Stomatitis is an inflammatory disease that affects the oral area, resulting in erosions, blisters and ulcers appearing on the mucous membrane. Over time, the symptoms become more pronounced and cause severe discomfort.
In medicine, there is more than one form of stomatitis, and each of them has its own symptoms.
Stomatitis on the cheeks is one of the common forms of the disease, the primary symptoms of which are ulcers, white plaque, pain and inflammation at the location of the sores in the mouth. Stomatitis is often diagnosed in children, although it also often develops in adults.
Stomatitis of the oral mucosa is not uncommon, but for treatment to be successful and adequate to the situation, correct diagnosis is necessary, which is often difficult. This is due to the fact that similar symptoms can also occur as a result of other pathologies.
What causes the development of stomatitis on the cheeks?
Stomatitis ulcers and sores can appear in absolutely anyone; they are localized on the cheeks and other mucous membranes of the oral cavity. There is a certain risk group that includes:
- people diagnosed with gastrointestinal diseases;
- patients with drug or food allergies;
- asthmatics (we are talking about bronchial asthma);
- women in the age category from 50 to 55 years;
- patients with a history of Quincke's edema.
The disease manifests itself for various reasons, we note the most common:
- inflammation of an infectious nature;
- mucosal injury;
- effects on the mucous membrane of alkalis and acids;
- decreased immunity due to treatment of a recent disease (the use of antibacterial agents, antibiotics, glucocorticoids and cytostatics weakens the body’s protective functions) or during pregnancy;
- sexually transmitted diseases - HIV;
- neglect of hygiene rules;
- malocclusion;
- bad habits;
- contact with a person diagnosed with stomatitis;
- metabolic disease;
- dysbacteriosis;
- incorrectly formulated diet.
Treatment of bacterial stomatitis
If, due to stomatitis, the cheek is swollen and ulcers appear in the oral cavity, antibiotics and anti-inflammatory drugs are prescribed. In principle, the treatment regimen is the same as for other types of disease. If tissue necrosis occurs, surgical intervention is necessary, after which the doctor prescribes the necessary treatment. Immunostimulants play an important role - they help cope with the disease much faster.
Forms of the disease - definition by symptoms
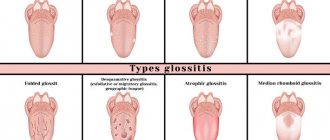
Experts identify 6 types of stomatitis, each of which can develop on the inside of the cheeks. Each form has characteristic symptoms:
- Traumatic , it causes redness and inflammation of the mucous membrane, erosion and sores that bring discomfort, white plaque on the cheeks, sore throat and mouth.
- Candidiasis, also called thrush, is characterized by a curd-like coating, blisters, pain and a feeling of weakness.
- Aphthous - ulcers appear that are red in color and round in shape. Edema also appears, a gray coating under which the epithelium dies, followed by the formation of a compaction-infiltrate, rejection of necrotic tissue and healing of aphthae.
- Herpetic . This form is characterized by the formation of blisters, in the area of which there is constant itching, later they turn into ulcers and aphthae, a feeling of malaise appears, and body temperature rises.
- The allergic form manifests itself in the form of redness, ulcers and inflammation appear on the cheeks, palate and lips, the plaque is often purulent. In addition, bleeding, fever, malaise and general weakness appear, as well as symptoms inherent in the aphthous form.
- Bacterial is accompanied by a light coating (yellow or gray) or erysipelas with blisters and bleeding.
The photo shows a sore on the inside of the cheek, characteristic of aphthous stomatitis
General clinical picture
With stomatitis, ulcers and wounds appear on the cheek from inside the mouth, which are covered with a white coating. Almost always, the disease affects not only the cheeks, but also the tongue, palate, tonsils and the inside of the lips.
Regardless of the form of the disease, there are symptoms that are inherent in each type of stomatitis:
- round ulcers appear on the mucous membrane;
- a white or gray coating is inherent;
- redness and swelling in the affected area;
- painful sensations.
