Oral health problems can affect absolutely everyone; both adults and children can suffer from infections in this area. One of the most unpleasant ailments is bacterial stomatitis, the occurrence of which is provoked by microbes of the genus streptococcus or staphylococcus. Once on the mucous membrane, they begin to actively reproduce, which leads to the formation of ulcers. The disease can occur in catarrhal and ulcerative-necrotic forms. Let us consider in more detail the features of identifying and eliminating bacterial stomatitis.
Description of the disease
Bacterial stomatitis is a disease of the oral cavity, which is accompanied by an inflammatory process and erosions with pus. The disease can appear due to bacteria that, when entering a certain environment, turn into pathogenic ones. In addition, some experts argue that stomatitis can develop due to microorganisms entering cracks and microscopic wounds. If the mucous membrane is not damaged, the risk of illness is minimal. Read more about whether stomatitis is contagious here.
The most favorable soil for the proliferation of pathogenic microorganisms is a weakened immune system.
It is important to start treatment on time, otherwise the disease progresses to a more severe, necrotic stage, fraught with tissue death.
Reviews
Reviews about the treatment of bacterial stomatitis have a positive trend, since most patients quickly got rid of the disease if they followed the instructions for the prescribed therapy.
In my case, bacterial stomatitis began to develop against the background of an incorrectly treated tooth. The infection did not make itself felt for a long time, and as the toothache intensified, ulcers appeared in the mouth. After visiting the dentist, I was prescribed various rinses and antibiotics. I want to say that I recovered quite quickly, but for this I rinsed my mouth very often and took pills on a schedule.
Marina
Our stomatitis appeared at a very young age. I couldn’t even imagine that this illness would cause such trouble. The child did not eat or sleep normally for a week until the wounds began to heal. I made compresses with hydrogen peroxide and gave a lot of fluids. After about 3 days, improvements became noticeable. Now I carefully make sure that the baby does not put her hands in her mouth and try to strengthen her immune system.
Natalia
Symptoms
Based on the state of the immune system, bacterial stomatitis can be short-term or long-term, turning into a necrotic (severe) stage not only with an inflammatory process, but also with purulent formations.
The main symptoms of bacterial stomatitis are:
- painful sensations while eating (especially for sour and spicy foods: marinades, sauces, citrus fruits, fruits, drinks, etc.);
- obvious swelling of a dark shade;
- itching, burning, possible appearance of ulcers and blisters on the inside of the lower lip, cracks;
- profuse salivation;
- strong unpleasant odor of acid from the mouth.
With bacterial stomatitis, a weakened immune system can give symptoms of general malaise - high fever, pain in the head and joints, loss of strength, intoxication, and a severe form of bacterial stomatitis can lead to a severe form of sepsis.
Bacterial stomatitis is often accompanied by bleeding gums, the tissues of which become swollen and loose if left untreated. In addition, the spread of the inflammatory process to the tonsils and nasopharynx can lead to sore throat.
Bacterial stomatitis causes severe discomfort when opening the mouth, and makes eating and talking painful.
If bacterial stomatitis is started, long-healing ulcers can form, which appear on the hard palate and, when tissue decomposes, lead to bone exposure. This symptom can be observed with Vincent's ulcerative-necrotizing stomatitis, the provoking bacterium of which is the spindle-shaped rod and Vincent's spirochete.
Types of bacterial stomatitis with photos
Bacterial stomatitis is a lesion of the oral mucosa, which is caused by bacterial pathogens: streptococci and staphylococci. These microorganisms are found almost everywhere (in the air, on household items, etc.), and are contained in the human body within normal limits.
