Etiology (reasons for formation) sticking in the corners of the mouth
The causative agents of angular cheilitis are streptococci (streptococcal infection) or yeast-like fungi of the genus Candida (candidomycotic infection), however, accompanying factors are also needed for the formation of infection.
In most cases, such factors are vitamin deficiency of B vitamins, skin maceration or diabetes mellitus, which reduce the body's resistance to skin infections.
A rarer, but no less important cause of angular cheilitis is the formation of folds at the corners of the mouth. The reason for the formation of folds may be the loss of muscle tone in old age or a decrease in the bite, which in turn can be the result of both the absence and pathological wear of teeth. This can also be caused by improperly manufactured orthopedic structures.
Treatment methods
Treatment of cheilitis depends on the form and stage of the disease and the patient’s skin. Doctors of various specialties can treat this disease: dermatologists, allergists, dentists. After clarifying the diagnosis, a treatment regimen is prescribed, consisting of the use of :
- B vitamins and minerals.
- Various gels for external use.
- Tablets and injections for systemic treatment.
- Physiotherapeutic procedures.
- Drugs and methods of alternative medicine.
The main efforts in the treatment of cheilitis are aimed at eliminating the cause that provoked the disease.
So for cheilitis:
- Exfoliative , psychotropic medications are prescribed: Sibazon, Phenazepam or Thioridazine. The lips are also treated with a special nourishing cream Spermaceti, rosehip oils or retinol. The exudative form of the pathology is treated with corticosteroid ointments: Prednisolone, Hydrocortisol, and boron-vaseline. Acupuncture and Bucca rays are considered effective.
- For angular, antibacterial therapy is carried out using Erythromycin and Furacilin ointments. Antifungal Nystatin ointment, creams containing retinol and zinc compounds are also prescribed. B vitamins are taken orally.
- For candidiasis, local antifungal therapy is carried out using Clotrimazole ointments, antibacterial solutions of Nystatin or Natamycin. Antiseptics Chlorhexidine or Hexetidine are recommended.
- In meteorological cases, the emphasis is on vitamin therapy and the use of nourishing creams or balms. The acute form of the pathology is treated with steroid ointments, and for daily use, the use of sunscreen is mandatory.
- For actinic , take the Delagil complex, B vitamins, Nicotinic acid, Prednisolone in small doses and external use of steroid and corticosteroid ointments: Advantan or Afloderm. A prerequisite for effective treatment is the use of Angelolis sunscreen ointment.
- For glandular at the initial stage, anti-inflammatory ointments are used: Naphthalene, Prednisolone, Hydrocortisone. The secondary form of cheilitis is treated by eliminating the provoking disease.
- In case of contact allergic form, the factors that caused the allergic reaction are eliminated. Drug therapy consists of the use of steroid ointments and antihistamines: Suprastin, Loratadine and others.
- For atopic, desensitizing therapy is carried out, in which antihistamines are taken: Fenkarol, Claritin, Diazolin. A protracted form of the pathology is treated with local application of ointments with corticosteroids.
- For eczematous, sedative and desensitizing drugs are prescribed. Local therapy consists of the use of ointments and aerosols containing corticosteroids. If eczema has a microbial etiology, therapy is supplemented with antimicrobial agents.
- For macrocheilitis, treatment consists of eliminating the cause of the disease. To directly combat cheilitis, corticosteroids are prescribed in combination with broad-spectrum antibacterial drugs. Antimalarial, antihistamine medications and vitamin complexes containing ascorbic acid and B vitamins are also taken.
Important! An effective auxiliary method for the conservative treatment of cheilitis of any type is physiotherapy and, in particular, laser therapy and electrophoresis with heparin ointment in combination with dimexide.
How to treat different types of cheilitis:
In advanced stages of cheilitis and to correct cosmetic defects, surgical treatment is performed. Laser excision is considered the most effective and less traumatic.
It is possible to use traditional methods in the treatment of cheilitis only after agreement with the attending physician. recipes for treatment at home are considered the most effective :
- For daily treatment of affected areas of the lips, oil solutions of retinol and tocopherol are used.
- A good moisturizing and nourishing effect is obtained from daily use of propolis pulp. It is applied to the lips for 30 minutes.
- A mixture of juices is prepared from the leaves of Kalanchoe, celandine, buttercup, plantain and garlic. Take them in equal proportions, mix and rub on sore lips.
- Use lotions made from marigolds. Prepare the decoction as follows:
10 grams of flowers are dipped in half a liter of boiling water and using a water bath, leave for ten minutes. Allow the liquid to cool and strain. Wet a napkin and apply it to your lips every half hour.
It is important to know that self-medication is unwise and harmful, since cheilitis has many forms and only a specialist can determine the type of disease and prescribe adequate treatment.
Clinic of angular cheilitis (jams)
Streptococcal seizures occur more often in children.
First, bubbles form in the corners of the mouth, covered with a thin layer of skin. After some time, the bubbles burst and in their place, crevice-like erosions (jams) form. After 1-2 hours, the jams become covered with a purulent-bloody crust, which, when removed, reveals a red, easily bleeding surface.
Streptococcal seizures are characterized by pain when moving the lips, as a result of which the patient often finds it difficult to speak or refuses to eat.
Candidomycotic seizures differ from streptococcal seizures in the absence of a crust. Instead, the erosion is covered with a grayish-white coating that is easily removed.
Often the jam is not visible when the mouth is closed, as it is masked by an overhanging fold of skin.
The most common reasons for jamming
The main reason why seizures begin to appear is a decrease in both general and local immunity (in the paranasal sinuses, oral cavity, upper respiratory tract, tonsils, nasopharynx), which creates favorable conditions for the activation of infection. But why immunity decreases is another question. This can happen for many reasons.