Diseases with similar symptoms
Mouth ulcers and white plaque on the cheeks can be a sign not only of stomatitis, but also of other diseases:
- mucosal tuberculosis;
- syphilis;
- acute necrotizing gingivostomatitis.
Often, such a reaction is observed with irritation of the mucous membrane, excessive consumption of sugar, use of inappropriate dental equipment, stress, injury, lack of vitamins, folic acid or iron in the body.
Traditional and folk medicine for the treatment of disease
The effectiveness of treatment depends on timely response and diagnosis of the disease. The most favorable prognosis is when treating a mild form of pathology. There are times when the use of special medications is not required. So, if bacterial stomatitis is diagnosed, then antibacterial, antiviral and antifungal agents are used, as well as drugs that increase immunity, due to the fact that restoration of the body’s protective functions speeds up the treatment process.
Before starting treatment, it is necessary to establish the reasons why stomatitis ulcers, plaque and other symptoms characteristic of the disease appeared on the cheeks. It is the analysis of the causes that makes it possible to diagnose the form of pathology and use appropriate methods of therapy suitable for each specific case. Only the attending physician should draw up a course of treatment and prescribe the dosage of drugs.
A set of measures that is used to treat stomatitis in the area of the mucous membranes of the oral cavity:
- oral administration of medications;
- use of rinses, compresses and ointments for local treatment;
- use of laser therapy.
Initially, the patient needs to undergo an examination and pass the appropriate tests. If a bacterial form of stomatitis is diagnosed, then treatment includes the use of antibiotics, antiallergic drugs, as well as drugs that restore microflora and probiotics.
Treatment of stomatitis of viral origin occurs by enriching the body with vitamins; the use of antiviral and immunomodulatory drugs is necessary.
All drugs used for treatment should be prescribed only by an appropriate specialist, who should also set their dosage.
To treat sores on the cheeks, medications in the form of a spray (Bioparox, Proposol, Ingalipt) can be used.
In addition, Penicillin, Cefazolin, Grammidin, Amoxiclav and Cephalosporin are often used. Also, to alleviate the condition, not only antibiotics are needed, but also medications that have an antiviral and wound-healing effect (Methyluracil ointment, Chlorhexidine, Solcoseryl), which can be used to treat wounds and ulcers inside the oral cavity.
Today, laser therapy has become quite popular. The effectiveness of the method allows you to see the result as quickly as possible. The principle of the technology is to target the affected area with a laser beam. In addition, the ulcers are disinfected without affecting the healthy tissue on the cheek.
As a result of using this method of therapy, nerve endings in the affected tissues are eliminated, and this helps to avoid the occurrence of pain. There are no contraindications to the use of a laser, so treatment can be performed this way almost always.
In addition to traditional medicine, you can use other treatment methods that are available for use at home:
- It is imperative to rinse with solutions based on antibacterial herbs;
- It is recommended to apply compresses to the affected areas of the mucous membrane;
- It is also necessary to enrich the body with vitamins by consuming fruits or herbal preparations (for their preparation it is best to use calendula, sage, chamomile and sea buckthorn).
Many experts recommend using folk recipes to speed up the healing process of ulcers. Alternative medicine involves the use of medicinal compresses based on garlic and potatoes, a mixture of honey and carrot juice. You can also use baking soda for compresses. It can also be used as a mouth rinse.
Stomatitis ulcers on the cheek can be removed using folk remedies:
Preventive actions
To prevent the development of stomatitis, as well as to avoid relapses in the future, you must adhere to certain rules:
- It is necessary to contact a specialist if there is damage to the teeth: chipped enamel, crown fractures, sharp edges, and others. Such injuries can lead to injury to the mucous membrane by the sharp edges of the incisors.
- Daily brushing of teeth is required; in no case should you skip the procedure during pregnancy and adolescence. In this case, you need to use not only toothpaste and a brush, but also dental floss.
- When using braces, all protruding parts must be covered with special wax so as not to injure the mucous membranes from the structural elements.
