Periostitis is a purulent disease, the focus of which is localized directly on the bone surface under the periosteum. The reason for its occurrence is a variety of pathogenic microflora, most often developing in the process of acute or chronic inflammation in the area of the apexes of the roots of teeth during periodontitis.
Periodontitis is inflammation in a very limited confined space. In the event of the formation of purulent exudate, the latter tries to find a way out, an outflow path. If it is not possible through the root canals or the gap between the tooth and the bone edges of the socket, a breakthrough occurs into the jaw’s own bone spaces. During the process of inflammation, the permeability of the walls of the bone socket of the tooth gradually increases - due to resorption and destruction of blood vessels, nerve fibers, etc. passing through this barrier.
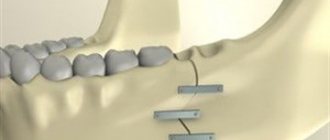
Scheme of formation of subperiosteal abscess, flux
From the bone spaces of the jaw, pus enters through the outer compact plate under the connective tissue periosteum. It becomes swollen and loose, and in some places loses its tight attachment to the bone. Scattered subperiosteal lesions quickly merge, forming a single cavity formation, which can significantly increase in size until emptying - through a fistula or through an incision.
Periostitis of the upper jaw occurs less frequently than the lower jaw. Most often, the causative teeth are the first molars, and the accumulation of pus is on the outside of the jaw in the area of the transitional fold. Less commonly, periostitis appears in the base of the nose, in exceptional cases on the palatal side of the dentition.
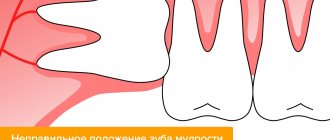
Periostitis of the lower jaw is more common, the most affected area is the outer surface of the jaw body near the molars. An additional cause, in addition to periodontitis, is inflammation caused by difficulties in the eruption of the lower third molar, the “wisdom tooth”.
Features of development
The following stages of development of this disease are distinguished:
- The infection from the diseased tooth spreads to the root and then to the bone tissue.
- Serous exudate forms in the bone tissue.
- The infection penetrates the periosteum through the vessels and nerves, exfoliating it.
- As the inflammatory process progresses, leukocytes appear in the serous exudate, and the process itself becomes purulent.
According to ICD 10, acute purulent periostitis of the lower or upper jaw has code K10.2. The number 10 indicates diseases of the jaw, and 2 indicates an inflammatory process in it, that is, periostitis in a purulent form.
Treatment
Treatment can be carried out using both conservative and radical methods. It should be noted that conservative therapy can only be used if the purulent process has not begun. In the latter case, urgent medical intervention is required.
For acute periostitis of the trunk bones, drug therapy may include taking the following drugs:
- antibiotics if the infectious nature of the disease is established;
- non-steroidal anti-inflammatory drugs;
- hydrocortisone;
- painkillers.
In addition to drug treatment, the doctor may prescribe the following physiotherapeutic procedures:
- electrophoresis with calcium chloride;
The issue of hospitalization is decided on an individual basis. However, if surgery is not required, treatment can be done at home.
In case of an odontogenic type of inflammatory process, drug therapy will include drugs with the following spectrum of action:
- antibacterial;
- general strengthening;
- antiallergic.
If a serous form of the inflammatory process is diagnosed, then medical measures are as follows:
- nerve removal;
- washing the wound with special antiseptic solutions to prevent the development of an infectious process;
- Antibacterial therapy – if necessary.
For the purulent form of the disease, the therapeutic measures are identical, however, the doctor may additionally prescribe physiotherapeutic procedures. If progression of the disease is observed, then the tooth is removed, and the wound itself is washed and drained.
The main causes of the disease
Periostitis in rare cases manifests itself as a separate ailment; most often it occurs against the background of other pathological processes in the oral cavity and larynx. Typically, the cause of this disease is chronic periodontitis in an advanced stage, as well as periodontitis, jaw cyst, alveolitis and inflammatory processes in the so-called wisdom teeth.
Leads to the accumulation of a large amount of pus, as a rule, and a bacterial infection, which occurs against the background of otitis media, influenza, tonsillitis, acute viral disease, measles, and scarlet fever.
