Much has been said about the effect of bad habits on the body. Smoking is usually associated with oral diseases and, in the long term, lung cancer. But the development of such a formidable disease requires time and smoking experience, but several months are enough for the development of nicotine stomatitis. MedAboutMe will tell you about the causes of stomatitis, its symptoms, treatment methods and consequences.
Stomatitis is a collective term that combines different types of inflammation of the mucous membrane. There can be a huge number of causes of inflammation: hormonal changes, fungi, bacteria, viruses, and much more.
Stomatitis can be caused by prolonged exposure to aggressive substances, for example, in patients in hazardous industries. By the way, workers at confectionery factories are at risk, even if it’s sickening to think about candy. But still, bad habits, namely tobacco smoking, are a powerful predisposing factor and cause of various stomatitis.
Nicotine stomatitis is a keratosis of the mucous membrane that develops as a result of systematic exposure of the mucous membrane to components of tobacco smoke or any other aggressive agents.
Keratosis refers to a violation of the process of keratinization of the epithelium - it thickens. The very name of stomatitis hides its main cause - nicotine, but is it the only thing that can provoke stomatitis?
Bad habits are not just smoking
The main causes of nicotine stomatitis are considered to be the negative effects of tobacco smoke substances, of which there are more than 400. Cigars and smoking pipes are considered especially dangerous in terms of the development of such changes in the mucous membrane. It has been proven that the longer the smoking history, the faster pronounced changes in the mucous membrane appear. The number of cigarettes smoked per day matters.
But not only smoking can be considered a bad habit responsible for changes in the mucous membrane. Stomatitis can develop in lovers of hot drinks, tea or food that continues to boil in a mug or plate. This love of hot food can also be considered a bad habit; many dentists and general practitioners advise gradually giving it up.
Symptoms of nicotine stomatitis
Changes in the mucous membrane develop gradually. At the initial stages, they do not cause any inconvenience to the patient and are often diagnosed by chance, during a preventive appointment.
The first symptoms of nicotine stomatitis will be a change in the color of the mucous membrane of the cheeks and palate. Brightly colored red-pink spots appear on a pale background. The spots develop into keratotic papules, at the top of which there are red dots corresponding to the ducts of the salivary glands. These are especially visible in the sky. Patients report that a rash has appeared on the roof of their mouth. Redness of the ducts is associated with their inflammation as a result of regular physical or chemical irritation.
The mucous membrane of the palate or cheeks gradually becomes cloudy and becomes grayish. The papules rise more and more above the mucous membrane and if they are located close to each other, they merge and form a pattern similar to the laying of paving stones.
Symptoms of nicotine stomatitis are associated not only with changes in the mucous membrane, but also with dysbiosis of the oral cavity. Disruption of microbial balance in the mouth occurs more often due to the negative effects of tobacco smoke components and decreased saliva production.
Oral dysbiosis can manifest itself with various symptoms, depending on the duration of its existence. Common ones include: the appearance of plaque on the teeth and tongue, changes in taste sensitivity, and bad breath. Against the background of dysbacteriosis of the oral cavity, stomatitis can become complicated: symptoms of a bacterial infection are added - the appearance of films from white to gray-yellow in color, unpleasant and even painful sensations, and when the plaque begins to disappear, eroded mucous membrane may be exposed.
Stomatitis can exist for a long time and be difficult to correct, because the only treatment is giving up bad habits. Considering the nature of the changes in the mucous membrane and the constant aggressive impact, some authors consider stomatitis as a factor in the increased risk of developing oral cancer. Other authors emphasize that for the process to become malignant, a number of provoking factors are necessary, namely smoking “with fire inside” (pipes, rolled-up cigarettes). But this does not eliminate the risk of oral cancer due to smoke containing carcinogenic substances.
Smoker's stomatitis - why is it dangerous?
To date, there is no consensus on the mechanism of development of nicotine stomatitis. Of course, the tars contained in tobacco smoke settle on the oral mucosa, one way or another provoking its irritation. In this case, the body’s immune response occurs and inflammation develops. However, stomatitis does not develop in all smokers - the effect of accompanying factors probably also plays a role: dietary habits (in particular, a love of spicy, sour, hot foods), drinking strong alcoholic beverages, taking certain medications, vitamin deficiency, and some allergic reactions. Stomatitis is promoted by improper or insufficient oral hygiene, incorrectly installed dentures, as well as the composition of saliva (increased tendency to form tartar). One of the important factors contributing to inflammation of the mucous membrane is an imbalance in the bacterial microflora of the oral cavity, and dysbiosis develops not only as a result of taking antibiotics or using antibacterial pastes and rinses for dental care. Tobacco smoke, which is full of toxins, itself contributes to the death of beneficial bacteria that inhabit the oral cavity.