- Nutrition should be reconsidered. At the same time, you need to stop eating foods that can cause allergies, because often they become the cause of stomatitis. In addition, nutrition must be balanced (the body must be enriched with all necessary nutrients) and timely.
- Experts recommend avoiding stressful situations.
Consequences of the disease
Stomatitis causes terrible discomfort when eating, which results in weight loss. If we are talking about small patients, this can cause inhibition of physical development.
A serious consequence of the pathology is the progression of stomatitis into a chronic form, which is aggravated by the addition of a secondary infection.
Despite the fact that in general the prognosis is quite favorable, if treatment is not started in time, diseases such as leukemia, diabetes mellitus and others can develop. Therefore, it is better not to put off the treatment of the disease, but if symptoms appear, immediately contact a specialized specialist.
Stomatitis is a common disease of the oral mucosa and occurs in 20% of people on the globe, having a variety of forms. The inflammatory process in the mucous membrane of the mouth, on the lips, tongue and cheeks is a kind of protective reaction of the body to a pathogenic irritant.
Several generations ago, this disease was common among children, but today it is often diagnosed in adults. Stomatitis on the inside of the cheek can be either an independent disease or a symptom of another disease, such as flu, pharyngitis, sore throat, etc.
Stomatitis is very diverse in its development and types, which is explained by many different reasons that can cause it. If you want, you can identify a number of main reasons why the disease most often occurs independently and develops:
- Infection of the body with pathogenic microorganisms , which causes inflammation in the oral mucosa, which in turn causes the appearance of ulcers and the formation of plaque.
- Poor nutrition , due to which the body does not receive much needed vitamins and microelements, which causes a weakening of the immune system and, as a result, leads to the development of diseases.
- Injuries to the oral cavity , both one-time and permanently inflicted in one place on the cheek. Various factors can cause injury:
- mechanical damage to the mucous membrane through a bite, scratch or constant exposure to improperly installed orthodontic devices;
- chemical damage to the mucous membrane as a result of an imbalance in the acid-base balance or exposure to an aggressive chemical.
- Insufficient care for oral hygiene .
- Smoking and drinking alcohol.
Aphthous stomatitis often forms on the cheek
But stomatitis cannot always be caused by reasons that are easy to eliminate. In some cases, when it is a symptom of another disease , it may turn out that a completely different part of the body should be treated.
There are a number of diseases or procedures to cure them that can cause stomatitis in the mouth on the cheek as a side effect:
- the disease may be a consequence of negative oncological changes in the body and may be a sign of tumor development in neighboring tissues;
- chemotherapy and radiotherapy for cancerous tumors can affect the condition of the oral cavity, cause erosion and ulceration, which ultimately leads to the formation of stomatitis;
- diseases of the gastrointestinal tract can have a negative effect on the oral mucosa and cause ulcerative lesions of the oral cavity;
- large blood loss , severe dehydration and fever can also cause stomatitis on the cheek (see photo);
- Pregnancy can also be a factor in the development of the disease, since while carrying a child, a woman’s hormonal levels change and the level of immunity decreases.
Can stomatitis cause your cheek to swell? This is quite likely. Ulcerative lesions of the oral mucosa, and especially the cheeks, are usually not difficult to notice, so if symptoms of disease appear, you should visit a dentist as soon as possible.
With stomatitis on the cheek, it can become very swollen
Description
Have you ever encountered a similar phenomenon and don’t know what stomatitis looks like on the cheek? The photos used as illustrations for the article will help you form your own opinion about all the “beauty” of the disease. It’s not pleasant, I must say.
The disease manifests itself in the form of ulcers in the mouth, on the inside of the cheeks. It lasts up to fourteen days, after which it usually passes without leaving any traces. It is noteworthy that if the disease makes itself felt at least once, there is a high probability of relapses, the frequency of which is very variable. According to statistics, people turn to specialists with similar complaints three or four times a year. Some people are concerned about chronic stomatitis (in the mouth, on the cheek, on the mucous membrane of the lips), in which new ulcers appear when the old ones have not yet had time to heal. This disease is considered to be contagious, although it all depends on the causes of its occurrence.
