Kinds
Let's look at the types of stomatitis in table form:
| Candida | Ulcerative | Allergic | Bacterial | Aphthous |
| The reason for this form is saprophytic fungi. Occurs during dysbacteriosis and decreased immunity. Young children, the elderly, and people with diabetes and immunodeficiency are especially vulnerable. The rash is accompanied by a white cheesy coating. | One of the most severe forms of stomatitis. The reasons are different - from mechanical damage to diseases of internal organs. The ulcers are painful, covered with a white coating. General health deteriorates significantly. | Occurs as an allergic reaction to food, medications, fillings, dentures, etc. Accompanied by swelling, inflammation, burning. | Infection occurs by different types of bacteria, including those that constantly live in the oral cavity. Since the oral cavity is usually immune to them, trauma or irritation of the mucous membrane is necessary for bacteria to penetrate. The ulcers are red, regular in shape, and the tissue is swollen. | It occurs most often as a result of infection with herpes viruses, as well as influenza, measles and other viruses. Aphthae are painful ulcers, from one to three, that cause severe pain when eating. |
Aphthous
Allergic
Bacterial
Candida
Ulcerative
Types of stomatitis
Doctors usually distinguish several types of the disease. The gradation is based on the reasons that caused its development.
Aphthous stomatitis
This is one of the most severe types of pathology. The aphthous form of inflammation is characterized by the formation of painful aphthae - ulcers reaching 3-5 mm in size. The disease typically has a chronic course, characterized by periods of remission and exacerbations.
Herpetic stomatitis
In this case, the culprit of the disease is the human herpes virus. Infection occurs by airborne droplets. Sometimes through direct contact with a carrier of the virus. The symptoms of the pathology in this case are as follows:
- abrupt onset, accompanied by a deterioration in general condition;
- increased body temperature;
- enlargement of submandibular nodes;
- swelling of the mucous membrane (initially) followed by the formation of painful erosions;
- increased salivation.
Fungal stomatitis
The cause of the disease is the Candida fungus. Most often diagnosed in childhood and old age. The main reason is a decrease in immune defense. Sometimes - long-term use of antibiotics.
The candidiasis form of the disease is manifested by the following symptoms:
- a person may experience a burning sensation in the mouth;
- a characteristic white coating forms on the palate, cheeks, inner surface of the lips and tongue (initially it is removed without any problems, but as the disease progresses, severe swelling and bleeding of the mucous membrane is observed);
- there is a loss of taste sensations.
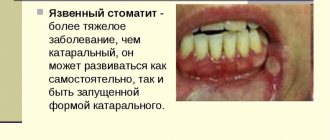
Ulcerative stomatitis
The most severe form of inflammation of the oral mucosa. The pain is significantly worse when talking and eating. The symptoms of the pathology are as follows:
- severe swelling and hyperemia of the mucous membrane;
- painful erosions can occur anywhere, with the exception of the palate and sublingual area;
- swelling and bleeding of the gingival papillae are observed;
- salivation increases;
- body temperature can rise to high levels;
- local lymph nodes enlarge.
Advice! Treatment of stomatitis in women during pregnancy requires special care, since there is a high probability of developing an allergic reaction to medications. That is why a preliminary consultation with a medical specialist is necessary.
Causes and provoking factors
Different types of stomatitis have different causes:
- Stomatitis can be a consequence of certain disorders in the body.
Infections. Infection occurs with viruses, bacteria and fungi, but they themselves do not provoke the onset of the disease. In order for a virus or bacteria to penetrate the mucous membrane, it must be damaged. In this case, infection complicates the course of the disease.
- Mechanical damage. The most common factor in the occurrence of stomatitis. You can damage the palate with solid foods - crackers, nuts, fish, poultry and meat with bones. This also includes burns. Medical manipulations can also injure the mucous membrane - for example, during dental treatment. Damaged covers become fertile ground for the penetration of bacteria and viruses.
- Poor nutrition. An unbalanced, poor diet often provokes the onset of the disease. Lack of vitamins A and C is especially dangerous; Group B; selenium, iron, zinc and other micro- and macroelements.
- Chronic diseases. Stomatitis can be a consequence of certain disorders in the body. Chronic diseases leading to decreased immunity, hormonal imbalances, and dehydration contribute to the appearance of ulcers. Their frequent occurrence is an alarming symptom that may indicate diseases such as cancer of the nasopharynx or neck, or immunodeficiency. It is worth undergoing a comprehensive examination.