Features of nicotine stomatitis
As a rule, inflammation of the oral cavity that develops as a result of regular smoking has its own characteristic features. In particular, usually the main focus of inflammation is located in the palate. This is explained simply: it is precisely this area of the oral mucosa that receives a stream of smoke when inhaling a cigarette. Inflammation develops not only due to the deposition of resins, but also as a result of exposure to fairly hot smoke. Over time, the body tries to defend itself - the normal epithelium at the site of chronic inflammation is replaced by denser and rougher, keratinizing epithelial tissue. However, such a protective reaction does not always have time to develop - often ulcers appear at the site of inflammation, which can be complicated by the addition of a bacterial infection. Inflammation can spread to the gum mucosa and affect the salivary glands. Smoker's stomatitis is not classified as a precancerous pathology, however, it should be remembered that nicotine and tobacco tars themselves have a carcinogenic effect, and regardless of whether or not there is chronic inflammation of the oral cavity, the likelihood of developing cancer due to smoking exists.
Smoker's stomatitis: what to do?
Some people consider stomatitis a natural accompaniment of smoking and are convinced that it does not need treatment. This is a dangerous misconception. Chronic inflammation, especially if it is complicated by ulcers, is an excellent breeding ground for pathogens and the development of complications. Therefore, nicotine stomatitis can and should be treated, and to treat it, use drugs that have an analgesic effect and relieve inflammation, and also destroy pathogens. Cholisal® has proven itself well . When applied topically, the main active ingredient choline salicylate is absorbed through the oral mucosa, providing local analgesic, anti-inflammatory and antipyretic effects. It also has antimicrobial and antifungal effects (in acidic and alkaline environments). Cetalkonium chloride is an antiseptic that acts on bacteria, as well as fungi and viruses. The gel adhesive base helps to retain the active substances on the mucous membrane. Cholisal® is a triple-action dental gel for the treatment of inflammatory diseases of the oral mucosa (gingivitis, periodontitis, stomatitis) as well as for relieving pain during teething in children. Helps relieve pain, helps relieve inflammation, acts on viruses, bacteria and fungi*.
However, it should be understood that the main cause of nicotine stomatitis is a harmful habit that must be abandoned in the name of the health of not only the oral cavity, but the entire body. Stopping exposure of the oral mucosa to tobacco smoke in combination with treatment with a drug with anti-inflammatory and antimicrobial effects will have a beneficial effect on the condition of the oral cavity.
* Instructions for medical use of the drug CHOLISAL®
How is nicotine stomatitis treated?
As many dentists say, treating nicotine stomatitis is not difficult, but patients do not agree with them. The main goal of treatment is to eliminate the traumatic agent, that is, quit smoking and refuse to eat anything hot. For some patients, such actions are difficult.
Only if you quit smoking, nicotine stomatitis is reversible, and literally after a few weeks the mucous membrane is restored, becomes pale pink, that is, returns to its original state.
Applications with substances that accelerate epithelization will help stimulate the recovery process: sea buckthorn oil, vitamin A oil solution and other drugs recommended by the dentist.
If it is impossible to give up a bad habit, then all treatment processes are aimed at eliminating the symptoms: strengthening oral hygiene, which will help fight stomatitis, anti-inflammatory therapy, vitamins, minerals and much more are prescribed. The main thing is regular examinations of the oral cavity, assessment of the condition of the mucous membrane and timely diagnosis of the malignancy of the process.
Take the test Take the test and find out how valuable your health is to you.
Rat diseases
Infectious stomatitis
This is a viral disease that occurs with inflammation of the mucous membrane of the mouth and tongue. Most often it affects young rabbits, and occasionally occurs in rats. Rabbit breeders often call this disease fox disease, or wet face, because infected animals begin to secrete copious amounts of saliva, and the entire front part of the body becomes wet. Most often, rabbits get sick, especially during the period of teeth change. There are many factors that provoke the occurrence of stomatitis. Among them:
- a sharp change in diet and feeding time, which can disrupt the already established functioning of the animal’s digestive organs; it also disrupts the reflex of eating at a certain time;
weakness of the body, unfavorable conditions for keeping the animal,
overcrowding, drafts, dampness and dirt in the cages;
inadequate food;
poor quality food;
food that has not undergone proper preparation;
complications after coccidiosis.