Classification and symptoms
Stomatitis on the cheek in a child or an adult differs in the type of its manifestation and the course of the disease. Basically, the classification of stomatitis is based on the reasons why it developed.
- Traumatic. Appears as a result of injury to the oral mucosa. The injury can occur one time or repeatedly.
- Candida. A disease that appears primarily in childhood. The cause of this stomatitis is the active proliferation of a fungus from the genus Candida. The fungus itself can exist quietly in the human body, but begins to spread in the oral cavity as a result of a decrease in the level of immunity.
- Aphthous. Usually it is the body’s reaction to the appearance of foreign objects in the oral cavity. Ulcers of aphthous stomatitis most often form on the cheek.
- Herpetic. Based on the name, the cause of the disease is the herpes virus in the oral cavity. As a rule, even after successful treatment, the herpes virus does not completely disappear from the human body.
- Allergic . Ulcers and wounds appear as a result of the body's inflammatory response to a specific irritant.
- Bacterial . Stomatitis is the result of the proliferation of streptococci and staphylococci that have entered the oral cavity from outside.
Cheek stomatitis has many possible causes.
Depending on the specific type, the course of the disease may differ. But, one way or another, any type of stomatitis has common symptoms that serve as sufficient grounds for an early visit to the dentist :
- the cheek became swollen from stomatitis, and the mucous membrane began to turn red and hurt;
- purulent ulcers appeared on the infected stomatitis area;
- salivation increased significantly, the gums began to bleed, and an extremely unpleasant odor appeared from the mouth;
- The lymph nodes have noticeably increased in size, and the body falls into a feverish state, which is typical when the disease develops severely.
Stomatitis can easily spread from the affected cheek to the tongue, soft palate, lips and tonsils.
How to treat stomatitis on the cheek? If the disease is not yet in advanced stages and occurs in a relatively mild form, then treatment can be carried out without drug therapy .
However, if the cause of stomatitis is the activity of microorganisms, then various drugs are used in treatment:
- immune supporting agents;
- antifungal;
- antiviral;
- antibacterial.
Treatment of stomatitis on the cheek is carried out with medications
A doctor can prescribe the necessary treatment for stomatitis on the cheek only after making an accurate diagnosis , which includes determining the type of disease affecting the oral cavity.
Treatment is carried out mainly in the following ways:
- taking medications internally;
- use of rinses, sprays and ointments on the inside of the cheek;
- using a medical laser to remove ulcerative lesions of the mucous membrane.
A very wide range of medications can be used: antibiotics, immunomodulating, antiviral and antiallergic drugs, probiotics to restore healthy microflora and vitamin-containing preparations.
The increased popularity of laser therapy is explained by its accuracy, bloodlessness, painlessness and high level of precision, which allows you to quickly and accurately eliminate the symptoms of stomatitis on the cheek inside the mouth (see photo).
Stomatitis is a disease accompanied by inflammation of the mucous membranes of the mouth, incl. inner surface of the cheeks, pathology can develop in isolation or act as a marker of other ailments. The disease requires complex drug and local treatment, and with prolonged absence of therapy it can become chronic. Note that both children and adults are susceptible to stomatitis. If you notice the first signs of the disease, you should immediately consult a doctor; failure to comply with this condition may lead to negative consequences.
The mechanism of development of stomatitis has not yet been studied; there is a theory regarding the occurrence of inflammation inside the oral cavity against the background of atypical immune reactions to molecules unknown to the body.
Reasons for the development of stomatitis on the cheek:
- elderly age;
- unbalanced diet, deficiency of substances important for the body;
- diseases of infectious etiology resulting from the penetration of pathogenic microorganisms into the body;
- taking medications that have the side effect of slowing salivation. The same applies to long-term use of antibiotics. For more information about stomatitis from antibiotics, see further in the material;
- anemia;
- chemical, thermal, physical damage to the epithelial tissues of the cheeks;
- dehydration of the body due to non-compliance with the drinking regime, blood loss, vomiting, diarrhea, feverish conditions;
- smoking abuse;
- reduced immunity;
- heredity;
- cancer cells in the neck or nasopharynx;
- changes in the normal background during pregnancy and adolescence;
- errors in the manufacture and installation of implants and prostheses.