- Allergy. Allergic stomatitis is a common type. Such a reaction can occur to food, medications, oral hygiene products (paste, mouthwash), new fillings or dentures, cosmetics - for example, lipstick. It is dangerous because it causes severe swelling of the tissues of the mouth and throat, which makes breathing difficult. If the allergen is not eliminated, angioedema may occur.
- Stress. Many patients suffering from frequent or chronic stomatitis note that exacerbation occurs in moments of mental or emotional stress, overwork, or severe stress.
- Bad habits. Smoking often leads to stomatitis. Smoke irritates the mucous membrane, which makes it vulnerable to viruses and bacteria. Alcohol abuse leads to the development of many diseases, weakens the immune system, and leads to a deficiency of important vitamins and elements in the body.
- Heredity. It has been noted that people whose parents also suffered from it are more often susceptible to this disease. Its occurrence in a child is also influenced by the mother’s lifestyle during pregnancy - nutrition, bad habits, hygiene, including the oral cavity.
- Hormonal changes. Pregnant women and people with diabetes are at risk. Also, stomatitis in women more often occurs on certain days of the menstrual cycle.
The risk of stomatitis in the upper, lower palate and uvula increases due to insufficient oral hygiene, abuse of too hot, spicy, and solid foods. Children can get sores due to dirty pacifiers, toys, or their own fingers in the mouth.
Supernumerary teeth, or what is hyperdontia, causes, symptoms, treatment methods
The normal number of teeth is considered to be 20 in the primary dentition and 32 in the permanent dentition. Occasionally, “extra” teeth are also discovered - they are usually called supernumerary, and such an anomaly is called hyperdentia (or hyperdontia). It occurs infrequently - it is only 2% of all deviations in the dental system, more often in men.
Hyperdontia
Features of supernumerary teeth:
Most often a single tooth occurs (about 70% of cases of hyperdentia), but two, three or more are also described. Cases with the identification of 2 or more supernumerary teeth must be distinguished from odontoma - this is a benign tumor built from dentin and enamel, which in its structure may contain many deformed tooth germs.
A case is described in which over 200 small enamel drops were removed from an odontoma, but by their nature such teeth are not supernumerary;
- The bite in which they are revealed
More often - about 2/3 of cases - in the replacement (during the period of replacement of milk teeth with permanent ones), in adults in the permanent dentition - ¼ of cases, and only occasionally are supernumerary teeth found in children in the milk dentition, this is less than 6% of cases;
This is what supernumerary teeth look like
- Location in the dental arch
Almost always this is the upper jaw - between the central incisors (mesiodens), in the area of lateral incisors and canines, and occasionally - next to the molars. In the lower jaw, supernumerary teeth are detected only in 3% of cases, in any part of the lower dental arch;
Correct eruption (appearing outward) is on the crest of the jaw arch in the dentition.
But in the case of hyperdentia, deviations are possible due to lack of space. Therefore, the direction of growth can be any - towards the palate, tongue, vestibular (outward). There are cases of deep burial in the thickness of the jaw, and eruption is impossible;
Anomalies such as spiky, chisel-shaped, triangular or lumpy deformities are not uncommon;
Symptoms in adults and children
The clinic of hyperdontia in adults is associated with inflammatory and degenerative changes in surrounding tissues:
- chronic injury and inflammation of the oral mucosa, gums and lips during chewing;
- impaired pronunciation of sounds and chewing due to improper closing of the jaws;
- inflammation and destruction of the roots of adjacent complete teeth;
- jaw pain;
- caries due to closer interdental contacts;
- prolonged runny nose, sinusitis (inflammation of the maxillary sinus) - when the roots of impacted teeth penetrate into the sinuses.
In children, in addition to these manifestations, the following may alert:
- delayed eruption of baby teeth;
- delay in the eruption of permanent teeth when the milk teeth have already fallen out;
- bite deformation;
- incorrect pronunciation of whistling, hissing sounds.
There are also frequent cases of asymptomatic disease, when a person may not feel discomfort in the oral cavity.
If supernumerary teeth do not interfere with chewing food, they are not removed
Dystopic and impacted supernumerary teeth
The origin of supernumerary teeth is already disrupted at the rudimentary stage, so they rarely grow correctly. Often their development is complicated by problems such as retention and dystopia.
