and become more pronounced redness. Slight bleeding and bad breath may occur. Often this form of gingivitis in adolescence can go undetected for a long time.
Atrophic gingivitis in children
and adolescents is less common than all other species. Basically, the manifestation of this pathology occurs when devices for aligning the bite in children are installed incorrectly or due to inadequate operation during their use.
Such devices significantly worsen oral hygiene. The child may not clean the oral cavity sufficiently, which can cause inflammation and cause atrophic gingivitis.
Treatment of gingivitis in children
Treatment of gingivitis in children is in many ways similar to therapy in adults. But for children, treatment methods are still more gentle. Acute gingivitis requires the following treatment measures:
- Broad-spectrum antibiotics (for ulcerative gingivitis).
- Antipyretics (paracetamol, ibuprofen).
- Antibacterial gels.
- Mouth rinse.
- Mechanically gentle food (soups, cereals, purees). Such a diet is needed in the acute period, so as not to injure the inflamed gums.
When the symptoms of the acute period subside, the principles of further treatment of gingivitis include the following points:
- Cleaning plaque and tartar.
- Sanitation of the oral cavity.
- Regular rinsing with antiseptic solutions (chlorhexidine, chamomile decoction).
- Antibacterial gels (Cholisal).
- Strengthening the immune system.
- Selecting a toothbrush.
- Regular oral hygiene.
Helping your baby with teething
To reduce the risk of developing gingivitis and reduce the severity of symptoms (itching, pain), the following methods are used:
- Careful oral hygiene with a soft toothbrush.
- In children after 3 years of age, rinse with a weak chamomile decoction.
- Using teethers. The main condition is its thorough disinfection.
- Gum massage. It must be carried out with clean hands, using a napkin soaked in water or an antiseptic solution.
- Anti-inflammatory gels (Baby-Doctor). It should be remembered that the use of lidocaine-based gels is prohibited for children under 2 years of age.
Description
Generalized periodontitis.
A common destructive and inflammatory process that affects the entire complex of periodontal tissues. Generalized periodontitis occurs with bleeding and swelling of the gums, pain, bad breath, the presence of dental plaque, the formation of periodontal pockets, mobility and dislocation of teeth. Diagnosis of generalized periodontitis is carried out by a periodontist using an examination of the oral cavity, determination of the hygiene index and periodontal index, orthopantomography, and biopsy of gum tissue. Treatment of generalized periodontitis includes local conservative and surgical treatment; general anti-inflammatory and immunomodulatory therapy.
Gingivitis in pregnant women
Pregnant women experience gingivitis quite often. This is due to hormonal changes in the body during pregnancy, decreased immunity and a lack of vitamins and minerals.
As a rule, hypertrophic or catarrhal gingivitis occurs in pregnant women. But against the background of catarrhal disease, a combination of herpetic and candidal gingiostoamatitis can occur.
Symptoms of gingivitis in pregnant women are, in most cases, swelling, bleeding and pain. But with the development of a fungal infection, a whitish coating is observed on the gums and mucous membranes of the oral cavity.
If a woman has developed a herpetic lesion, then upon examination a rash in the form of blisters filled with serous contents will be observed. Subsequently, they open and ulcers form in their place.
Herpetic lesions pose a significant threat to the pregnant woman and the fetus. Therefore, it is necessary to begin treatment as quickly as possible.
Treatment of gingivitis in pregnant women has its own difficulties. This is due to the fact that many drugs are not recommended for use during pregnancy. But there are some drugs that are not contraindicated during pregnancy.
First, a pregnant woman undergoes professional cleaning of the oral cavity, then the mandatory use of rinsing solutions is prescribed. The safest remedy during pregnancy is a 0.5% chlorhexidine solution.
You can also choose decoctions of medicinal plants (chamomile, eucalyptus, oak bark) as rinses.
Anti-inflammatory ointments are used to relieve inflammation. During pregnancy, heparin ointment or 3% acetylsalicylic ointment is used.
In pregnant women, vacuum massage of the gums is widely used to treat gingivitis. This type of treatment is the safest for use during pregnancy.
In addition, physiotherapeutic procedures are indicated for pregnant women. Electrophoresis treatment is mainly used.
The use of antibacterial drugs is possible if the course of gingivitis is severe and there is a tendency to develop complications.
In this case, treatment can be carried out using approved drugs.
These include penicillin antimicrobials (Amoxiclav, Amoxicillin) and cephalosporins (Suprax).
Surgical treatment (if conservative methods are ineffective) is avoided during pregnancy.
The operation is performed after childbirth.
Gingivitis - treatment
Treatment of gingivitis is carried out in stages and includes:
1. Cleaning your teeth. Thorough cleaning of teeth and oral cavity is carried out. Plaque is removed from the teeth and tartar is removed. The cleaning procedure is carried out mainly with an ultrasonic device, unless there are contraindications. Next, the teeth are polished.