Depending on the agent, the course of the disease will be different. In some cases, the disease passes quickly and does not have a detrimental effect on the general condition, in others there are accompanying symptoms. You can see what bacterial stomatitis looks like in the photo (see also: what does different types of stomatitis look like in children?).
| Type of stomatitis | Pathogen | Location of the lesion | general characteristics |
| Impetiginous | Streptococcus, but later staphylococci also appear | Gum | Mostly, children under 3 years of age suffer from bacterial stomatitis. Ulcers covered with a grayish coating form on the mucous membrane. Its removal is accompanied by bleeding |
| Erysipelas | Stomatitis is caused by streptococcal microorganisms | Mucous membranes (cheeks, gums, tongue) | Initially, swelling appears, after which reddish spots form, which are soon replaced by ulcers and blisters. The patient suffers from high fever, and overall health deteriorates greatly. Therapy must be started immediately, as sepsis may develop (mainly with a purulent course) |
| Sticking on the lips (we recommend reading: sticking in the corners of the lips in children: causes and treatment) | Streptococci and staphylococci | Corners of the lips (we recommend reading: why do cracks appear in the corners of the lips and how to deal with them?) | An ulcer appears on the affected area, which itches and bleeds with sudden movements (damage) |
Kinds
The degree of tissue damage can divide stomatitis into 2 types:
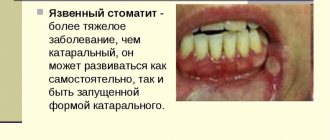
- superficial (catarrhal stomatitis) is characterized by symptoms of intoxication in the form of decreased appetite and increased body temperature. In addition, the patient experiences discomfort during chewing and swallowing food and increased salivation. Examination of the oral cavity shows a white coating on the tongue (there are distinct marks from the teeth on the lateral surfaces), bleeding gums, and hyperemia of the oral mucosa. In case of untimely provision of medical care or in its absence, the disease may progress to a more severe stage;
- deep (ulcerative-necrotic). The condition is significantly worsening. Signs of intoxication become stronger: headache, high temperature, sleep and appetite disturbances, lethargy, irritability, weakness. In addition, there is pain when chewing, an unpleasant odor from the mouth, and increased salivation. A medical examination shows bleeding gums, hyperemia of the mucous membrane, ulcerative formations with a grayish coating, fraught with subsequent tissue decay.
Stomatitis in children
Viral stomatitis
One of the most common contagious species. After the incubation period is completed, blisters form on the oral mucosa. Within a few hours they burst, turning into round or oval ulcers.
It is easy to “recognize” viral stomatitis in children: by its perfectly even shape and characteristic yellow coating on areas of erosion. Single spots often combine into larger lesions. The palate, tongue, and cheeks are inflamed and have a crimson-red tint.
Acute herpetic stomatitis
The second most common is herpetic stomatitis in children, the symptoms of which are the same as those of viral stomatitis. The onset of the disease resembles the flu: high temperature (up to 41°), aches, headache and muscle pain, enlarged lymph nodes.
First, a scattering of small bubble formations becomes noticeable (there can be quite a lot of them, up to twenty). They are grouped on the palatine arch, tongue, cheeks, and sometimes on the skin - near the lips and nose. The mucous membranes swell, the gums are also red and inflamed. In place of the burst bubbles, single or merged areas of erosion are formed, quickly becoming covered with a yellowish or whitish coating.
Recovery is long, from 10 days to two weeks. As a rule, infants who have reached six months of life and small children under three years of age become ill. During this period, the natural protection against the herpes virus obtained from the mother’s blood disappears.
Chronic herpetic stomatitis
Herpes is a virus that cannot be expelled from the body. Infection with it is also inevitable; in civilized countries, any person is a carrier of the infection. This is why herpetic stomatitis in a child with a weakened immune system periodically recurs. Provoking factors are colds, hypothermia, taking corticosteroid drugs, chronic tonsillitis, caries, microtrauma of the gums.
The external manifestation of the disease does not differ from the acute form of this type of stomatitis: the same blisters and ulcers. However, with a chronic course of the disease with periodic exacerbations, there is no acute period: there is no jump in temperature, the child remains active, although the lymph nodes enlarge.
Chronic aphthous stomatitis in children
The disease often develops against the background of food or drug allergies, so children with identified allergopathology are at risk. The treatment of stomatitis in children with this feature is also carried out together with the dentist by an allergist, and sometimes by a gastroenterologist.