The term retention (from the Latin word retentio - to linger) is what dentists call the delay or impossibility of teeth erupting. In a third of the detected cases, they lie deep in the jaw - horizontally, or with a turn towards the nose, maxillary sinuses, and even into the orbit. This type of filling makes cutting through impossible.
The term dystopia means deviation from the correct direction of growth. An extra tooth rarely has the opportunity to erupt in the dentition - the roots of other teeth interfere with this. As a result, it may move to the cheek or even to the palate.
Diagnostic methods
The first stage is a dentist’s examination of the oral cavity: gums, palate, processes and jaw arch. Already in this case, hyperdontia can be visually detected. When a tooth germ is retained, you can see redness and swelling at the location, as well as bulging of the jaw.
At the diagnostic stage, a panoramic image is taken
The “gold standard” is a panoramic image (or orthopantomogram, OPTG). This extra-oral x-ray examination is performed using a circular survey. This x-ray lasts 30 seconds and shows a complete picture of both jaws.
It happens that a two-dimensional X-ray is not enough - if the root is close to the wall of the sinus and it is unclear whether it penetrates into it, or the tooth itself is deep in the thickness of the bone. In such situations, three-dimensional imaging (3D imaging) is necessary and the dentist may prescribe a cone beam tomography (CBCT).
This is the same x-ray, but with a larger number of sections taken in 3 projections. The device also moves in an arc around the head, and the examination lasts no longer than a minute.
Should I delete it and when should I do it?
Supernumerary teeth, being themselves a developmental anomaly, in many cases become the cause of other disorders in the dental system:
- Due to the lack of space on the dental arch, the eruption of complete teeth is impossible or incorrect;
- The dentition is moved apart to form a diastema (widening of the interdental space);
- Cause malocclusion and facial asymmetry;
- By wedging into the dentition, they make the contacts of the side surfaces closer, as a result, the enamel is quickly erased, and the stuckness of food debris provokes caries.
The timing of removal depends on the depth of the location and the degree of impact on the surrounding teeth and the bite as a whole. Removal is much easier when eruption has already occurred.
If a tooth causes discomfort, it is removed
Easy removal
Simple is the removal of an already erupted supernumerary tooth.
The stages of the operation are standard:
- Anesthesia,
- Incision of the mucous membrane and exposure of the roots,
- Rocking and turning the tooth with an elevator to destroy the connective ligaments,
- Destruction of the bone at the root attachment site,
- Tooth extraction and rinsing the socket with hydrogen peroxide to wash away fragments and clots,
- Applying 1-2 stitches and a therapeutic bandage. Silk sutures are removed after 4-6 days.
Removal of an impacted tooth
Features that complicate removal:
- location deep in the jaw bone;
- irregular shape, twisted roots;
- proximity to the roots and rudiments of normal teeth;
- proximity to the walls of the maxillary sinus, nasal cavity and orbit.
Often the operation is performed by two doctors, a dental surgeon and his assistant.
The photo shows a rare case of hyperdontia
To gain access, the bone wall of the jaw is opened by drilling a series of small holes. Next, the tooth is exposed and extracted. Sometimes it is necessary to cut it into large roots and a crown. The hole in the bone is closed with a periosteum flap.
Anesthesia options
The operation is performed under regional (or regional) anesthesia. An anesthetic solution is injected with a needle into the space around a large nerve trunk, the branches of which surround the area of removal, “freezing” the conduction of pain impulses.
To make the injection imperceptible, at the beginning you can use topical anesthesia - this is what is called applying an anesthetic gel to the gums with a cotton swab (for children there are fruit flavors).
Conventional treatment of caries or pulpitis is carried out under the same anesthesia. In case of an atypical location, an additional injection may be required to better block pain sensitivity in the desired area.
Such anesthesia completely eliminates the feeling of pain for 3-5 hours, but does not affect tactile sensations, so during the removal the patient feels pressure, tapping, etc.
In some cases, adrenaline is added to the anesthesia drug - this substance constricts blood vessels and reduces bleeding, but when it enters the general bloodstream, it can cause a slight palpitation. This reaction is normal.
General anesthesia (with the administration of an anesthetic intravenously or inhalation) is rarely used and almost always in adults and children with inappropriate behavior (Down syndrome, cerebral palsy, various types of dementia).
