Inflammation in the oral cavity in children is common and is always accompanied by pain. Stomatitis in infants is further complicated by the difficulty in implementing therapeutic measures and the inadmissibility of using many medications due to the patient’s age. It is still difficult for a child’s body to resist infection, since the defenses are not yet strong enough, and the baby’s curiosity forces him to taste everything.
What is stomatitis
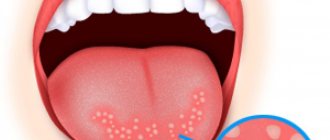
Stomatitis in infants is a disease characterized by an inflammatory process in the oral cavity. Stomatitis is localized on the inside of the cheeks, tongue, lips, and gums.
Blisters in a baby's mouth may appear immediately after birth. Infection occurs at the time of birth, when the child passes through the birth canal. The cause of stomatitis in newborns is the presence of a disease in the mother such as candidiasis (thrush).
The baby behaves restlessly and is capricious. There is redness in the mouth that bubbles and causes severe discomfort to the child. Such anxiety can lead to breast refusal due to pain.
Causes of stomatitis
May be caused by sores in the mouth and poor hygiene. For example, if a child had a wound in his mouth and he touches the wound during activity, he will easily bring dirt into it. As a result, stomatitis will appear. There is often redness around the stomatitis. If the sore comes into contact with anything, including food, it can cause severe pain.
Aphthous
May occur for no reason. Treated without intervention for up to 10 days. If the child notices obvious discomfort, then you need to resort to taking medications prescribed by the therapist.
Viral
Occurs due to a virus and may be accompanied by fever. The cause of viral stomatitis is reduced immunity and lack of vitamins. It is necessary to undergo an examination by a doctor who will prescribe medications and treatment.
Read, types of local anesthesia in dentistry. What are temporary suction cup dentures? The answer is in the article.
Oral candidiasis
The causes of thrush can be different. A common cause is prematurity and contact with an infected person. If a mother has thrush, it could be passed on to the baby.
Unlike stomatitis, candidiasis appears as large white patches that can be located not only in the mouth, but also on the genitals. If you notice that your child suddenly has a white coating all over his mouth, then he has candidiasis.
Thermal and chemical burns
You don't have to touch hot objects to get burned. Burns can be caused by food and medications that were consumed incorrectly.
The main thing for every parent to remember is that the same medicine that is suitable for an adult may be too heavy for a newborn. The mucous membrane can also be corroded by eating food that is too peppery or with the addition of a lot of seasonings.
Lack of vitamins
Lack of vitamins, in addition to white sores, can manifest as weakness and rashes on the body. If the child has been lethargic lately, and redness has appeared on the body, then examine the oral cavity. If you notice a white sore, then run to the doctor.
Classification of stomatitis
Stomatitis in infants is usually classified based on the causes of the disease. The following types of disease are distinguished:
- Fungal . This type occurs most often in children under three years of age. It is often called oral thrush. Mother's milk remaining in the mouth is an environment favorable for fungus. Externally, such stomatitis manifests itself in the form of a whitish coating.
- Herpes . Stomatitis caused by a herpetic virus. Most often it affects children aged one to three years.
- Mechanical . Appears as a result of injury.
- Allergic . This type of stomatitis in infants appears as a result of a reaction to an allergen, most often food.
- Aphthous . This species is less studied from an etiological point of view. The following factors are called that provoke aphthous stomatitis: hereditary predisposition, lack of vitamins, mechanical injury to the mucous membrane, including the palate.
The damaged part of the palate is colonized by pathogenic microorganisms, which leads to an inflammatory process. In a baby, this phenomenon can be caused by pacifier or finger sucking , as well as other mechanical damage. However, not every injury to the mucous membrane leads to stomatitis; the disease develops against the background of a weakened or still fragile immune system.
Where does the disease come from?
Inflammation is transmitted by airborne droplets or household contact, and may not be contagious (aphthous stomatitis). There are acute and chronic stomatitis in children.
Causes:
- herpes virus type 1 leads to damage to the oral mucosa;
- stress;
- deficiency of vitamins and minerals in the child’s body (especially iron, vitamin B 12 and folic acid);
- allergic diseases;
- decreased general immunity due to teething and colds;
- During childbirth, the child can become infected with a fungal disease from the mother (candidal stomatitis).
