All about how to avoid dangerous complications after dental implantation
Despite the fact that dental implantation appeared a long time ago, it is still relatively safe today. Especially often, complications after treatment occur if the patient made a mistake in choosing a professional doctor or repeatedly violated his recommendations during the rehabilitation period after surgery.
One of the most serious complications that a person who has received their dream smile may face is peri-implantitis. In the article presented below, we will consider in as much detail as possible what this phenomenon is, how it is characterized, why it occurs, whether it is possible to recover from it without consequences for your health, wallet, and, in fact, save the installed implant.
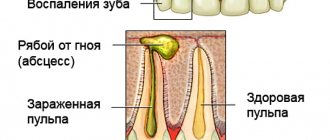
What is the essence of the disease
Peri-implantitis is an inflammatory process that affects not only bone, but also soft tissue located around and near the implant. This complication can also provoke the destruction of bone tissue, which gradually becomes thinner and decreases in volume.
The saddest consequence of peri-implantitis is implant rejection and the need for its removal. All this is accompanied by a long rehabilitation period and the need to re-build and restore bone structures. Naturally, such actions for all patients, without exception, are associated with unnecessary expenses not foreseen in advance, psychological and physical discomfort, and disappointment.
Infection can occur a short period of time after implantation, or it can manifest itself after months or even years of successful use of titanium roots.
Peri-implantitis is often confused with mucositis. The second disease is also characterized by inflammation of the tissues adjacent to the implant, but their pathogenesis and clinical manifestations are different: with mucositis, the bone does not decrease in volume and does not become worse in quality. That is, mucositis is a purely superficial inflammation.
Reasons for development
There are several etiological factors that lead to the gradual development of peri-implantitis and inflammation. There are a few of the most common ones:
- quality of the implantation system;
- reliability of the prosthetic design;
- insufficient oral hygiene;
- complications in the postoperative period.
In most cases, peri-implantitis develops when the doctor made technical errors and mistakes during surgery. Procedures such as dental implantation and dentures should be trusted to qualified dentists. After the operation, you must observe hygiene standards and perform mandatory hygiene procedures daily.
Medical errors rarely lead to the development of the disease. Peri-implantitis can develop as a result of violated rules of asepsis and antisepsis, as well as when risk factors were incorrectly assessed. They can influence the success of the procedure.
Pathology develops due to improper manufacturing of orthopedic structures and implants. These could be crowns or dentures. When they have a poor anatomical shape, overload or chronic trauma to the periodontium occurs.
Typical factors in the development of pathology:
- Formation of subgingival hematoma and its suppuration;
- The bone bed does not correspond to the size of the installed implant;
- The design becomes too mobile when worn;
- Gradual destruction of bone tissue;
- The area around the tooth may become inflamed and fester, exposing the implant structure.
People with bad habits are at risk. These may be smokers who do not take good care of their oral cavity. Patients with periodontal diseases (periodontitis, gingivitis, periodontal disease, apical periodontitis), immune disorders need to regularly visit the dentist.
Factors provoking peri-implantitis
The reasons for the development of this disease may be the following factors:
- doctor’s mistake during implantation: most likely, due to his unprofessionalism, the doctor selected the wrong implant model. It is also possible that the doctor violated sterile conditions during implantation, injured the bone during their installation, or incorrectly applied sutures,
- lack of a proper stage of preparation for the procedure: this is again the doctor’s mistake, but also the patient’s responsibility. The banal presence of a cold at the time of the procedure, weakened immunity, the presence of hidden from the doctor or undiagnosed chronic diseases of the body, teeth and gums in the acute stage can cause peri-implantitis and lead to implant rejection. The formation of a secondary infection may also be to blame here. If inflammation is not eliminated before implantation, it will most likely make itself felt again. And peri-implantitis can be caused by more than 300 types of bacteria,
- the formation of gaps between the abutment and the metal rod: this situation is very likely if the clinic does not use the original models of implants, but their cheaper analogs, whose production is not supported by a sufficient positive research base. That is, a situation can occur if an implant from one company was used and an abutment from another,
To avoid getting into an awkward and even dangerous situation, find out in advance which brands of implants the doctor offers for installation. Check that the specialist has the necessary quality certificates, as well as certification for the right to use the presented models of artificial roots in his practice.