Removing a supernumerary tooth is a complex operation
Symptoms
General manifestations of stomatitis include a general deterioration in health, lethargy, weakness, apathy, and sometimes fever. Children often become whiny, irritable, and refuse to eat or drink.
External signs of stomatitis of the palate include:
- Children often become whiny, irritable, and refuse to eat or drink.
swelling of the mucous membrane of the palate;
- redness of oral tissues;
- pain, difficulty eating;
- the appearance of painful ulcers, rashes;
- coating on the tongue.
If treatment is not started at the first signs, the ulcers will develop further, become covered with a grayish-white coating, become painful, and may merge into continuous erosion.
In this case, it is possible to increase body temperature to 38 degrees, headache, symptoms of intoxication of the body, enlarged lymph nodes in the neck, increased salivation. It hurts to drink, eat, talk.
Aphthous stomatitis: symptoms
If you suspect you have aphthous stomatitis, the symptoms are quite similar. A day or two before the onset of ulcers, patients usually notice a slight burning sensation in some areas of the oral mucosa. A little later, one or 2-3 clearly defined ulcers (aphthae) appear, covered with a necrotic coating of a gray or yellowish tint. The ulcers are round in shape and their diameter is usually no more than 1 cm, and along the perimeter they are surrounded by an inflammatory red halo.
Ulcers of this size usually heal within 10 to 14 days without scarring. However, in 10-15% of patients, the diameter of the ulcers may exceed 1 cm, and sometimes they can even reach 2-3 cm in diameter. Ulcers of this size are usually deeper than ulcers smaller than 1 cm (which may cause the ulcer border to appear raised). Healing of such ulcers usually lasts up to 6 weeks, and most often with the formation of scar tissue.
Important: the typical localization of ulcers is on the mucous membrane of the cheeks and the inside of the lips, on the soft palate (Fig. 7-8), tonsils, as well as the lower and lateral surfaces of the tongue. This localization is due to the fact that ulcers in aphthous stomatitis occur primarily on “non-keratinized” areas of the oral mucosa, i.e. where keratinization of the mucosal epithelium does not occur.
Less commonly, ulcers can occur on the keratinized mucous membrane (hard palate, dorsum of the tongue, tightly attached alveolar gum around the teeth) - this may be a signal of autoimmune diseases or HIV infection. In contrast to aphthous stomatitis, keratinized gums are affected precisely in herpetic stomatitis, which can also be a distinguishing feature of these two main forms of stomatitis from each other.
Foci of aphthous stomatitis on the soft palate: photo
→ Symptoms of herpetic stomatitis
Diagnostics
Differential diagnosis may be required to distinguish stomatitis from other pathologies of the mucous membrane
When the first signs of stomatitis of the palate appear, you should consult a doctor.
The dentist deals with diseases of the oral cavity.
The diagnosis is made in most cases based on a patient interview and examination.
Most often, this is enough to confirm the disease and determine its type.
If in doubt, a test is carried out for candidiasis and herpes, bacterial culture of a scraping or smear.
Differential diagnosis may also be required to distinguish stomatitis from other pathologies of the mucous membrane.
For frequent stomatitis, especially one that is difficult to treat, the dentist may send the patient for a general examination to identify systemic and chronic diseases that are its causes.
Hyperdontia in an adult
In adults, hyperdontia is much more common than in children. Additional teeth are mainly located in the palate or on the gums, which is unnatural and contrary to the norm. The eruption of an “extra” tooth can cause the following symptoms:
- Impaired diction. The person begins to burr and vaguely pronounce some sounds and sound combinations.
- A feeling of discomfort caused by the abnormal position of supernumerary teeth. Such teeth provoke curvature of the dentition.
- Malocclusion. This problem entails a number of dental diseases, such as pathological tooth wear, impaired diction and others.
- Damage to the oral mucosa with subsequent inflammation;
- Impaired chewing function, which leads to gastrointestinal problems.
This type of anomaly often causes nervous breakdowns and mental disorders. Due to the displacement of the dentition, healthy teeth lose their strength and begin to loosen under the pressure of the growing supernumerary rudiment. The jawbone swells, which leads to pain. Constant aching pain leads to irritability, apathy and deterioration in general well-being.
Treatment
Treatment of stomatitis is carried out with the help of medications, which include both tablets for oral use and external agents: gels, ointments, rinsing solutions, irrigation sprays. Folk remedies have proven themselves to be quite good - mainly rinses.