Often infants themselves spread the disease. This is due to the fact that children touch their mouths with their hands.
Inflammation of the eyes, ears and nasal cavity may occur. At the first signs, you should immediately begin sanitizing the inflamed areas on the tongue, cheeks and gums. Miramistin can act as an antiseptic.
Causes
Stomatitis is a fairly common disease in infants. There are a number of factors that cause stomatitis in infants.
Firstly, the mucous membrane of the oral cavity is extremely sensitive and is easily injured from mechanical, chemical or thermal influences. Secondly, infants have a very developed sucking reflex, which manifests itself in the desire to taste everything. This leads to the entry of pathogenic organisms into the oral cavity, as well as injuries to the mucous membrane.
Children's immunity is still in its infancy, and is not able to “repel” many pathogens of stomatitis . Saliva in newborns does not yet have the same disinfecting properties as in adults. Poor hygiene when feeding a child (poor handling of pacifiers, feeding bottles), including insufficient hygiene of the mother’s breast.
Diagnostics
If stomatitis is detected on the gums in children, treatment is carried out after diagnostic measures.
The parents’ task is to show the child to a specialist in a timely manner . It is an early visit to a doctor that will help quickly get rid of the disease. In most cases, diagnosis does not require the use of any complex procedures. The doctor only needs to examine the child’s cavity to determine the disease.
The examination will determine the severity of stomatitis, identify the area affected, and determine the nature of the disease.
Parents are also interviewed for a more accurate diagnosis. If there is any suspicion of a serious disease that has caused ulcers to appear on the gums, the doctor may prescribe the following diagnostic measures:
- donating blood for biochemical analysis;
- blood glucose test;
- immunogram;
- culture for sensitivity to antibacterial drugs;
- histological examination of the affected tissue;
- examination for the viral origin of the contents of the vesicle.
IMPORTANT: Only after a diagnosis has been established can treatment begin.
Symptoms
External manifestations of stomatitis in infants vary depending on the form of the disease.
Viral stomatitis
This form has several stages. Initially, in the absence of external signs of pathology, the baby may feel a burning sensation and itching in those areas where inflammation will later appear. The child's behavior becomes restless, the baby cries as if for no reason. The temperature may rise and lymph nodes may enlarge.
After the end of the incubation period, whitish blisters appear on the oral mucosa of the infant, which subsequently burst and leave ulcers with plaque. Such erosions can merge into one large wound and cause pain to the child. There is an increase in temperature within 38 degrees, in exceptional cases - even higher. There is an unpleasant odor from the mouth.
The baby refuses to eat, does not even take the mother's breast, since any sucking movements cause significant discomfort, the child often cries.
After healing of stomatitis erosions, there are no scars left on the mucous membrane , and the baby’s well-being improves. However, stomatitis is often accompanied by inflammation of the gums, which does not go away for several days after the symptoms of stomatitis have subsided.
Bacterial stomatitis
The symptoms of bacterial stomatitis in infants are very similar to the viral type of the disease . It is characterized by:
- darkish color of the oral mucosa;
- ulcers that can merge and form large areas of damage;
- the formation of yellowish crusts that stick together the lips;
- elevated temperature;
- bad breath;
- profuse salivation.
Diphtheria stomatitis in infants is characterized by the appearance of a film in the mouth , upon removal of which the inflamed surface bleeds.
Infection of a newborn baby with gonorrheal stomatitis is possible when passing through the birth canal. External symptoms - bright red color of the oral mucosa, lips, erosions do not merge, yellowish contents are released from them.
Aphthous stomatitis
The name of stomatitis speaks for itself - aphthae form in the mouth. These are inflammations that have a whitish or grayish color, a red border, and are very painful. This form is recurrent in nature, exacerbation occurs, as a rule, in the spring and autumn periods. Children aged 3-4 years are more susceptible to aphthous stomatitis.
In the absence of external manifestations, the baby complains of lethargy, he is capricious and irritable. Then aphthae appear, which have a rounded shape, covered with plaque. After the aphthae heals, there are no scars left, and the child’s well-being improves.
Fungal stomatitis
The cause of this disease in infants is often the use of antibacterial drugs, which destroy both pathogenic and beneficial flora. This situation can also arise when a nursing mother takes antibiotics.