Outwardly it manifests itself as the formation of painful round lesions covered with a dense grayish coating - aft. All aphthae have a clear shape and a bright rim. They are much larger in size than ulcers: they can reach 5-10 mm.
Unlike herpetic manifestations, with aphthous stomatitis the rise in temperature is slight, although there is weakness, the gums do not swell or redden. Aphthae are few in number (sometimes one lesion appears on the tongue or under the tongue, on the cheek), touching them causes severe pain.
The disease is provoked by staphylococcus, a microbe that lives in carious teeth and dental (soft) plaque. The disease appears more often if the child has congenital, acute or acquired pathology of the gastrointestinal tract, or some kind of immune disorder.
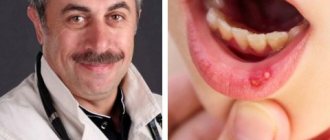
Bacterial stomatitis
Painful areas of bacterial stomatitis are small in size, uneven, and covered with a dense yellow coating. Sometimes yellowish dense crusts form on the baby’s lips, there is a clear putrid smell of breath, and drooling occurs. Mucous membranes are inflamed, dark or purple-red. It can be seen that the gums are loose and bleeding. The general condition also suffers: there are complaints of aches, headaches, and nausea.
Bacterial stomatitis in children is caused by staphylococcal and streptococcal bacteria. Treatment must be specific, fast and correct.
Candidal stomatitis
Candida fungi cause this type of disease that affects newborns. A characteristic sign of the disease is the formation of a cheesy, homogeneous milky coating over the entire area of the tongue and cheeks, on the gums, and sometimes on the lips. If this layer is removed, a painful, bleeding ulcer will be exposed.
A characteristic sign is the appearance of a sour odor from the infant’s breath. The baby does not take the breast and bottle and is capricious.
General approaches to the treatment of childhood stomatitis
Depending on the type of stomatitis in children, treatment will vary significantly. Nevertheless, there are general principles, the observance of which will alleviate the baby’s condition and will not aggravate the course of the disease.
- Careful oral care is necessary: antiseptic rinsing before and after meals, mandatory but careful brushing of teeth with a brush with the softest bristles. Infants can wipe the inside of their cheeks with a special napkin soaked in an antiseptic composition.
- Food for a sick child should be warm, so as to cause as little pain as possible when chewing. Spicy, sour, irritating mucous membranes and solid foods are prohibited. Purees, broths, and pureed porridge are preferred. Whole milk and juices should be excluded for a while.
- On the recommendation of a doctor, you can apply an anesthetic gel or spray to the gums and mucous membranes before meals.
- To recover faster, your baby needs to drink plenty of fluids.
The dishes of a sick child should be kept separately and carefully handled, especially if there are other children in the house. It is important to provide him with a separate towel and toys. If a newborn is sick, nursing mothers should definitely take care of the cleanliness of their breasts, nipples, and bottles.
The most important point, common to all types of disease, is not only timely and correct, but also sufficient treatment. This means that even with significant relief of the condition, you need to complete the course of taking medications prescribed by your doctor. If treatment is interrupted earlier, pathogenic pathogens will form a persistent defense against drugs, and it will become difficult to fight them.
Treatment of acute and chronic herpetic stomatitis
The acute form is treated with antiviral drugs that are effective against herpes. If the disease has become chronic, then additional immunomodulatory drugs will be required. To relieve the first acute symptoms, the doctor will prescribe an antipyretic, but only if the temperature is above 38.5°. At a lower temperature, you need to give the baby’s immune system the opportunity to work - the immunity will be stronger.
The main drug used to combat viruses in the oral cavity in dental and pediatric practice is Acyclovir. It successfully destroys herpes, but only at the first stage, when a vesicular rash forms. From the moment the ulcers form, ointments and gels are used for local treatment.