Stomatitis can also develop as a result of violation of hygiene standards in the process of oral care; the use of toothbrushes with hard bristles and the use of hygiene products containing sodium lauryl sulfate also have a negative impact.
Causes of pathology
Basically, stomatitis on the inside of the cheek is caused by the following factors.
- Pathogenic microorganisms. Ulcers occur at the site of penetration of bacteria, viruses, fungi and other harmful microorganisms into microcracks in the mucous membrane. In fact, opportunistic flora is always present inside a person’s mouth, but manifests itself only in the presence of favorable conditions (reduced immunity, damage to mucous tissues, exacerbation of systemic diseases, etc.).
- Diet. An unbalanced menu leads to a deficiency of vitamins, minerals and antioxidants, which increases the risk of microbial growth.
- Oral injuries. Any violation of the integrity of the mucous membrane (burn, rough food, hard bristles of a toothbrush, household item, tooth fragment, etc.) increases the risk of ulcer formation.
- Violation of hygiene rules. Insufficient care of teeth and gums, poor cleaning and processing of products, poor hand washing, etc. can also increase the risk of stomatitis on the cheek. Most often this cause is present in children.
- Dental manipulations. It has been noted that the disease develops more often in patients who have recently had braces, dentures, plates, mouth guards or implants installed.
- Taking medications. Some drugs (for example, diuretics) disrupt the natural microflora of the mucous membrane and lead to the proliferation of opportunistic microflora. They can also reduce salivation and increase dryness of the buccal mucosa, which will lead to the appearance of microcracks.
- Bad habits. Alcohol and smoking lead to disruption of tissue trophism, chemical and thermal burns of the mucous membrane, which reduces local immunity.
- Systemic diseases in acute and chronic form. Any diseases, especially those associated with ENT organs (tonsillitis, tonsillitis, etc.) lead to weakened immunity and an increased risk of secondary infection.
- Malignant processes of ENT organs . Often, patients with cancer pathologies develop stomatitis in parallel.
- Ionizing radiation, chemotherapy, radiation sickness. As a result of these processes, the immune system is greatly weakened and tissues become thinner; this is one of the causes of stomatitis in the mouth.
- Parasites. In rare cases, parasitic infestation in advanced form can also cause ulcers on mucous surfaces.
- Dehydration. Against the backdrop of a prolonged lack of fluid, the mucous membranes dry out, which provides soil for the proliferation of pathogens.
- HIV infections. In patients with HIV and AIDS, the risk of candidiasis, herpes and stomatitis increases significantly.
- Endocrine pathologies. When hormonal imbalances occur (including during pregnancy or menopause), ulcerative lesions occur more often. Pathology can also be triggered by treatment with aerosol hormonal drugs, for example, for bronchial asthma.
- Diabetes. People with an advanced form of the disease or poor compensation often develop a complication in the form of aphthous stomatitis.
- Anemia. Disturbances in blood flow and blood structure can also provoke autoimmune forms of stomatitis on the buccal mucosa.
Source: stomatita.ru
Varieties
There are the following types of stomatitis on the cheeks:
- candidal stomatitis - develops against a background of weakened immunity, after the elimination of symptoms, the herpes virus remains in the body and has the property of manifesting itself under suitable conditions;
- traumatic - occurs as a result of damage to the mucous membrane, wounds and ulcers appear as a result of an incorrect bite, the presence of sharp fragments of teeth in the oral cavity, or a diseased tooth. Find more information about the treatment of traumatic stomatitis here;
- aphthous - affects the body after penetration of a foreign object into the oral cavity, injuring the mucous membrane;
- herpetic - occurs against the background of herpes virus infection;
- allergic - caused by the development of a response against the background of exposure to various allergens;
- bacterial stomatitis - develops as a result of penetration of pathogenic bacteria into the body.