External manifestations of fungal stomatitis in infants:
- white plaque in the mouth;
- elevated temperature (in severe disease);
- lethargy, moodiness, refusal of food, including breast milk;
- white coating on the tongue.
Types and causes of stomatitis in children's mouths
Stomatitis in a newborn baby's mouth occurs for various reasons. Depending on the location of the main localization of its manifestations, pediatricians understand which symptoms should be key in choosing the direction of treatment for the baby.
On the tongue
Rash on the tongue in the vast majority of cases occurs due to:
- Failure of the child to comply with basic rules of oral hygiene. In this case, we mean not only improper brushing of teeth, but also too often carried out measures to cleanse the oral cavity. If we are talking about a newborn, non-compliance with hygiene rules means imperfect cleaning of objects that enter the child’s mouth, for example, pacifiers, rattles, a “rodent”, and the mother’s breast.
- Lack of balanced nutrition. Applies to bottle-fed children. The lack of vitamins and nutrients contained in the infant formula leads to a weakening of the local immunity of the child’s mucous membranes.
- Taking a number of medications that negatively affect the mucous membranes of the newborn.
- Chronic diseases of internal organs. Such diseases may not appear at an early age and may not even be diagnosed, being in the stage of complete remission.
Considering that the baby cannot say or even point with gestures to the area in which he experiences the greatest discomfort, the only method for timely diagnosis of stomatitis is a daily examination of the child’s oral cavity by the parent.
When a pathological process begins, an adult will find:
- Increased body temperature of the child. At the same time, there are no secondary disturbances in the functioning of the body - the throat is not red, there is no runny nose, breathing is clear, blood and urine tests are normal.
- Sores on the affected area of the tongue. In some cases, before the formation of ulcers, numerous blisters form in the child’s mouth, reminiscent of the classic consequence of a burn.
- A white coating that usually covers the baby’s entire tongue completely or in chaotic spots of varying sizes. It is not possible to erase the plaque even by running your finger over it.
On the lips
Stomatitis, localized on the lips of a child, can occur in three forms: mild, moderate and severe (most often doctors deal with the mild and moderate stage of the disease, since in infants it is possible to diagnose the onset of the pathological process immediately after its onset).
The emergence of pathogenic microflora in a baby’s mouth can be recognized by characteristic symptoms:
- The child begins to sleep poorly. Children who previously slept all night begin to wake up every 2-3 hours, and those who periodically woke up their mother at night to give them food practically abandon the deep phase of sleep.
- The baby becomes restless. Unreasonable crying, nervousness, irritability, whims, and a constant desire to be in the mother’s arms appear.
- Decreased appetite. The child is less likely to breastfeed or does not eat his age-appropriate amount of formula.
- Increased salivation. A common sign of stomatitis, which is usually confused with the beginning of the process of teeth sinking into the “pockets” of the gums.
- Nausea , often developing into vomiting and frequent regurgitation. Regardless of food intake.
- Increased size of lymph nodes in the lower jaw area.
- Runny nose or cough . In rare cases.
This localization of stomatitis in the vast majority of cases is due to domestic and physiological causes of the disease.
For example:
- damage to mucous membranes by viruses;
- hypothermia;
- long-term insolation;
- the child is constantly in a stressful state (most often in this case the child transmits the emotional state of the mother);
- lack of nutrients (possibly due to incorrect selection of formula or unbalanced nutrition of a nursing mother);
- high dosages of antibacterial drugs;
- dangerous diseases of the respiratory system;
- infections (including those in remission).
On the gum
Stomatitis in a newborn baby's mouth can be localized on the gums. Most often, this type of disease occurs due to frequent contact of children's gums with dirty objects.
Other causes of stomatitis on the gums are:
- Injury to the mucous membrane. A child can damage the integrity of the skin by carelessly playing with a rattle or accidentally injuring himself with the nails of his fingers put in his mouth.
- Active reproduction of pathogenic microflora in the child’s mouth. Typically, the spread of bacteria and viruses occurs within 5-10 days. If during this period no measures are taken to stabilize the baby’s condition, stomatitis will acquire an acute form of its manifestation.
- An allergic reaction of the body to a specific irritant. The allergen may not be related to food.
- Diseases of the digestive system.
- Pathologies of the body's circulatory system.