Usually the oral cavity contains bacteria that do not harm the animal. However, a weakened immune system, general loss of strength, constant irritation and damage to the mucous membrane of the mouth create conditions for infection. In such cases, seemingly harmless bacteria cause severe inflammatory processes, and sometimes even the death of the animal.
Symptoms.
A pet infected with infectious stomatitis develops ulcers on the gums and tongue, because of this the appetite immediately disappears, the animal drinks a lot and has difficulty chewing food, as a result it quickly loses weight and moves little. Excessive salivation, tongue ulcers, and exhaustion are observed. The animal's chin and neck are always wet, as if the animal had been immersed in water. A large amount of saliva also enters the stomach. This leads to indigestion, which results in diarrhea. The mucous membrane of the mouth and tongue of a sick animal becomes covered with a grayish coating. After 4-5 days, this plaque becomes brown or dark red and begins to peel off, and the gums swell.
Treatment
. Provided that the treatment was carried out on time and the animal was cared for well, infectious stomatitis in the initial stage, which is the most acute, can be cured quickly and easily. If the disease is started, it will lead in 2-3 days to complete depletion of the animal’s body. Animals with infectious stomatitis must be isolated. Give them foods that don't require much effort to chew. Salt and meat and bone meal are added to the feed. Various medications are used: a weak solution of copper sulfate, a solution of rivanol or potassium permanganate. These solutions should be used to irrigate the oral cavity of a sick animal. To do this, use a syringe or syringe without a needle. It needs to be inserted between the raised lip and cheek and the procedure is carried out. You can dip the animal's face into a freshly prepared heated solution. You can also wipe the animal’s oral cavity with a swab pre-moistened with a solution of penicillin (in the proportion of 200,000 units per 50 ml of water). Streptocide, sulfazine and other sulfonamide drugs can be given orally to your pet, 0.3 g per animal 2 times a day. A day or two after this, the secretion of saliva stops, the animal’s skin dries out and it begins to eat again. If the pet is very weak, it can be fed artificially. To do this, you need to lift his head, pull his cheek near the corner of his mouth and pour a little oatmeal jelly there. Another method of artificial feeding is the introduction of liquid food through a rubber tube with a diameter of 0.3-0.4 cm. A male urinary catheter is suitable for this purpose. This procedure can be carried out by the animal owner independently. After recovery, young rodents usually lag behind in growth compared to those that did not suffer from infectious stomatitis.
Prevention
. Successful prevention of this disease lies in the timely detection, isolation and subsequent treatment of infected animals. You need to monitor the feed: removing hard parts of sunflower, stalks and leaves of corn, which can injure the mucous membranes, spoiled, rotten, moldy, dust-, sand- or rust-covered feed helps prevent the occurrence of infectious stomatitis. Do not feed rodents frozen or sour food. Feeders and other equipment should be thoroughly washed daily with a hot solution of caustic soda, and periodically they should be treated with boiling water. Quarantine for newly acquired animals must last at least 1 month. Of decisive importance in the prevention of infectious stomatitis is strict adherence to the rules of animal hygiene, sanitary standards, and proper feeding, which can completely prevent the infection from entering the body of rodents.
Damage to the oral mucosa that occurs as a result of smoking is called nicotine stomatitis. Such damage occurs with prolonged exposure to toxic substances released from tobacco on the mucous membrane. The first manifestations of stomatitis are the appearance of areas of inflammation in the oral cavity, hardening of the mucous membrane, and roughness. The earlier such a disease is identified and treatment is started, the more favorable the prognosis, since in advanced cases the pathology can develop into cancer. Therefore, when the first signs of illness occur, you need to go to the hospital.
Treatment of aphthous stomatitis
Basically, the treatment is nonspecific and has the following goals:
- anesthesia;
- elimination of functional disorders by suppressing inflammatory reactions;
- reduction in relapse rates;
- reducing the risk of new ulcers.
Components of treatment:
- diet;
- topical rinses and lotions use products containing analgesics, anesthetics, antiseptics, anti-inflammatory drugs, steroids, sucralfate, tetracycline suspension, silver nitrate;
- When aphthous stomatitis is associated with systemic diseases, immunomodulators, antimetabolites, and alkylating agents are used strictly as prescribed by the doctor.