Stomatitis on the cheek is accompanied by painful and unpleasant symptoms; ulcers and small ulcers form on the inside of the cheeks, which can bleed. Redness and swelling appear on the affected areas, and a white coating often appears on the cheeks. The patient may also experience weakness, malaise, pain while eating; symptoms may differ slightly depending on the type of stomatitis.
Symptoms of stomatitis:
- herpetic - itchy blisters on the inside of the cheeks, general malaise, high fever. Read more information about the treatment of herpetic stomatitis in this article;
- traumatic - swelling and redness of the mucous membrane, erosive lesions on the inside of the cheeks, shallow tissue injuries;
- candidiasis - a removable whitish coating, redness and swelling, soreness, discomfort in the oral cavity, spread of inflammation over the entire area of the mucous membrane;
- aphthous - small reddish spots, grayish plaque on the tongue and cheeks, death of cells under the plaque, formation of dense infiltrates. Read more about the treatment of aphthous stomatitis here;
- allergic - redness of the mucous membrane, formation of ulcers with bleeding and suppuration, fatigue, fever;
- bacterial - small plaque on the cheeks, bursting and bleeding blisters, sepsis in severe stages of the disease.
If pathological symptoms occur, you should immediately consult a doctor, this will help avoid negative consequences in the future.
Symptoms
The disease in question is characterized by the formation of certain symptoms, and for each type they are unique.
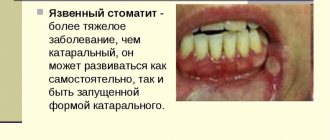
For example, when catarrhal stomatitis appears inside the body, ulcers or aphthae appear on the cheeks.
In a situation where a patient complains of slight swelling and redness of the mucous membrane, the formation of a whitish coating, then in such a situation experts talk about the formation of a similar type of disease.
Aphthae are round ulcers with a gray coating on top. Mostly they do not provoke any discomfort and do not cause unpleasant sensations to the patient, but if they recur, they are likely to scar, healing over a long period of time and causing deformation of the cheek.
With a complex course of the disease, the formation of ulcers is observed, causing a deterioration in the patient’s well-being, as well as leading to damage to the lower layers of tissue.
You should consult a doctor if the following symptoms occur:
- The formation of the pathological process will begin with the appearance of slight redness on the mucous membrane of the cheeks. Over time, a slight swelling will form near this area of tissue, the tissue itself will swell and become overly painful.
- In a situation where ordinary bacterial stomatitis appears inside the body, then a day later it is possible to see a small ulcer on this inflammatory focus, near which there is an inflamed halo of a reddish tint, and a thin white film is visible in the center.
- The formed ulcer provokes painful discomfort, complemented by increased salivation, bleeding in the gums and foul odor from the mouth.
- In acute cases of the pathological process, fever and enlarged lymph nodes are likely.
Often the location of the ulcers will be the cheeks, as well as the soft palate, tonsils, the surface of the tongue and the inside of the lips.
Diagnostics
The doctor conducts a general examination of the patient, studies the medical history, and conducts a visual examination of the oral cavity. Special tests and laboratory studies are not provided for the diagnosis of stomatitis; the whole process consists of visually determining the stage of the disease and identifying the cause of its occurrence. The medical opinion is formed on the basis of the symptoms indicated by the patient, the location of the ulcers, their shape and size.
Therapy for various forms of stomatitis should take an integrated approach; it includes certain procedures aimed at eliminating pain and discomfort. This will prevent further development of the disease and its transformation into a chronic form.
Drug treatment includes taking the following medications:
- antibiotics - Amoxiclav, Penicillin, Cefazolin, and Cephalosporin. Read more details about the selection of antibiotics for stomatitis further in the article;
- antifungal - Fluconazole, Diflazon, Clotrimazole, Diflucan, Nystatin ointment, Metronidazole;
- antiviral - Methyluracil ointment, Solcoseryl, Chlorhexidine - intended for treating ulcers from the inside;
- immunostimulants - their action is aimed at increasing the body's defenses; Immunal, Amiksin, Sodium Nucleinate, Imudon are widely used.