- Hormonal imbalance. In infants, in the vast majority of cases, the imbalance is physiological and is a consequence of passage through the mother’s birth canal.
- Infectious diseases. Even those in remission.
Stomatitis on the gums can be recognized by the most common signs:
- numerous white sores;
- swelling of the gums;
- significant changes in the child’s behavior (increased number of whims, unreasonable crying, irritability, for example, with toys);
- sleep disorders;
- loss or decreased appetite;
- bleeding gums;
- light coating on the tongue and cheeks;
- crying of a newborn during feeding.
In the sky
Stomatitis on the palate is most difficult to diagnose by parents who have not encountered the disease in question before. Its advanced stage is manifested in the formation of a dense white coating over the entire area of the hard palate. The presence of plaque is not associated with food intake or the presence of procedures to keep the child's mouth clean.
At the initial stage, stomatitis, localized on the palate, can be recognized by:
- Increased body temperature. Temperatures can reach 40 degrees Celsius.
- Violation of the frequency of nutrition and drinking regime. The baby begins to eat less often or refuses food and water completely.
- Baby's anxiety during feeding. Eating is usually interrupted by the baby's crying or screaming for no reason.
- Presence of chills.
- Nausea progressing to vomiting.
- Numerous blisters or ulcers, most of them located in the affected area of the mucous membrane.
- Swelling of the mucous membrane. This provokes acute pain when the child tries to take a hard object in contact with the palate into the mouth.
The pathological process affects the roof of the child’s mouth for a number of objective reasons:
- the child often puts dirty toys in his mouth;
- a nursing mother does not observe basic hygiene rules in breast care;
- a newborn comes into contact with animals whose saliva touches the child’s lips;
- genetic predisposition of the body to the formation of ulcers on the body;
- weakened immune system;
- lack of nutrients (particularly iron and B vitamins);
- acute food allergy;
- progressive bacterial infection.
Treatment of stomatitis
Any treatment of stomatitis in infants should be carried out under the supervision and after consultation with a pediatrician. Therapy is prescribed taking into account the patient’s age, degree of neglect, and the condition of the child.
When treating stomatitis, regardless of the type and etiology of the disease, it is recommended:
- Following basic hygiene rules, processing baby toys and household items with which the newborn comes into contact. Mandatory breast hygiene for a nursing mother.
- Processing baby bottles, nipples, cutlery.
- Drinking enough. It is necessary to regularly offer your child warm drinks.
- If the baby has already begun to get acquainted with complementary feeding, the food must be of liquid consistency, not irritate the mucous membranes, and be of a moderate and comfortable temperature.
- If you refuse to eat and have no appetite, there is no need to insist and force-feed the baby, thereby causing severe discomfort to the baby. It is worth waiting and waiting for the condition to improve, then the baby will ask to eat.
- If you have started teaching your child about oral hygiene and he has started trying to brush his teeth, you should not give up this good habit, but after recovery you should change your toothbrush.
Mild forms of candidal disease
Treatment of stomatitis in newborns begins after examination by a pediatrician. At home, gentle medications and folk recipes are used, but a severe form requires more serious intervention.
For mild cases of candidal stomatitis in infants, use a soda solution, applying it to a piece of clean gauze. Gently wipe the damaged mucous membranes with your finger. The disinfecting properties of soda help remove up to 100% of all bacteria. Gradually the wounds dry out and the ulcers heal. But you cannot use baking soda alone, as it does not speed up the healing process.
It is prohibited to use brilliant green to treat stomatitis in infants, no matter what form the pathology belongs to. The baby's oral cavity is treated every 3 hours or after meals.
Chamomile infusion in water, prepared from 1 tbsp, relieves inflammation well. l. dry herbs and a glass of boiling water. It is advisable to prepare a fresh portion each time, but if necessary, the properties of the decoction can be stored in the refrigerator for 8-12 hours.
Remember! Disinfecting solutions - preferably chlorhexidine - are used to treat nipples, bottles and all baby toys.
If you skip the stage of preventive treatment of objects, the infection will begin to recur constantly. The use of antifungal agents is prescribed by a pediatrician.
Drug treatment
The following groups of drugs are used in drug therapy for stomatitis in infants.