Viferon restores immunity well and destroys viral infection. Thanks to interferons and a vitamin complex in its composition, it quickly alleviates the condition of a sick child, especially if used in the first hours of illness. Available in convenient forms: candles are suitable for newborns and one-year-old babies, gel and for older children.
The third mandatory component of the treatment of stomatitis in children is frequent antiseptic rinsing. It is important that only the drug that is active against herpes viral infection will work. Miramistin is usually prescribed. There is no point in rinsing your mouth with herbal infusion.
It is good to treat ulcerated areas with Cholisal gel, which both heals and relieves pain for several hours. Sea buckthorn oil, Aekol, and wild rose (rose hip) oil have a strong healing effect. They are used topically, applied to the mucous membrane.
If the disease returns, that is, becomes chronic, then immunomodulatory drugs are included in the treatment regimen. You cannot use them on your own or violate the recommendations of the instructions: this is fraught not with an increase, but with an even greater decrease in immunity. Effective immunomodulators, for example, Immunal, Imudon, Amiksin.
Additionally, special pastes enriched with enzymes will enhance immunity in the mucosal area.
Causes
There are several reasons that can provoke a bacterial infection:
- Injuries to the mucous membrane when visiting the dentist, so pathogenic bacteria enter through the resulting wounds. More information about the treatment of traumatic stomatitis below.
- Advanced form of caries.
- Contact with an infected person.
- Use of utensils and hygiene products for oral care belonging to a patient with stomatitis.
Diagnostics
Diagnosis of bacterial stomatitis is based on an initial examination by a dentist and identification of characteristic signs of stomatitis. To determine the causative agent of infection, the following studies can be carried out:
- Tank culture of a smear taken from the oral cavity;
- PCR analysis;
- Complete blood test to study changes in basic indicators.
By identifying the exact cause of the resulting inflammation, it is possible to correctly prescribe the necessary medications and quickly heal the damaged oral mucosa.
Treatment
Self-treatment for bacterial stomatitis is excluded, since it is necessary to accurately identify the pathogen and, based on this, determine the appropriate medications to suppress its activity. Testing for bacteria is carried out in laboratory conditions. This procedure is extremely important, especially for children. To exclude possible complications, parents should promptly contact a specialist if there is swelling or an inflamed scratch.
The treatment procedure for bacterial stomatitis usually includes:
- antiseptics. The initial stage of the disease and its middle requires the use of rinsing solutions (Chlorhexidine for stomatitis) and disinfection of the oral cavity using gels with anti-inflammatory and analgesic properties. After the acute symptoms have passed, treatment continues with epithelial agents, which provoke faster healing.
- immunostimulants. Their need is to strengthen the immune system and prevent new outbreaks of the disease. The drugs are divided into general and local medications. In addition, a course of vitamins may be prescribed to maintain the general condition of the body.
- antibiotics. The prescription of these drugs occurs when the disease becomes more severe or the cause of the disease is chronic diseases of the internal organs. The most effective remedies in this case are ointments, the component of which is an antibiotic. The result is guaranteed to be positive if the cause of stomatitis is a coccal infection. For internal use, the following drugs can be distinguished: kanamycin, gentamicin, penicillin, lincomycin, etc. Read more about antibiotics for stomatitis here.
When necrosis develops, the dead tissue is removed by the surgeon, after which a complete sanitation of the oral cavity is carried out.
Along with drug treatment, the patient must follow a diet. During this period, you should take gentle food, limit your carbohydrate intake and enrich your diet with proteins and vitamins.
Treatment and prevention of disease
Doctors prescribe proven medications for the successful treatment of bacterial stomatitis:
- To get rid of the manifestations of the disease, it is recommended to treat the affected areas by treating them with special ointments and solutions. A list of medications will be given by an experienced doctor, taking into account the type of stomatitis and the individual characteristics of the patient’s body.
- Antiseptics like Furacilin and Rivanol are effective. They need to rinse the mouth every 3 hours.