- Violation of doctor's recommendations during the rehabilitation period: abuse of alcohol and nicotine can be fraught with consequences. A heavy load on the implant or injury to the place where it is located will not lead to anything good.
- poor oral hygiene: even months and years after installing an implant, do not forget that you need to take care of it in the same way as a natural tooth, because the accumulation of plaque and bacterial infection in the oral cavity, even in the absence of living teeth, has not yet been canceled. Also, do not forget to visit a doctor several times a year for the purpose of prevention and examination of artificial structures,
- excessive load on the implant from the prosthesis: most likely, in this case, the design was performed incorrectly by the orthopedic doctor. Or the patient himself, after installing new teeth, used them too actively.
It is often possible to determine the etiology of the disease based on the time when it appeared. If pathology occurs immediately after installation of the implant, most likely the doctor is to blame, or low-quality materials were used. But the development of the disease years later speaks of the patient’s own fault.
Symptoms of complications
Peri-implantitis is often confused with other inflammatory soft tissue diseases. Let's consider the symptoms that distinguish this process from other pathologies:
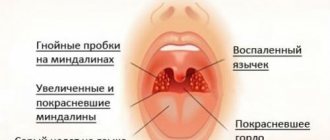
- swelling of the tissue around the implant and a change in the color of the mucous membrane from pale pink to bright red,
- bleeding, possible suppuration and fistula formation,
- the gum peels off from the implant by more than 1 millimeter, becoming loose: a so-called periodontal pocket is formed,
- painful sensations, especially when pressing, chewing and even just touching the tongue,
- the implant may wobble and move,
- noticeable thinning of bone tissue.
If you experience any of the signs listed above, then it's time to make an appointment with your doctor. Do not attempt to diagnose peri-implantitis or carry out treatment on your own. The specialist will analyze the situation using modern radiography methods and select a set of measures to successfully eliminate the problem.
Signs of early dental implant failure
After implantation, you should visit your doctor frequently. Already 2-3 days after the intervention you should come for the first appointment. These inspections will help identify the problem in time.
At the appointment, the dentist evaluates the stability of the implant and the condition of the tissues around it. He will see whether the structure fuses well with the bone, whether additional surgical intervention is required, and whether there are signs of inflammation.
Unpleasant symptoms are considered normal after implantation, and since surgical implantation is associated with tissue trauma, after this there is always swelling and redness of the gums, and soreness of the jaw.
These problems should go away in 3-4 days, sometimes it lasts up to a week. If the patient feels severe pain that does not go away or intensifies, then an urgent visit to the attending physician is necessary. Only he will determine whether the rejection process is underway or whether it is an individual reaction of the body to a foreign body.
In some cases, with simultaneous bone grafting and the presence of inflammatory processes in the socket, the rehabilitation process is delayed up to several weeks.
Stages of the disease
- stage 1: bone tissue decreases slightly in the horizontal direction. The soft tissues change color, the implant may wobble a little, slight pain is felt, and the shape of the gums may change,
- Stage 2: The jaw bone decreases moderately in height, forming a vertical defect where it grips the implant. The implant moves, the pain increases, the gums peel off, a periodontal pocket forms,
- stage 3: the gum moves away greatly from the implant, to the point that the metal elements of the structure become visible. At the site of localization of the inflammatory process, pus may appear, the patient also begins to be haunted by a putrid odor from the mouth,
- Stage 4: Bone resorption occurs. The destruction becomes pathological. At this stage, it is no longer possible to save the implant.
Regarding the clinical picture of the disease, acute and sluggish peri-implantitis, stages of remission and re-intensification of the pathological process are distinguished.
Signs of peri-implantitis
Peri-implantitis - an inflammatory process around the implanted element may appear immediately after surgery, but there are cases of rejection several years after installation. Therefore, you cannot relax: careful oral care is necessary throughout your life. Your dentist will tell you how to properly clean your teeth and care for your dentures.
Signs of rejection:
- change in the color of the gums around the prosthesis, the appearance of a bluish tint and redness;
- hyperemia around the prosthesis - slight swelling of the soft tissues;
- separation of the mucous membrane from the artificial crown, loose fit;
- discomfort when chewing food increases over time, turning into pain;
- heavy breathing, bad breath due to pus;
- bleeding from the hole near the prosthesis;
- looseness of gum tissue;
- hyperthermia, temperature can rise to +39C;
- noticeable mobility of the prosthesis.