Antiviral
This category of drugs is prescribed when stomatitis is caused by viruses. They inhibit the development of infection. When treating stomatitis in children under one year of age, the following local drugs are used:
- Oxolinic ointment . It is used 2-3 times a day and the affected areas are treated.
- Acyclovir . The drug is used 2-3 times a day, and the interval between treatments should be at least 8 hours.
- Terbofen ointment can be used up to 4 times a day.
Antifungal
Prescribed to infants when it is determined that the cause of the disease is a fungus. These are topical preparations; they are used to irrigate the main foci of the disease:
- Miramistin (in the form of a gel).
- Candidal solution.
- Nystatin drops.
- Aqueous suspension of levorin.
Painkillers
The use of drugs in this group does not solve the question of how to treat stomatitis in children under one year old; it helps relieve pain and improve the general condition of the baby. This group of drugs includes:
- Kamistad . The drug is available in gel form. For therapeutic purposes, the gel is applied to the affected areas three times a day. The drug can be used from three months of age.
- Propolis spray . Treatment is possible up to 5 times a day.
- In case of severe pain and high temperature, you can resort to the use of medications containing ibuprofen or paracetamol . They are available in the form of a suspension or suppositories.
Healing
Medicines in this group help to activate and accelerate the restoration processes of the oral mucosa in infants. These include:
- Solcoseryl ointment . Treatment is carried out after drying the mucous surface with a cotton swab, then ointment is applied and the areas are moistened with water. This procedure should be carried out up to 5 times a day, preferably after meals, and always at night.
- Shostakovsky Balm.
Disinfectants
For these purposes, preparations are used in the form of rinses . If the child cannot rinse his mouth himself, you can use a syringe or syringe without a needle. To do this, the antiseptic solution is carefully poured into the mouth, holding the baby face down over the container. Manipulations should be carried out every three hours.
Treatment of fungal stomatitis in a child
To overcome fungal stomatitis in children, the doctor will need to join forces with the child’s parents.
- Remember that the baby must be taken to see a pediatrician. Because a white coating can form on the tongue not only with stomatitis, but also simply after breastfeeding. Therefore, it is important that the child is seen by an experienced doctor. If the doctor confirms that the child is suffering from fungal stomatitis, then the baby’s parents will need to boil all the baby’s toys, pacifiers, bottles and other things that the baby will be in constant contact with when they come home. The pacifier can be stored in a soda solution immediately before giving it to the baby. The baby's mother should wash her nipples and breasts with plain warm water before feeding. There is no need to use soap. It is better to use detergent for this. In order to bring the microflora of the child’s mucous membrane back to normal, you can also wipe the oral cavity with a one percent solution of baking soda. To do this, take boiled water, let it cool to room temperature, then add a little soda to it and mix well. Next, take a cotton swab and dip it in the baking soda solution, then gently wipe the child’s mouth.
- The doctor’s main task is to correctly make an accurate diagnosis; in some cases, it is necessary to take smears for this. The doctor also needs to prescribe topical fungicidal medications or drugs for oral administration in the required dosage. Remember that self-medication can lead to the most unfavorable consequences. You also need to keep in mind that you can rinse stomatitis with soda. It works well and quickly cures the symptoms of the disease.
Often, a doctor may prescribe treatment for candidal stomatitis with a 20% solution of borax in glycerin or a 2% solution of boric acid. Gels, oils are also used, as well as spraying the mucous membrane with drugs that contain substances such as clotrimazole, nitamycin, nystatin, amphotericin B and levrin. An excellent remedy is also the Candida solution (which can be taken even by infants) and Diflucan.
Candida solution for stomatitis helps against mold and other fungi that can cause stomatitis. The exact dosage for treatment can only be determined by a doctor.
Typically, treatment procedures should be performed five or six times a day for 1-1.5 weeks. If improvements become noticeable earlier, then you should not rush to stop treatment altogether until the full course for recovery of the body has been completed. To speed up the recovery of the mucous membrane, it is recommended to use sea buckthorn oil or oil with vitamin A.
Sea buckthorn oil for stomatitis is a folk remedy that relieves inflammation and has bactericidal properties.
Candidal stomatitis in children is best treated with complex remedies. The mother of the baby must not only help her baby overcome the disease, but also undergo examination and, if necessary, treatment. In addition to using various antifungal drugs and treating formations in the oral cavity, children should also take vitamin complexes, strengthen the immune system in various ways and restore intestinal microflora.