- During the extinction of the disease, some medications can be replaced or supplemented with keratoplastic medications - vitamins A, group B. Sea buckthorn oil, aloe, and kalanchoe are used to treat tissues. Rosehip oil, which contains many vitamins, is also effective.
- Additionally, it is recommended to take immunomodulators (for example, Amiksin or Immunal) to increase the body's resistance.
- Treatment of bacterial stomatitis requires the use of the following groups of medications: antiseptics, antibiotics and anesthetics.
Regular adherence to simple hygiene rules will save you from the need to treat stomatitis. Be sure to brush your teeth in the mornings and evenings. In addition, you should forget about drinking large amounts of alcohol and smoking cigarettes. This is especially true for those people who suffer from a chronic form of the disease - giving up bad habits will help speed up the treatment of the disease. It is important to visit the dentist more often in order to prevent relapses. It is advisable to eat natural foods that do not cause allergies. Eliminate processed foods and fast food from your daily diet.
Complications
If timely treatment is not undertaken, bacterial stomatitis can lead to a serious complication that is very difficult to cure. A severe form of stomatitis is fraught with an increase in temperature to 40 degrees and above, which is not amenable to antipyretic medications.
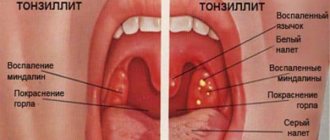
The patient suffers from constant headaches. Pathogenic microorganisms move to the tonsils, resulting in the development of a sore throat or bacterial tonsillitis.
Severe and rare forms of bacterial stomatitis are characterized by exposure of bone tissue in the area of the hard palate. Usually the complicated form is caused by Vincent's spirochete or spindle-shaped rod.
Reasons for education
First of all, this is poor oral hygiene and the presence of chronic diseases caused by bacteria. A concomitant disease, which results in impaired salivary secretion, can also contribute to the development of such stomatitis. Saliva is a natural disinfectant of the oral cavity, and if its composition changes and its quantity decreases greatly, such changes contribute to the rapid proliferation of bacteria and complicate the course of stomatitis.
Another cause of the disease is infection in the injured area of the mucous membrane. The injury can be very minor, resulting from an accidentally bitten cheek, burnt gums, or even a child’s erupting tooth. Often the injury can be chronic. For example, such damage to soft tissues occurs due to an incorrectly manufactured prosthesis, which constantly rubs and irritates the gums.
Previously suffered tonsillitis, otitis, and bronchitis also contribute to the development of bacterial stomatitis. In addition, this disease may also occur in people who often suffer from even simple acute respiratory infections.
Normally, the human body contains a large number of harmful and beneficial bacteria. If a person is healthy, then the pathogenic bacteria simply “sleep” and do not cause him any harm, but as soon as the immune system is weakened as a result of illness, stress, hypothermia, injury or other serious external influences, the pathogenic microflora begins to actively multiply and cause concomitant diseases. One of these bacteria is Fusobacterium necroforum, the result of whose active life is an acute form of bacterial stomatitis, namely ulcerative necrotic (Vincent).
Timely tests at the initial stage will help the attending physician identify the type of pathogenic bacterium that caused the erosion, determine its sensitivity to antibiotics and prescribe appropriate treatment.
Prevention
By following a number of simple measures, you can avoid such troubles as bacterial stomatitis. The rules must be followed both during illness and as a preventive measure. Let's look at them in more detail:
- Proper diet.
- Regular oral hygiene.
- Avoiding contact with a carrier of the disease.
- Clean hands.
- No scratches in the oral cavity.
- Professional treatment of the oral cavity.
If you are nevertheless overtaken by bacterial stomatitis, there is no need to be afraid, since the mucous membrane has rapid tissue regeneration. The main measure in this case will be to contact your treating specialist and strictly follow all his recommendations. More information about treating stomatitis at home in this article.