Important! To choose the right treatment method, you need to know the nature of the disease, and only a doctor can definitely determine it.
Drugs
Medicines for the treatment of stomatitis of the palate are divided into the following groups:
- In case of allergies, antihistamines are prescribed; it is also important to eliminate the allergen
For pain relief. They do not treat the disease itself, but are used to relieve symptoms that prevent the patient from eating and speaking. Anesthetics are available both in the form of external preparations and for oral administration.
- Anti-inflammatory. Such funds are prescribed without fail. As a rule, they are external. These are gels (Cholisal, Kamistad, Actovegin), lozenges (Eucalyptus M), sprays for irrigation (Cameton), rinses (Ingafitol).
- Antiviral or antihistamine. The former are prescribed for the viral nature of the disease, the latter for the allergic nature. Antiviral ointments include Bonafton, Interferon, Oxolinic and Tebrofen ointments. In case of allergies, antihistamines are prescribed; it is also important to eliminate the allergen.
- Accelerating healing. Such drugs are prescribed during the recovery stage to speed up tissue regeneration. These include Solcoseryl gel, Karotolin oil solution, propolis spray, preparations based on sea buckthorn and rose hip oils.
Important! Local medications quickly relieve the condition, but in most cases they alone are not enough for recovery. Greater effect can be achieved with complex therapy.
How to treat ulcers using traditional methods?
Traditional methods in the form of rinsing and lubricating go well with medications and can speed up recovery:
- The more often you rinse, the faster the effect will come.
Aloe juice - lubricate the sores several times a day, rinse your mouth thoroughly before doing this;
- Chamomile flowers - brew a tablespoon with a glass of boiling water, leave, rinse your mouth several times a day;
- Calendula flowers - soak a tablespoon in a water bath in a glass of water for 10 minutes, leave, use for rinsing;
- Propolis tincture - after rinsing, wipe the wounds with hydrogen peroxide, then drop the tincture on each of them;
- Carrot juice - lubricate the sores several times a day, also mixed with water can be used for rinsing.
Traditional methods also advise rinsing your mouth with hydrogen peroxide or a weak soda solution. The more often you rinse, the faster the effect will occur. It is especially important to do this after eating.
The main symptoms of polyodontia
The eruption of supernumerary units may have different signs in children and adults. For example, some babies are already born with such teeth. It becomes very difficult to feed them, as they injure the nipple during breastfeeding.
When a supernumerary tooth grows in an older child, symptoms may include:
- the appearance of pain at the site of eruption;
- temperature increase;
- in rare cases – stomach upset;
- swelling of the upper respiratory tract;
- salivation.
The most difficult thing to endure is the eruption of excess teeth on the upper palate. When the baby begins to talk, polyodontia has a negative effect on the pronunciation of sounds. On top of that, the tongue and oral mucosa are constantly injured, which provokes the development of inflammatory processes.
We suggest you read: How many teeth should a person have?
Features of treatment in adults and children
In order for the treatment of palate stomatitis to be beneficial, you need to adhere to the following recommendations:
- Antiseptic rinses should be used after each meal, keep the mouth clean
The drug should be selected based on the nature of the disease ; antiviral drugs will not help against allergic stomatitis, and vice versa. Choosing the wrong remedy will only make the situation worse. Therefore, you cannot do without consulting a doctor.
- Antiseptic rinses should be used after each meal, and keep your mouth clean.
- When treating stomatitis in an infant, you should carefully treat all his personal belongings: feeding bottles, pacifiers, pacifiers, toys that he chews.
- Ointments and gels for treatment should be specifically for the mucous membranes. The usual ones, which are used for the skin, will not help.
- At the first stage, agents are used to eliminate the source of the disease and its causes, then, when the ulcers begin to dry out, it is the turn of wound healing agents.
In addition, during the treatment of stomatitis, you should take care: do not overcool, strengthen your immune system, avoid stress and do not eat food that irritates the oral mucosa.
Aphthous stomatitis in children: treatment
Aphthous stomatitis in adults is the same as canker sores in children - the treatment is the same, and the treatment strategy described below is suitable for patients of any age. As for the medications listed later in the article, some of them do have age restrictions, which we will also indicate.