It is also worth remembering that a child over one year old can be prescribed ointments against childhood stomatitis.
Treatment with folk remedies
Therapy with traditional medicine should be carried out only after prior consultation with a pediatrician. The following folk recipes have proven their effectiveness in treating stomatitis in infants:
- Soda solution . The product has an antiseptic and drying effect. A spoonful of soda is diluted with a glass of boiled water and the affected areas are treated.
- Chamomile decoction . Effective due to its disinfecting effect. A tablespoon of dry plant is infused in a glass of boiled water. The resulting decoction is rinsed using a syringe or syringe. The same solution can be prepared from dry calendula petals.
- Potato . To treat wounds, you can use either grated potatoes or a piece of vegetable.
- Onion broth . For it, dry husks, previously crushed, are used. For half a liter of decoction, three teaspoons of husk are needed. After the broth boils, it is infused overnight, then used as a rinse.
- Aloe . The plant can be given to an older child to chew. When treating stomatitis in an infant, aloe pulp is applied to the affected areas.
- A solution of blue or brilliant green will dry and disinfect the wounds. To do this, the affected areas are treated daily with cotton swabs.
The main task in the treatment of stomatitis in infants is to identify the causative agent of the disease; the choice of therapeutic measures and prescribed drugs depends on this. For treatment to be effective, it is important to eliminate the factors that provoked the disease.
Treatment
Treatment during pregnancy
This issue must be taken seriously. With extreme caution at all times and any prescriptions should be made only by an experienced specialist, since some drugs can harm the child. The medications prescribed by the doctor must be more effective than the possible harm to the fetus. The choice of method directly depends on the cause of the disease.
You can compensate for the lack of vitamins and certain elements by eating meat, fruits and fish more often. Or taking special vitamin and mineral complexes.
An important aspect of the treatment of mouth ulcers in pregnant women is nutritional adjustments.
- Bacterial stomatitis. Treat with antibiotics such as Amoxicillin, Erythromycin, Metronidazole, Oftoloxacin or drugs based on chlorhexidine digluconate.
- Fungal form. Antifungal drugs are prescribed that are safe for the fetus, with the exception of some contraindications.
- Viral stomatitis. Antiviral drugs are prescribed. Since most of them are unsafe for children, you should be especially careful when choosing a medicine.
- Allergic reaction. It is necessary to eliminate contact with the allergen. To do this, you must first determine it by analysis or exclusion. When treating this form of the disease, antihistamines and antiseptic solutions are used.
Treatment during lactation
Doctors recommend treating stomatitis during lactation with traditional methods, since medications directly reach the baby through the milk of a nursing woman and can harm the baby. The most common and effective method of combating stomatitis during lactation is rinsing using the following means:
- Soda solution followed by treatment of the oral cavity with Lugol's solution and glycerin.
- A solution of “Rotokan” in water (1:2), followed by lubrication of mouth ulcers with undiluted preparation.
- Alcohol tincture of propolis (15-20 drops per glass of warm water).
- Aqueous solutions with aloe juice. It is also acceptable to use pure plant juice by applying directly to the wound.
- Furacilin solution. One crushed tablet must be dissolved in a glass of warm water.
- Hydrogen peroxide (teaspoon per glass of water).
- Freshly squeezed carrot juice diluted with water.
- Medicinal herbs (calendula, chamomile). A tablespoon of dry herb is poured into a glass of boiling water and left for 30 minutes.
It should be noted that sea buckthorn oil has decent antibacterial properties due to the content of vitamins A and E, which promote the regeneration of the skin and mucous membranes. This product is safe during breastfeeding.
During the course of the disease during lactation, it is necessary to follow a gentle diet that excludes solid foods, foods and drinks containing irritants. These foods can include sweet, savory foods and citrus fruits. But the diet of a nursing mother must be balanced so that the child receives the substances he needs.
To avoid infecting a child with stomatitis, a nursing mother must take maximum precautions during feeding when breastfeeding. To do this, it is necessary to exclude the mother from contaminating dishes, pacifiers, toys and other objects that may come into contact with the baby’s oral mucosa. Here we should not forget that kids are inquisitive and get to know an object by tasting it.
To protect yourself from infection while pregnant and breastfeeding, you need to follow simple rules.