Folk remedies
Traditional medicine in the treatment of bacterial stomatitis gives the desired effect with the correct selection of the necessary antiseptics. The most effective recipes:
- Using alcohol tincture of calendula to rinse the mouth in a ratio with water (1:10). The finished product has pronounced anti-inflammatory and healing properties;
- St. John's wort tincture is also effective as a rinse. The dosage is 30 drops per 1 glass of water. The procedure must be carried out several times a day;
- Making a tincture of sage leaves is especially effective in treating bacterial stomatitis. 1 tbsp. Brew a spoonful of the plant in 250 ml of boiling water and rinse the mouth 3-4 times a day;
- A solution of soda with iodine disinfects well and promotes rapid healing of the mucous membrane. The proportion is 1 teaspoon of iodine and soda per glass of water;
- A decoction of oak bark in a ratio of 20 grams per 500 ml of water. Rinse the mouth well with the prepared product several times a day;
- Kalanchoe juice has a high healing ability in the treatment of bacterial stomatitis. It is used when applying compresses to formed ulcers in the mouth. You can also use an alcohol tincture with a plant extract;
- Eucalyptus leaves contain a considerable number of antiseptic substances, therefore they have a beneficial effect on the healing process of the mucous membrane. Preparation consists of pouring 20 grams of the plant with 500 ml of boiling water and infusing for several hours. The finished product is diluted in a ratio of 1:10 and rinsed 2-4 times a day;
- An oil solution of eucalyptus is diluted with water and also used to rinse the mouth;
- The use of alcohol tincture of propolis, since this substance has a large number of beneficial properties and helps restore the mucous membrane in bacterial stomatitis. A diluted solution in a ratio with water (1:10) is used for rinsing procedures.
Symptoms and treatment of bacterial stomatitis
The most common type of stomatitis, an inflammatory process that develops in the oral cavity, is bacterial stomatitis. This type of pathology occurs due to pathogenic bacteria, for example, streptococci or staphylococci, which penetrate into the smallest wounds in the oral cavity. The harmful microorganisms in question can be said to be “ubiquitous”, so stomatitis caused by bacteria is diagnosed in both adults and children, and even in newborn babies who are still in the maternity hospital.
Bacteria recognized as causative agents of stomatitis are considered in medicine as opportunistic pathogens, since microorganisms live in every human body. If a person’s immune system is normal and chronic diseases do not bother them, then both adults and children should not be afraid of the disease. But as soon as the body weakens or a wound forms in the oral cavity, harmful microorganisms will immediately make themselves felt by rapid reproduction, which will cause the development of bacterial stomatitis.
The analyzed disease can manifest itself against the background of the following diseases:
- deep caries;
- periodontitis or gingivitis;
- tonsillitis;
- laryngitis or rhinitis.
However, not only internal bacteria can cause the development of an inflammatory process in the mouth; quite often microorganisms enter wounds, as they say, from the outside, due to the following reasons:
- as consequences of inflammation that develops on the skin of the face, most often in the corners of the lips;
- when an infection occurs in dentistry, during dental treatment;
- if food products, in particular vegetables or fruits, are consumed unwashed;
- in close contact with an infected person, for example, during a kiss.
Under such circumstances, only streptococci initially begin to develop in the patient’s body, and then, if treatment is not applied in a timely manner, a staphylococcal foreign agent will join them.
Characteristic symptoms
You can understand the development of the disease being analyzed by the following characteristic symptoms:
- It becomes painful to eat certain foods, for example, spicy, sour or salty foods.
- The surface of the oral mucosa takes on a bright red tint.
- Swelling appears on the mucous membrane, and ulcers subsequently form.
- The patient begins to be bothered by a burning sensation and itching in the oral cavity.
- Salivation increases several times.
- An unpleasant and one might even say pungent odor appears from the mouth.
As bacterial stomatitis develops, the gums begin to hurt and bleed. The pain gradually intensifies, so even dental hygiene cannot be done painlessly.
Quite often, the victim of the disease begins to be bothered by frequent headaches, the body temperature may rise, and weakness is felt throughout the body. If a harmful bacterium spreads its harmful effects to the tonsils and the surface of the nasopharynx, this fact will provoke the development of a sore throat.