Therapy is prescribed after diagnosis and identification of the type of stomatitis on the cheek.
Causes of relapse of herpetic stomatitis
An acute reaction in a healthy body occurs once, then when the immune system is weakened, the virus manifests itself in the form of a disease such as chronic recurrent herpetic stomatitis.
Late diagnosis and treatment of periodontal tissue diseases can lead to tooth loss! Self-medication does not work! Contact PerioCenter specialists!
- 044 337-93-60
The following prerequisites for the occurrence of relapse of herpetic infection are identified:
- the effect of low temperatures on the body;
- acute infections;
- chronic pathologies in a state of decompensation;
- immunodeficiencies;
- taking significant amounts of antibiotics, corticosteroids, antitumor drugs;
- injuries, burns, congenital anomalies.
All of the above reasons contribute to a decrease in immunity. As a result of this, the virus begins to multiply in the nerve ganglia and infects other tissues. According to worldwide studies, about 12% of people experience relapses of herpes infection. In more than 2/3 of all cases, the first relapse occurs 10-12 months after acute herpes.
Home Remedies
The patient’s main task is to sanitize the oral cavity, which will help eliminate foci of inflammation as quickly as possible; at the next stage, it is recommended to strengthen the immune system, incl. with the help of diet. Antiseptic rinses for stomatitis in adults are recommended to be carried out at intervals of 5-6 times a day; chamomile decoction, oak bark, and sage show high effectiveness.
Recipes:
- Take 1 tbsp. chamomile, pour 0.5 liters of boiling water, leave for 10 minutes. on the fire, strain, the broth can be drunk throughout the day.
- 1 tsp Pour hydrogen peroxide into 0.5 tbsp. boiled water , use for rinsing 2 times a day, the product has analgesic properties.
- Mix 1 tsp. sage and oak bark, pour 0.5 liters of cold water , place in a water bath for 20 minutes. Dilute the strained mixture in equal proportions with boiled water and rinse for a week.
Compresses
For stomatitis on the cheeks, it is recommended to apply a cut aloe leaf to the ulcers 3 times a day. It is also recommended to lubricate the oral cavity with sea buckthorn oil and refrain from eating and drinking for an hour.
Dietary recommendations
Treatment of stomatitis should be carried out in any case, otherwise the disease can cause discomfort that can disturb the patient's condition.
Dietary recommendations:
- fermented milk products normalize the microflora of the stomach and can act as a stabilizer in strengthening the immune system;
- food should not be solid, hot or cold , preference should be given to liquid or semi-liquid food;
- exclusion from the diet of foods that can cause pain ; this category includes sour and spicy foods, fruits, citrus juices, carbonated drinks.
- giving up alcohol and smoking;
- complete exclusion of physical activity , overwork, and prolonged exposure to the cold.
Compliance with the listed rules will help to avoid complications and eliminate irritating effects on the oral mucosa.
Oral hygiene during treatment
Strict adherence to hygiene rules helps speed up the healing process, resulting in a reduced risk of re-infection. In case of stomatitis, it is necessary to carefully remove plaque, otherwise the inflammatory process will persist, which will lead to the progression of the microbial environment. The choice of toothpaste also plays an important role; all toothpastes containing the foaming agent sodium lauryl sulfate should be excluded. Contact of the substance with the mucous membrane is irritating and leads to dehydration. Toothpastes with flavors increase pain and should also be avoided. To brush your teeth, it is recommended to use products that contain only natural plant ingredients.
If symptoms of stomatitis appear, it is recommended to change your toothbrush; preference should be given to soft bristles with a massaging effect. Brushing your teeth should also be done twice a day, but be careful. After each meal, you need to rinse your mouth; this will help remove food debris; dental floss will also help.
Keeping your mouth clean will help reduce pain and irritation, resulting in improved overall health.
For more information about methods of eliminating herpetic stomatitis on the cheek, watch the video
https://youtube.com/watch?v=JTY70XTP3Yo
Source: bolvzhivote.ru