Due to the fact that it is usually impossible to clearly identify the specific cause of aphthous stomatitis in a particular patient, treatment will be multifocal, i.e. drugs of several groups are used simultaneously. The choice of treatment strategy and medications will depend on the following 3 factors:
1) on the severity of symptoms, 2) on the frequency of relapses, 3) on identified predisposing factors.
Treatment at the first stage should be aimed at reducing pain and inflammation in the area of ulcers, and at the second and third stages - at speedy epithelization of ulcers and preventing their occurrence in the future. To facilitate the choice of the best treatment option, all patients can be divided into 3 types (according to the criteria - severity of the disease and frequency of relapses).
- Type A - in patients of this type, aphthous stomatitis occurs no more than several times during the year and is characterized by slight pain.
First of all, in such patients it is necessary to identify local predisposing factors and eliminate them (for example, overhanging edges of fillings or hygiene products with sodium lauryl sulfate). It is important to ask the patient about eating habits to evaluate a possible relationship between stomatitis outbreaks and certain foods. The patient is advised to avoid solid foods (eg, crackers, toast), all types of nuts, chocolate, eggs, acidic drinks or foods - fruit or citrus juices, tomatoes, pineapples, salty foods. You should avoid eating spicy foods, any spices, including pepper and curry, as well as alcoholic and carbonated drinks. In type A patients, local symptomatic therapy is mainly used, which includes antiseptic rinses and gel applications for pain and inflammation.
- Type B - in such patients, aphthous stomatitis develops almost monthly, and the ulcers are so painful that they force the patient to change habits (for example, brushing teeth less often due to severe pain). It remains important to identify local and general predisposing factors and, if possible, eliminate them. It is very important to teach patients of this type to feel the first signs of the imminent appearance of ulcers - burning, itching or swelling of the mucous membrane, in order to provide early local treatment even before the formation of the ulcers themselves.
- Type C - in patients of this type, ulcers are very painful, appear so often that while one lesion is healing, the next one appears almost immediately. This group also includes patients in whom local treatment in the oral cavity is completely ineffective, and improvement in their condition occurs only after the use of systemic therapy.
Prevention
To prevent the occurrence of stomatitis, the following preventive measures must be observed:
- careful adherence to oral hygiene;
- proper balanced nutrition;
- avoiding mechanical injuries to the oral cavity;
- avoidance of stressful situations;
- strengthening the immune system;
- rejection of bad habits.
For any disease, and stomatitis of the palate is no exception, the best prevention lies in a healthy lifestyle. The less harmful and undesirable things there are in life, the better for overall health.
Prevention of stomatitis development
The following are worth noting as preventive measures:
- Keeping your mouth clean. It is necessary to visit the dentist’s office if you have any problems with your teeth, since trauma to the oral cavity is one of the factors in the formation of stomatitis.
- If stomatitis develops as a reaction to certain foods, then they must be removed from your diet. If it is impossible to track the food provocateur, it is necessary to keep a special diary that will help identify the culprits. Just write down all the foods you consume during the day, as well as your body's reaction.
These simple rules will certainly help avoid the development of this unpleasant disease.
Diagnostic methods
Diagnosis of polyodontia is carried out exclusively by a specialized doctor - an orthodontist, who conducts a preliminary examination of the oral cavity and dentition, refers the patient to x-rays (orthopantomography) and analysis of anthropometric casts of teeth made of plaster. Such models are made for a more detailed study of a specific anomalous phenomenon, on the basis of which a diagnosis is then made and treatment is prescribed.
Table of normal human teeth.
Deviation from the norm - polyodontia When examining plaster models made on the basis of dental casts, the doctor measures the size of the teeth, and then analyzes the data obtained based on a special table by Wetzel and Ustimenko. The length of each row of teeth must be measured. This indicator may fluctuate depending on such characteristic individual characteristics of a person as crowding of teeth or the presence of large gaps between them.
We suggest you read: Why and how to clean a person’s tongue
What is stomatitis on the palate?
Stomatitis is an inflammatory disease of the oral mucosa.
It causes white sores, rashes on the tongue, inner surface of the cheeks, and gums. The type of stomatitis that will be discussed in the article is characterized by the localization of the lesion on the palate. The disease does not pose a direct threat to the life and health of the patient, but causes discomfort. With the treatment provided, stomatitis lasts from 4-5 days to 2 weeks.
ICD-10 code
According to the International Classification of Diseases, stomatitis is assigned the number K12 :
By 12.0 – recurrent aphthae of the oral cavity.