2. Anti-inflammatory therapy. This stage begins with rinsing, which is necessary to remove dirt from the surface of the teeth, especially after eating. Such products as Chlorhexidine, Furacilin, Furamistin are excellent for rinsing. Among the herbal remedies one can highlight calendula tincture, Japanese Sophora tincture, chamomile decoction, and arnica flowers. Rinsing should be done after each meal, first with plain water, then with a solution of the above products.
To reduce swelling, bleeding and other signs of inflammatory processes, anti-inflammatory gels and ointments are used after rinsing. They also promote pain relief and faster wound healing. For this purpose, products such as “Acepta gel”, “Solcoseryl”, “Cholisal”, “Apident - active” have proven themselves well. Before using the products, the gums must be dried. The course of treatment ranges from several to 20 days, depending on the remedy and the severity of gum inflammation.
Read also Skin cancer - first signs, symptoms, causes and treatment of skin cancer
For local anti-inflammatory therapy, non-steroidal anti-inflammatory drugs can also be prescribed - 0.1% solution of mephenamine sodium salt
3. After the symptoms of gingivitis have reduced, the dentist examines the teeth and, if necessary, treats the possible causes of this disease - caries. In addition, in the presence of other diseases, symptomatic treatment is carried out, therefore, treatment of gingivitis can often be carried out by two or three doctors at once, for example, a dentist, endocrinologist or gastroenterologist.
4. Antibacterial therapy. For gingivitis of infectious etiology, herbal antibacterial drugs are prescribed - “Novoimanin”, “Sodium usinate”, “Salvin”.
5. Treatment of ulcerative-necrotic gingivitis includes taking antihistamines (Suprastin, Claritin, Agistam), a diet (rich in easily digestible proteins and vitamins), drinking plenty of fluids, and vitamin therapy (C and P).
6. Surgical intervention. If there are necrotic areas (dead tissue), surgical treatment is performed. It is also used for hypertrophic gingivitis, if the tooth is completely covered with gum tissue.
7. Recovery. After the main course of treatment, medications are prescribed to restore the gum mucosa.
8. Orthodontist. If necessary, to correct pathologies in the development of teeth and jaws, treatment by an orthodontist is recommended.
Additional treatment
In addition to the main treatment, the attending physician may prescribe the following medications:
1. Vitamin therapy. Additional intake of vitamins helps to speed up the relief of gum inflammation. Particular emphasis is placed on taking vitamins C (ascorbic acid), P (rutin and other bioflavonoids), A (retinol), E (tocopherol) and U (methylmethionine). Among the vitamin complexes you can oh, Pangexavit tablets
2. In case of severe swelling of the gums , drugs are used to reduce hypertrophy (sclerosing drugs) - “Maraslavin”. For the same purposes, electrophoresis of a solution of ronidase or lidase in a buffer solution (pH 5.2) is used.
3. For severe pain, painkillers are used - Solcoseryl, Metrogyl and Apident-Active.
4. For severe bleeding, use decoctions of yarrow herbs and nettle leaves.
5. To normalize metabolic processes , the functioning of blood vessels, and relieve vascular spasms, Heparin helps well.
6. To protect the nerve endings through which pain is actually transmitted, preparations based on tannins are used. These products also help relieve gum swelling and strengthen its tissue. Among the plants with tannins can be noted - serpentine rhizome, cinquefoil rhizome, burnet rhizome and root, blueberries (fruits), oak bark, viburnum bark, bird cherry fruits, pine needles. They can be used as decoctions for mouth rinsing, applications, and lotions. Among medicines – “Tannin”.
7. For chronic catarrhal gingivitis, hydrotherapy with carbon dioxide is used, as well as electrophoresis (5% ascorbic acid solution or 1% galascorbine solution).
8. When treating gingivitis in children , to strengthen the capillaries of the gums, as well as to reduce swelling, it is recommended to use anti-inflammatory drugs of plant origin - decoctions of sage, mallow, marshmallow root, chamomile flowers, flavonoids. For the same purposes, plant phenolic compounds are excellent, which are similar in their action to steroidal anti-inflammatory drugs, but are softer, non-toxic and gentle.
Important! The use of any medications - gels, ointments, applications, etc. can only be started after rinsing the mouth and drying it, and after consulting a doctor!
Read also Mastitis - first signs, symptoms, treatment and prevention of mastitis
Features of the course of gingivitis in people over 60 years of age
Gingivitis in older people is not such a rare occurrence. The manifestations of this pathology depend on the condition of the oral cavity in older people. Often, with age, the condition of teeth worsens, some of them may decay and fall out.
The main factors for the development of gingivitis in older age:
- Changes in metabolism.
- Lack of vitamins and minerals.
- Chronic foci of infection.
- Decreased levels of sex hormones in women.
- Dry mouth and lack of saliva.
The course of gingivitis in old age is more likely to be chronic. An atrophic type of development of the disease is also possible. Symptoms of pathology correspond to the development of pathology at a younger age. But in some cases, a more muted clinical course is possible.
To treat gingivitis, the same methods are used as in the main age group.