Damage to the oral mucosa that occurs as a result of smoking is called nicotine stomatitis. Such damage occurs with prolonged exposure to toxic substances released from tobacco on the mucous membrane. The first manifestations of stomatitis are the appearance of areas of inflammation in the oral cavity, hardening of the mucous membrane, and roughness. The earlier such a disease is identified and treatment is started, the more favorable the prognosis, since in advanced cases the pathology can develop into cancer. Therefore, when the first signs of illness occur, you need to go to the hospital.
Causes and symptoms of pathology
Long-term smoking is considered the main cause of the disease.
But there are also factors that provoke the appearance of stomatitis:
- failure to comply with hygiene rules;
- decrease in the body's defenses;
- dental diseases;
- dysbacteriosis;
- improperly equipped dentures;
- diseases of the stomach and intestines;
- frequent consumption of hot and spicy foods;
- consumption of alcoholic beverages;
- taking medications;
- infectious diseases of the oral cavity;
- allergy;
- insufficient intake of vitamins and minerals into the body.
Symptoms of stomatitis when smoking:
- foci of hardening of the epithelium;
- hyperemia of the mucous membrane;
- formation of white films;
- the appearance of white circles or stripes on the cheeks;
- inflammation and redness of the salivary glands;
- roughness of the affected areas.
General principles of treatment
Treatment of stomatitis in children under 1 year of age causes certain difficulties. Children are not able to fully comply with all recommendations for therapeutic effects. Many, not knowing what to do, resort to folk remedies. They, of course, help, but not always. For example, in no case should you lubricate the mucous membrane with a fungal infection with honey. This will only help the bacteria grow even stronger. A good method of exposure would be rinsing with decoctions of the following herbs:
- chamomile;
- calendula;
- sage;
- St. John's wort.
Decoctions of chamomile, calendula, sage and St. John's wort are excellent anti-inflammatory agents
In addition to all medications, when treating stomatitis in children, the famous doctor Komarovsky recommends drinking plenty of fluids. The more liquid a child drinks, the more he will excrete it, which means that various bacteria and viruses will be removed from the body. Large fluid intake increases the secretion of the salivary glands. This helps to better wash away pathogenic bacteria from the mucous membrane. From the video you will learn what Dr. Komarovsky advises when treating stomatitis in children.
Among medicines, the use of iodinol and miramistin is indicated for the treatment of stomatitis in children of almost any form. Iodinol is a molecular iodine. Its action is based on antiseptic properties. Polyvinyl alcohol introduced into the composition after application to the wound, for some time, protects the lesion with a kind of film. The drug must be diluted before use, approximately 5 drops per 50 ml. boiled warm water.
Miramistin is more suitable for the treatment of herpetic eruptions on the mucous membrane. It is available in the form of a spray, which makes it easier to use, especially in the treatment of stomatitis in children under 3 years of age. The drug is a topical antiseptic (instructions for use of Miramistin).
Miramistin is available in the form of a spray and is an effective treatment for stomatitis in children.
Another drug that has gained confidence in the treatment of many inflammatory diseases of the oral cavity is Tamtum Verde. It is a non-steroidal anti-inflammatory and antipyretic drug. For the treatment of stomatitis in children, Tamtum Verde is used mainly in the form of a spray.
Tantum Verde spray for topical use dosed 0.255 mg/dose (Angelini company)
Is it possible to smoke with stomatitis?
Cigarette smoke destroys the microflora of the oral cavity.
If stomatitis occurs from smoking, doctors recommend stopping smoking, since cigarette smoke acts as an irritant on the inflamed mucous layer of the oral cavity. When smoking, the damaged areas are burned and the microflora in the mouth is destroyed. This leads to prolonged healing and increases the risk of complications, as well as degeneration into a malignant version of the disease. Smoking also negatively affects the immune system, reducing it.
Aphthous stomatitis
Aphthous stomatitis is one of the most common lesions of the oral mucosa and is classified as follows.
- Simple aphthous stomatitis
(87% of all cases), in which from one to five ulcers (afts) are formed, the diameter of each lesion does not exceed 1 cm. These ulcers heal without scars within 7-10 days. - Complex aphthous stomatitis
(7-10% of all cases), in which the number of ulcers can reach 10, some with a diameter exceeding 1 cm. Ulcers can last up to 6 weeks, lead to discomfort when swallowing and the formation of extensive scars. The genitals and perianal area may also be affected. - Aphthous stomatitis herpetiformis
(7-10% of all cases) - simultaneously, from 10 to 100 ulcers with a diameter of 1-2 cm are formed, which merge into large areas of ulceration that does not heal for 7-10 days. This form of stomatitis superficially resembles stomatitis caused by a virus.