K 12.1 – other types of stomatitis.
K 12.2 – phlegmon and abscess of the cavity.
Causes
The disease progresses against the background of poor oral hygiene.
The causes of stomatitis in the palate are:
- hereditary predisposition;
- hormonal changes in the body;
- chronic pathologies of the gastrointestinal tract, cardiovascular system;
- oncological neoplasms, chemotherapy;
- mechanical injuries to the palatal surface due to eating solid foods or malocclusion;
- weakening of the body’s protective properties during psychological stress;
- lack of vitamins and beneficial microelements;
- allergies to certain foods;
- non-compliance with oral hygiene rules;
- severe dehydration of the body;
- presence of parasites;
- long-term antibiotic therapy;
- use of toothpastes containing sodium lauryl sulfate.
The negative effect of sodium lauryl sulfate is manifested in severe drying of the palatal mucosa and the formation of microcracks on it. As a result of such exposure, the surface of the palate becomes vulnerable to various pathogenic microorganisms.
Caries as one of the causes of stomatitis
Tooth decay is a common problem among adults and children. It is because of carious lesions of tooth enamel that many dental diseases arise, including stomatitis. Caries develops gradually, starting with slight demineralization of the enamel, when it becomes dull and rough areas with increased porosity appear.
The main cause of caries is insufficient oral hygiene. After eating any food, food fragments remain in the interdental spaces, which are a breeding ground for cariogenic microorganisms.
Against the background of caries, the infection can spread further, affecting the pulp, bone structures, ENT organs and oral mucosa.
For inflammatory areas on the palate and erosions, the dentist sanitizes the oral cavity and examines the teeth. If there are carious lesions, it is necessary to remove them using a drill and carry out the necessary therapeutic measures.
The following factors provoke the appearance of carious defects:
- bad habits (smoking, alcoholism, chewing nuts, hard objects);
- irregular oral hygiene, use of low-quality toothpastes;
- damage to tooth enamel by aggressive foods;
- dental injuries;
- vitamin deficiency, lack of calcium and fluoride;
- excessive consumption of foods that contain simple carbohydrates and weaken tooth enamel (chocolate, sweet carbonated drinks, jams, juices, coffee, tea, citrus fruits);
- metabolic disorders, endocrine pathologies.
Based on this list of predisposing factors, the principles for the prevention of caries and stomatitis are built. The dentist will not only prescribe treatment, but will also recommend therapeutic and prophylactic toothpastes that have high antibacterial activity, and will also develop preventive measures.
Any doctor will tell you that it is best to prevent the disease, especially since the prevention of caries and stomatitis is simple and accessible to every person.
Symptoms of stomatitis
The main symptom of the disease is the appearance of painful ulcerations on the surface of the oral mucosa (photo below). More precisely, at first a slight redness appears, which later transforms into a painful ulcer of a regular round or oval shape. But this period most often passes unnoticed for a person.
If treatment is not received at this point, the surface of the ulcer becomes covered with a grayish-white coating. At the same time, it causes a lot of trouble for a person, since stomatitis ulcerations are very painful. The surface of the mucosa around the ulcer remains unchanged.
Advice! Treatment of stomatitis with so-called “blue iodine” is quite effective. Methylene blue (the official name of the product) has excellent healing properties. The drug acts completely painlessly. That is why it is recommended for the treatment of stomatitis in children.
Ulcers can be either single or multiple. For a severe course, the ulcerations merge into a single spot. Pathology in this case is accompanied by:
- increased general body temperature;
- enlargement of nearby lymph nodes;
- severe headache;
- loss of appetite;
- increased salivation.
Stomatitis is almost always accompanied by the development of pain, which prevents a person from speaking and eating normally.
Who's at risk
Stomatitis with localized inflamed areas on the palate is more common in children. A young child is susceptible to developing stomatitis. This is due to the gradual “maturation” of the immune system.
Read more about the symptoms of childhood stomatitis on our website.
Many parents do not teach children to brush their teeth until they are 3-4 years old, although dentists recommend removing food debris after each meal with moistened gauze even before the first tooth appears.
In adults, stomatitis on the upper palate occurs mainly due to thermal and mechanical injuries. The infectious and viral nature of the disease more often causes the appearance of erosions and inflamed areas on the tongue and the inner surface of the cheeks. Stomatitis in the soft palate is the result of an incorrectly selected prosthesis, damage to the mucous membrane from hot drinks and food.