Factors that provoke the development of angulitis can be divided into two large groups:
- External.
- Internal.
- External factors include allergic reactions in women to the use of decorative cosmetics for the lips, incorrect bite (leading to microtraumas), exposure of wet lip skin to wind or cold. Very often, jams are formed due to excessive wetting of the corners of the lips with saliva. Such a favorable environment for opportunistic microorganisms gives them the opportunity to reproduce unhindered.
- Internal causes even more often become provocateurs for the development of angulitis. Lack of vitamins (especially B12) and minerals, rehabilitation period after illness, colds, HIV, diabetes, disturbances in the functioning of the digestive system, etc. Most often, binge eating begins to bother us in the spring, when the body really needs vitamin “support”. Also, people who take antibiotics or hormonal drugs are more susceptible to angulitis.
Read on our website:
What is ocular uveitis, symptoms of the disease
Often there is an impact of several factors at the same time, which is why the occurrence of jams is practically unavoidable.
For example, streptococcal angulitis most often develops for the following reasons:
- Insufficient oral and dental care.
- Habit of licking or biting lips.
- Skin contamination and lack of timely care.
- Diseases of teeth and gums.
- Incompetent approach in choosing braces or dentures.
- The skin of the lips is too dry, which provokes the appearance of microcracks.
- State of hypothermia or overheating.
If seizures bother you very often or do not go away for a long time, this is an alarming signal that something is wrong. Typically, relapses of angulitis are observed in cases of serious lack of immune strength. It is advisable to consult a doctor (perhaps more than one) to find out the cause of this phenomenon. Suddenly there is some serious disorder in the body or a disease develops that has not yet made itself felt too clearly. It is better to eliminate such a danger.
How to distinguish angulitis from other diseases
In order not to confuse angulitis with herpes (which, however, happens quite often), the best solution is to scrape the affected area of the skin or mucous membrane, and take a swab from the oral cavity. This diagnostic method will help differentiate the type of angulitis, since the treatment of streptococcal and candidal infections has significant differences . The doctor may also advise you to give urine and blood for a general analysis. If seizures are frequent “guests” of the patient, then it is better to consult with different specialists: an endocrinologist, an immunologist, a hematologist, or even an orthopedic dentist.
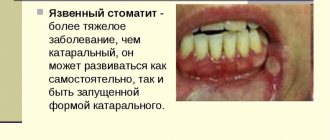
Photo of the manifestation of the disease
How to treat seizures using traditional methods
For treatment of seizures to be effective, an accurate diagnosis is first established based on the results obtained during research. Doctors will, of course, first prescribe medication. All drugs are selected for each patient individually, taking into account his condition, tolerability of certain drugs, and the form of the disease. The approach to treating angulitis should always be comprehensive, therefore the following methods are used:
- Local treatment of angular stomatitis.
For streptococcal angulitis, an ointment containing antibiotics (for example, erythromycin or syntomycin liniment) is prescribed. Vishnevsky ointment helps get rid of purulent discharge and promotes rapid healing of wounds.
If candidal angulitis is detected, levorin, sulfur-salicylic, nystatin or ointment containing fluconazole can be used to treat it . In addition to the fact that they eliminate the very cause of the disease (yeast-like fungus), with their help you can quickly relieve pain and speed up the regeneration process.
Before applying the ointment to the affected area of the skin, it must be wiped with antibacterial agents that contain alcohol.
- General treatment. The meaning of general treatment is exactly the same as the meaning of local treatment, namely, the impact on the source of infection through medications. To do this, the doctor prescribes medications to be taken orally. This can include both antifungal drugs and antibiotics (again, depending on the causative agent of angular stomatitis).
- Vitamin and mineral complexes. Since a common cause of seizures is a lack of nutrients in the body, it is necessary to undergo vitamin therapy along with local and general treatment. It is also advisable to take immunostimulant drugs that help increase the body's defenses. Pay attention to the article about probiotics, because... The health of your intestinal microflora is also important.
- Correction of diet. Vitamins and minerals should also be obtained from food. You definitely need to reconsider your diet and, if there is a shortage of those foods that contain a sufficient amount of riboflavin (B2) and vitamin E, be sure to add them. These include: egg yolk, nuts, legumes, bran, green leafy vegetables, oatmeal, corn, cabbage, vegetable oils, poultry. You need to lean more on fresh fruits and vegetables, dairy products. Along with this, the diet should not contain spicy, sour or too salty foods. If the cause of the seizure is candidal in nature, then you need to give up sweets, baked goods, and carbonated drinks. They not only have a bad effect on the condition of the body, but can also increase pain in the area affected by angulitis or even provoke the appearance of a new crack.
Read on our website:
28 ways to cure hemorrhoids at home
In parallel with the treatment of angulitis itself, it may be necessary to treat the disorder or disease that provokes the appearance of the seizure. For example, if a patient has diabetes mellitus or some other type of metabolic disorder, he must undergo treatment by an endocrinologist .
Additional diagnostics
If you go to the doctor with angulitis, then you should not be surprised that the doctor will write out directions for the child to undergo tests that rule out the presence of congenital or acquired syphilis in the baby.
The fact is that eczema with angular stomatitis is very similar to similar formations around the mouth with syphilis, differing only in the density of the formations. It is for this reason that additional tests for syphilis should not confuse and outrage moms and dads.
A thoughtful pediatrician will also give a referral for a biochemical blood test, which will allow you to see if the child has a significant deficiency of vitamins, in particular vitamin B.