The listed symptoms may appear all at once, but not necessarily. At the first signs of a pathological condition of the tissues around the implant, you need to consult a doctor, then there is a chance to save the prosthesis.
During the first 5-6 days after surgery, some of the listed symptoms of peri-implantitis may be observed: swelling, inflammation, pain, hyperthermia. This is normal. If the inflammation does not go away after a week, you should consult a doctor.
What happens to the implant in the oral cavity when foci of inflammation appear? The problem may concern not only the implanted metal rod; stability may lose:
- gum former;
- artificial tooth crown;
- stub.
The structure loses stability, the fastening of elements to each other may weaken. Shakiness and instability of structural elements can be felt when chewing or brushing your teeth.
How to diagnose the problem
Peri-implantitis can be diagnosed through visual examination using special instruments. It is important to assess the condition of the mucous membrane, its swelling and hyperemia, which are the main symptoms of the disease. Palpation of the gingival pocket is often accompanied by the release of purulent exudate. The implant wobbles, and soft plaque accumulates on the prosthesis and neighboring teeth, if they exist in the oral cavity.
In addition to visual inspection, other examination methods are also used:
- orthopantomogram and 3-dimensional computed tomography, allowing to identify bone resorption and the degree of development of the inflammatory process,
- probing to assess the depth of periodontal pockets,
- laboratory tests: bacteriological, PCR, biochemical, pH-metry of oral saliva. Such studies are in the nature of diagnostic aids. But, as a rule, the doctor is limited to carrying out exclusively the first two points - they are more than enough to make a correct diagnosis.
Symptoms
Symptoms of this disease appear gradually:
- Initially, at the site of an already healed implant and installed dentures, inflammation of the gum area appears, which manifests itself as slight redness, swelling and discomfort, especially during chewing
- If the patient does not consult a dentist on time, the disease progresses, inflammatory processes intensify, and gum bleeding in this area increases.
- As a result of inflammatory changes, connective tissue grows
- Periodontal pockets of varying depths are formed, from which serous fluid or purulent discharge is released
- Inflammation is accompanied by sharp, prolonged pain
- Pathological mobility of the implant appears, which intensifies as inflammation manifests itself
- The radiograph shows areas of bone resorption around the installed implant.
Important! External trauma to a bone area with an installed implant requires a mandatory consultation with a dental surgeon to assess post-traumatic complications and prevent the development of peri-implantitis.
Treatment of the inflammatory process
It is important that the treatment of peri-implantitis is comprehensive. Whether surgical intervention is required or therapy is sufficient - the doctor decides here, based on the stage of development of the inflammatory process. But, as a rule, if the bone is destroyed on 2 or more sides, the implant still needs to be removed. But let's look at possible treatment options in more detail.
Surgical method
This is not the removal of the implant, but the removal of inflamed, granular tissue with subsequent replenishment of bone material. This method consists of the following steps:
- preparatory: sanitation of the entire oral cavity, administration of anesthesia. During the procedure, sterility is required to prevent the penetration of bacteria and the development of additional infection,
- opening the problem area, cleaning the entire periodontal space from pus, if there is suppuration,
- inspection of the implant, its treatment and antiseptics with special preparations, for example, hydrogen peroxide,
- bone grafting, gum suturing and suturing,
- prescription of accompanying therapy: medications, antibiotics, home rinses, physiotherapy.
The specialist can change the stages of surgery depending on the specifics of the situation. It is better if these manipulations are performed by the same doctor who performed the implantation.
In general, antiseptic treatment of an exposed implant, especially if it was recently installed, is quite dangerous. Because good models from well-known brands have various coatings on the surface, which help accelerate the growth of bone tissue cells. And during processing, such a coating can be easily damaged.
Non-surgical method: drug therapy
It is possible to refuse surgical intervention in the treatment of peri-implantitis if the disease is in the initial stages and pathological changes have not yet occurred in the bone structure of the jaw, i.e. significant tissue loss and destruction did not begin.
The non-surgical method involves taking medications, among which antibiotics are mandatory. It is also recommended that the patient replace or modify the prosthetic structure and place it in the hands of professionals for high-quality disinfection. It is also necessary to strengthen oral hygiene, eliminate bad habits, and normalize the diet. Additionally, restorative physiotherapy procedures may be prescribed.