Particular attention is paid to the prevention of gingivitis. In old age, it is important to eat a balanced diet, eating foods rich in calcium. This helps strengthen teeth and prevent tooth loss.
Nutrition for gingivitis
Treatment of gingivitis also involves dietary restrictions. During the period when acute gingivitis occurs, you need to adhere to the most gentle food possible. You should eat easily digestible foods; the nature of the food in the acute period should be pureed. You should avoid salty and spicy foods, which can increase pain.
The following products should be included in the diet:
- Fruits (green apples, pears, citrus fruits).
- Vegetables (cabbage, zucchini, carrots).
- Dairy products (milk, cottage cheese, cheese).
- Spices. For example, turmeric. It has natural antiseptic properties and prevents the growth of bacteria.
- Multivitamin complexes. These drugs are necessary if there are not enough vitamins in the food (in winter).
Prevention of gingivitis
To prevent the development of pathology, you must adhere to the following preventive measures:
- Completely clean the oral cavity. You need to brush your teeth 2 times a day (morning and evening), thoroughly using a toothbrush to clean all hard-to-reach places where food debris may accumulate. It is necessary to rinse your mouth with water after every meal.
- Use antiseptic mouth rinses after every brushing.
- Choose the right toothbrush. Its bristles should not be too hard, as such a brush can injure the gums.
- Timely undergo a preventive examination by a dentist. The frequency of such inspections is once every 6 months.
- Have your teeth professionally cleaned by a dentist.
- Sanitize chronic foci of infection in the mouth and throat.
- Treat chronic somatic pathologies or control their development.
- Increase immunity.
- Follow a balanced diet, exclude sweets, too spicy and salty foods from your diet.
- To refuse from bad habits.
Complications
The most basic consequence that gingivitis causes is periodontitis, which can lead to tooth decay and loss. In addition, the following possible complications are identified:
- Transition of gingivitis into a chronic form. This may occur due to improper treatment of an acute process. The chronic form of gingivitis is characterized by periodic bleeding, pain, and redness of the gums. There may be an unpleasant odor from the mouth. The chronic course of the pathology is difficult to treat and requires longer treatment.
- Ulcerative-necrotizing gingivitis. Treatment in this case becomes more complicated. This form may develop from ulcerative gingivitis. This course is characterized by a less favorable prognosis for the patient compared to other types of inflammation. Necrotizing ulcerative gingivitis does not respond well to conventional antibacterial therapy and can cause further spread of infection. One of the complications of this type of gingivitis is the development of Vincent's angina, as well as possible infection of the skull bones and the development of purulent inflammation in them. Such inflammation can develop in people with severe immunodeficiency (HIV infection, cancer, diabetes).
- Osteomyelitis. It is an acute purulent inflammation of the periosteum. Mostly occurs against the background of acute ulcerative gingivitis. This complication is possible with inadequate treatment of the disease, late seeking medical help, or in people who have concomitant chronic diseases (mainly with a low level of immune defense).
- Chronic diseases of the pharynx and tonsils. Gingivitis can lead to the development of chronic pharyngitis (inflammation of the pharynx) and tonsillitis. This leads to decreased human immunity and increased sensitivity to respiratory diseases.
- Gingiostomatitis.
- Herpetic lesions of the gums and mucous membranes.
- Candida inflammation.
- Formation of abscesses. For example, with advanced gingivitis (especially ulcerative), a peritonsillar abscess may occur. This complication requires urgent surgical intervention.
- Spread of infection by hematogenous route. Inflammation of the kidneys, joints and heart may develop. Most often this is possible due to infection with streptococcus. Also, in weakened patients (during chemotherapy), such inflammation can provoke the development of sepsis.
- Sepsis. It does not occur in all patients with gingivitis. The state of immunity and the presence of concomitant severe somatic pathologies are of decisive importance for this pathology. Also, such extensive infection is possible against the background of necrotizing ulcerative gingivitis and its complications.
Complications of gingivitis can pose a serious risk to human health. Therefore, gingivitis requires a serious approach to treatment. Treating gingivitis as early as possible is the best prevention of complications.
Additional facts
Generalized periodontitis is diffuse damage to the periodontal complex, covering most or all teeth. Generalized periodontitis is one of the most complex and still unresolved problems of clinical dentistry. Periodontitis, especially its generalized form, is 5-6 times more likely than caries, leading to partial and complete secondary adentia, and long-term persistence of infection in periodontal pockets is a risk factor for the development of rheumatoid arthritis, infective endocarditis, atherosclerosis, myocardial infarction, stroke, etc. . The term “periodontium” refers to a complex of periodontal tissues that have a common innervation and blood supply and are closely related to each other in morphological and functional terms. The periodontal complex is formed by the gum, periodontium, bone tissue of the alveolar processes, cement of the roots of the teeth and performs the most important functions - support-retaining, protective, reflex. Periodontal pathology includes gingivitis, periodontitis, periodontal disease, and tumor-like processes (periodontomas). When widespread dystrophic-inflammatory changes occur in the entire complex of periodontal tissues, they speak of generalized periodontitis.
Generalized periodontitis