Read about how stomatitis occurs in adults.
The main provoking factors for stomatitis:
- weakening of the local protective reaction;
- endocrine diseases, including diabetes;
- trauma to the mucous membrane from dentures, braces, tissue damage due to bruxism;
- using an overly hard toothbrush;
- aggressive dental treatment;
- allergic reaction;
- decreased immunity due to severe operations, hormonal treatment and the development of immunodeficiency conditions.
This is interesting: How to remove brown plaque on teeth and dark spots near the gums on the inside
To choose the right treatment for stomatitis, you first need to determine the nature of the disease and conduct a comprehensive examination. If relapses of inflammatory processes occur frequently, the dentist pays attention to the state of the immune system and identifies hidden immunodeficiency states, endocrine diseases, and hormonal disorders.
Stomatitis on the palate of a child - photo
What could be the consequences?
Very often, stomatitis goes away on its own , but if the body’s defenses fail to cope with the disease, the inflammation spreads to adjacent areas and can develop into a more severe form . In this regard, at the first signs of illness, you should consult a doctor.
Complications
If ulcers appear, treatment should be started immediately. Acute stomatitis must be stopped to prevent the development of complications:
- damage to the tonsils;
- bleeding gums;
- inflammation of the lymphatic system;
- chronic tonsillitis;
- laryngitis;
- secondary infections.
Stomatitis during pregnancy and treatment features
During pregnancy, a woman's body experiences a hormonal imbalance, against the background of which the immune system is sharply weakened. It becomes vulnerable to viruses and bacteria, so inflammation of the mucous membranes in the mouth is a common problem in the first trimester. The most likely diagnosis is herpes or candidal stomatitis, occurring on the tongue or palate.
Treatment of pregnant women requires special treatment. When selecting medications, the doctor is guided by safety for the fetus and placenta, giving preference to natural-based medications without allergens and side effects. Light gels with antiseptics are effective:
- Holisal;
- Asepta;
- Viferon.
Ulcers can be treated with Miramistin solution, avoid alcohol formulations and tinctures. In the second trimester, it is allowed to use antiallergic drugs that relieve swelling and irritation of the gums: Claritin, Loratadine, Suprastin. In case of complications of herpes, it is recommended to undergo treatment in a hospital under the supervision of a specialist.
Preventive actions
To prevent the disease from progressing to a severe stage, it is necessary to treat the surface of the palate with medicinal agents every 3 hours for the first 2-3 days of the disease. To prevent the formation of palatal stomatitis, it is recommended:
- maintain a diet;
- carefully monitor oral hygiene;
- regularly clean the house using antibacterial agents;
- use personal hygiene items;
- promptly treat dental diseases;
- avoid mechanical injury to the oral mucosa.
To prevent the development of such a pathology, it is necessary to beware of damage to the tissues of the oral cavity, use dental floss, and rinse the oral cavity with antiseptic agents. If any pathological processes appear in the mouth, you should contact a specialist and not self-medicate.
Why is the upper palate inflamed?
The vault of the mouth, connected to the larynx and separating the nasopharynx and oral cavity, is called the palate. It consists of two sections - soft and hard. The first section is muscle tissue, which is often subject to inflammation, while the second includes the bone tissue of the upper jaw. A clear example of inflammation of the upper palate in an adult is presented in the photo accompanying the article. The palate becomes inflamed due to various reasons, for example:
READ ALSO: Yellow palate in the mouth: causes with photos and treatment
- allergy,
- dental diseases (pulpitis, caries, osteomyelitis),
- neuralgic diseases,
- contact inflammation (when using dentures to eliminate dental defects),
- injuries,
- infectious diseases (laryngitis, sore throat),
- stomatitis.
READ ALSO: Stomatitis in a baby's mouth: symptoms with photos and treatment With the development of an inflammatory process affecting the palatal tissues, we will talk about one of the types of stomatitis - palatinitis. If, along with inflammation, a tumor appears on the surface of the palate - even the smallest and insignificant one - this is a reason to urgently consult a doctor. In most cases, such neoplasms are benign (fibroma, neurofibroma, lymphangioma, hemangioma, papilloma). However, only a qualified doctor can exclude a malignant lesion (cylindroma or glandular cancer) and prevent the degeneration of a benign formation.