Often, with peri-implantitis, doctors are inclined to favor a radical method of solving the problem, namely the removal of a previously installed implant. This will avoid recurrence of this complication, which occurs quite often when using conservation therapy. After removing the structure, the specialist restores the bone tissue, applies a protective membrane, and only six months after rehabilitation returns to the implantation procedure.
Treatment
Periodically, at conferences and congresses, doctors are fooled by showing cases of “successful treatment” of peri-implantitis: here they polished the implant, here they poured a graft, here they covered it with a membrane and... the cost of such treatment turns out to be much more expensive than the cost of re-implantation and re-prosthetics. In addition, I have never seen good results in the treatment of peri-implantitis outside of all these seminars, congresses, conferences…. And this once again says that there are no confident and reliable methods for restoring bone tissue around an integrated implant - otherwise they would not be shown at any events.
Yes, peri-implantitis cannot be cured. Lost bone tissue around the implant is almost impossible to restore in full. But we can drive the problem into a state of stable and long-term remission, making sure that it does not in any way affect the patient’s quality of life, or the reliability and durability of the prosthetic structure, or the life expectancy of the implants themselves. Like here, for example:
The task looks quite trivial: it is necessary to eliminate the factors that led to the development of peri-implantitis, or to reduce their influence to a minimum.
To solve it, you need to do the following:
1. Remove prosthetic structures from the implants. If the orthopedist was a far-sighted fellow and used screw fixation, then this is very easy to do. Crowns fixed with cement are much more difficult to remove and often require breaking to gain access to the abutment and screw.
As a rule, in advanced cases of peri-implantitis, a “gum catastrophe” - the mucous membrane is swollen, inflamed, and upon palpation, ichor or pus is released along the perimeter of the platform. The raccoon understands that in such conditions it is useless and simply dangerous to carry out any operations, so it is worth plugging the implants and waiting. until the gums return to normal. Usually two to three weeks are enough for this.
2. After a couple of weeks, the gums will calm down, the swelling will go away, and the implants will heal a little. From this point on, you can begin planning and performing surgical treatment. It consists of several stages.
2.1. It is necessary to remove all granulations, dental plaque and other nasty things that are in it from the peri-implant funnel. Sometimes this requires opening the funnel - we do this using a conventional surgical handpiece or a piezosurgical system.
2.2. As a result of the destruction of surrounding tissues, part of the implant ended up above the bone tissue. “Pushing” it back is a bad and unreliable solution. It is much easier to convert a subgingival implant into a transgingival one. In the end, why is your Dentium Superline worse than Straumann TL? Transgingival implants work great! To do this, we use a set of burs and a contra-angle handpiece to remove all the threads that are above the bone from the implant and polish its surface. BE SURE to do this with the plug or healing abutment in place to avoid damaging the platform.
2.3. Peri-implantitis is a chronic inflammatory disease. As with any chronic inflammation, the body builds the so-called. “demarcation boundary” along the perimeter of the inflammatory focus. This boundary, consisting of tissue macrophages and antibodies, separates the damaged area from the rest of the body, which, on the one hand, prevents the spread of infection and damaging factors, on the other hand, it “turns off” the nutrition and blood supply to the bone inside the inflammation zone - something similar to the formation of a sequester occurs , a section of dead bone along the perimeter of the peri-implant funnel. To ensure access of living cells into the funnel itself and restart the regeneration processes, dead tissue must be removed as much as possible. We do this using a surgical contra-angle or straight handpiece with a set of carbide burs, or we use a piezosurgical system.
2.4. At this stage, some doctors fill the resulting bone defect with a graft and cover it with a membrane in the hope that the bone tissue will recover. Hope dies first if you know how grafts and membranes work and how bone regeneration occurs. If you have only seen this technique on TV, this does not mean that it confidently and 100% gives good results. Rather, on the contrary, otherwise no one would be interested in her.
Therefore, we do not use biomaterials to treat peri-implantitis - it is expensive and stupid. We leave the peri-implant funnel as is, hoping for at least partial restoration of the bone. This is, in fact, what happens subsequently.
2.5. The next step is to change the biotype of the mucous membrane towards thickening. To do this, we use a free connective tissue graft (FCT):
2.6. Next, we seal the surgical wound tightly and prescribe postoperative antibacterial and anti-inflammatory therapy.
2.7. The stitches are removed after 10-14 days.
2.8. 4-6 weeks after surgery, we reshape the gum. If the implants allow you to switch platforms, it is better to do so.