Treatment of pathology
If a person experiences the first signs of the disease, he needs to consult a specialist, undergo an examination and begin adequate treatment, since quitting smoking will not completely solve the problem that has arisen. When visiting the hospital, the doctor will listen to the patient’s complaints and conduct an examination. To clarify the diagnosis and exclude other diseases, the doctor will order special tests. For effective treatment, the specialist will prescribe medication and traditional medicine as an additional method.
- Definition
- Differential diagnosis
- Prevention
Etiology
Definition
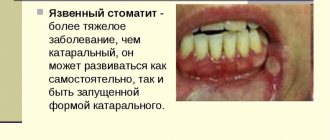
Nicotine stomatitis is an inflammation of the mucous membrane, characterized by the appearance of keratosis (keratinization), due to cigarette or pipe smoking.
It is localized in the area of the hard palate, sometimes on the buccal mucosa. Stomatitis is a disease caused by prolonged exposure to a negative factor.
The mechanism of damage goes in 2 directions: firstly, the presence of toxic elements in tobacco causes constant irritation of the mucous membrane, which leads to its change; secondly, toxins cause dysbiosis of the oral cavity (that is, a decrease in local immunity of the oral cavity), which now becomes a favorable environment for the further development of both stomatitis and many other pathologies.
Nicotine stomatitis is not a precancerous condition, but its symptoms are similar to those of malignant tumors. In addition, stomatitis often accompanies various forms of oral cancer.
Usually diagnosed in middle-aged and elderly men. However, with the advent of fashion for smoking hookahs and various exotic pipes, nicotine stomatitis is found in people under 30 years of age. Finally, there is an increase in the percentage of the disease among middle-aged women.
Etiology
The main reason for the development of nicotine stomatitis is smoking. As already noted, this addiction leads to a decrease in immunity and causes toxic elements to settle on the surface of the mucous membrane. It is also worth noting the adverse effect of hot smoke generated by smoking on the mucous membrane.
Finally, nicotine stomatitis can cause the development of other types of stomatitis. The disease is aggravated by alcohol intake, non-compliance with the principles of a healthy diet and work and rest regime.
Clinic
The initial stage of the disease is marked by the appearance of painless redness (erythema), which is diffuse in nature. Gradually, this area undergoes keratosis; the keratinized area has a grayish color. Keratosis acts as the body's defense mechanism against regular irritation. Then papules appear on the keratinized surface, having a depressed center of a reddish tint. These papules are an inflamed duct of the small salivary gland, which, due to the disease, significantly expands.
The progression of the disease is manifested by an increase in the number and size of papules. They do not merge into one and give the hard palate an uneven, bumpy surface. This symptom has acquired the name “cobblestone pavement.” Indeed, multiple papules of varying heights resemble a poorly laid, rocky road.
Harbingers of stomatitis are dry mouth, which smokers often complain about, and the appearance of bad breath for no apparent reason (no dental or digestive problems, regular oral hygiene).
Urgent care for stomatitis in a child
Can a child use the same medications as an adult when the disease has just been discovered? It is not for nothing that this issue stands apart, since the fight against the disease is different for children and adults. Despite the fact that mothers and fathers know which medications are effective, they are often afraid to give them to their children.
When antibiotics are used that are effective against a bacterial infection, such remedies will help both adults and children. For example, using Metrogyl-Dent for stomatitis will help get rid of the disease. Cholisal is also a good drug.
By using these medications at the primary stage of the disease, it is possible to eliminate painful sensations that often cause inconvenience to patients, interfere with normal communication and eating, and negatively affect dental and oral hygiene. Such medications are especially indicated for children, since it is difficult for them to tolerate pain.
In addition, the child’s diet should be enriched with useful elements, such as B vitamins, as well as iron-containing foods. You can find what you can eat if you have stomatitis on our website.
It is better to eat food in pureed form to avoid damage to the affected areas of the mucous membrane and palate.
Various teas help well - mint, chamomile, linden, calendula is perfect. All these remedies effectively rid the body of the spread of bacteria and viral infections.
Read about how to cure stomatitis in children at home.