2.9. After another two weeks, you can begin re-prosthetics, or return, adjust and return the previously made denture to its place. If previously crowns on implants were fixed with cement, then when making new ones it is better to sacrifice aesthetics in favor of screw fixation.
2.10. Subsequent preventive examinations at 2, 4, 8 and 24 weeks allow you to evaluate the result of the treatment.
Judging by the images, we did not cure peri-implantitis, but its development stopped, the symptoms that bothered the patient disappeared, and the quality of life increased. This is exactly what we wanted.
Folk remedies: is it possible to cure inflammation at home?
Even the initial stage of the disease cannot be cured with rinses and lotions. If the bone begins to dissolve, only a highly qualified dentist in the clinic with the necessary tools and equipment can help. After the examination, the doctor will determine which treatment method is most suitable in a particular case.
When the treatment has already been carried out in the clinic, at home the patient will carry out oral baths and rinses with products prescribed by the doctor - these are antiseptics, decoctions of medicinal herbs.
Prognosis and prevention: will it be possible to save the installed implant?
If the treatment was possible and it was carried out by a professional doctor, the result will be positive and the implant will last for many more years. But again, you need to understand that if inflammation occurs, it can recur. And this, again, is a certain risk. Therefore, it is imperative to strengthen your oral hygiene and strictly follow all the recommendations of your doctor:
- visit the dental clinic regularly (2-3 times a year) - according to the rules established in your medical center,
- avoid injuries and stress on new teeth - although they are artificial, they are not much stronger than real ones,
- do not abuse alcohol and cigarettes, especially in the first days of the week after implantation,
- Monitor the overall health of the body (in the presence of chronic diseases) and maintain it with the help of a proper diet, reasonable physical activity, hardening, and taking vitamin complexes.
Most implant manufacturers today provide a lifetime guarantee on titanium roots, i.e. in fact, they can last forever. But in order for this promise to be fully fulfilled, look for a competent specialist and be responsible in the future. Then even budget models will constantly please you, but otherwise, premium-segment implants may cause disappointment.
More complete information on implant care can be found in a separate article on the website. Proper care of structures will be an excellent prevention of peri-implantitis.
It is also interesting that today the risks of developing peri-implantitis can be reduced by treatment protocols, the planning of which is carried out using special computer programs for visualization, in which the doctor works on the basis of tomographic data. For example, dental prosthetics on 4 implants, the cost of which is not so high compared to other methods. But due to careful study of the treatment process, it is possible to significantly reduce postoperative risks.
Classification
Anomalies are divided depending on the stage of the disease and the timing of its occurrence, relative to the time of the operation to install the implant.
By stages
Like all diagnoses, peri-implantitis is characterized by several stages of the pathology, each of which is characterized by certain clinical manifestations:
- The first stage - the hard tissue becomes somewhat thinner , it seems that the gums seem to “dry out”, and pockets form in the resulting gaps. The crown is not attached so firmly, causing redness of the surrounding tissues and minor bleeding. The bone still retains its integrity
- The process reaches the second stage, if you do not resort to medical help , the deformation of the organ will continue further, the tissue partially atrophies, becomes looser, the gums begin to peel off from the structure, the pockets expand. The tooth gains mobility.
- The third is accompanied by severe pain , which occurs upon any contact with the organ. The tooth is almost no longer fixed in the socket, and the abutment becomes visible, and structural decomposition of the soft tissues begins vertically relative to the root.
- Fourth – the alveolar is almost completely destroyed . The device is visible through the gum and is hardly held in place. Accompanied by the appearance of a fistula with internal purulent accumulation. Severe pain covers the entire jaw row, the person’s general well-being deteriorates sharply. May cause damage to adjacent fragments.
By timing
According to the timing of the disease, it can be early or late:
- if self-rejection occurs within a month after the operation , it is considered short-term and is defined as the impossibility of fusion of the device with natural tissue;
- medium-term - rejection mechanisms are launched no earlier than six months later, or, in general, after a year or two . If there is no mechanical reason for this phenomenon, then the only factor provoking the situation will be bone delamination. This, in turn, is caused by incorrect calculation of the load on the tooth.
- if the problem manifests itself several years later, is a late type of anomaly. It occurs solely due to the fault of the patient, in particular, neglect of hygiene in caring for the implant.