Acute periostitis of the jaw can also occur when exposed to negative factors, which include:
- problems arising during tooth extraction;
- oral surgery;
- mechanical damage to the jaw resulting in wounds;
- the beginning of the inflammatory process in facial tissues;
- hypothermia or, conversely, overheating, severe physical exertion;
- eruption of the child's first teeth;
- improper treatment of dental diseases;
- reduced immunity.
The cause of acute purulent periostitis of the jaw can be pronounced, in which case it will be quite simple to diagnose it. But everything is much more complicated when there are no visible symptoms of the pathological condition.
The inflammatory process can appear as a result of exposure to negative factors. For example, after cured caries, a wound formed near the root of the tooth, which, due to low immunity, was exposed to bacteria. As a result of this process, the development of acute purulent periostitis of the jaw begins. When visiting a doctor, the patient must give him all the information that will help determine the cause of the illness. In this case, treatment will be prescribed effective and comprehensive.
Symptoms of periostitis
The general clinical picture of the disease in each patient will differ depending on the form of the lesion, the stage of development, the characteristics of the course, as well as the individual characteristics of the patient’s body.
The chronic form of the disease is usually sluggish, without pronounced symptoms. The acute form of the disease cannot be ignored, since it is most often accompanied by one or more pronounced symptoms that will not allow a person to work and rest normally.
Acute periostitis of the upper jaw can manifest itself as an independent disease or develop against the background of other diseases of the oral cavity. This is what will determine the symptoms, which will progress every day.
Doctors include the most common complaints about purulent periostitis of the upper jaw:
- severe and acute, in some cases, throbbing pain on one side, which radiates to the ear, temple or neck;
- problems with jaw mobility, which provoke severe pain when opening the mouth;
- swelling and swelling of a part of the face, depending on the area of pain, in some cases, problems with facial expressions arise;
- a purulent abscess near the root of the diseased tooth, which leads to a yellow and watery discharge, this condition occurs from time to time and can bring temporary relief;
- inflammatory processes in the oral mucosa, resulting in redness;
- an increase in temperature in some patients to 38-39 degrees, general malaise, feeling tired, chills;
- an increase in the size of the submandibular lymph nodes, severe pain in them.
What symptoms will accompany acute purulent periostitis of the upper and lower jaws will directly depend on the stage of development of the disease and its progression. In most cases, suppuration of the periosteum spreads to the lower lateral teeth, which provokes severe swelling of the submandibular area and cheeks. Of course, the medical history of acute purulent periostitis of the lower jaw will be different for each patient.
If inflammation develops in the upper jaw, then tissue hyperemia occurs near the lips and eyes. The face takes on pronounced uneven outlines, severe swelling and bluish discoloration of the skin occurs.
From the appearance of the first symptoms of the lesion to the formation of a large abscess, as a rule, several days pass. After this, the pain syndrome gradually intensifies, and overall health only worsens.
From time to time, a person’s condition may improve; this is typical for those cases when the abscess opens on its own. But this does not mean at all that you don’t have to visit a doctor; if you don’t start proper treatment and clean it, then pus will accumulate in the affected area of the oral cavity again.
Acute purulent periostitis of the jaw
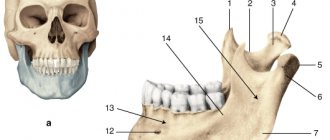
Acute purulent periostitis of the jaw is an acute purulent inflammation of the periosteum of the alveolar process or the body of the jaw. Most often, the periosteum of the alveolar processes is affected on the vestibular side of the jaws (85.6%), less often on the palatal side (palatal abscess) (5%) or the sublingual fold (9.4%). The process predominantly develops in the lower jaw and occurs in young and middle-aged individuals (from 16 to 40 years). In the lower jaw, the cause of the development of acute purulent periostitis is the first large molars, wisdom teeth, less often - the second large molars and the second small molars, sometimes the first small molars. The process can also develop from the first incisors and canines. In the upper jaw, acute purulent periostitis occurs when infection spreads from the first large molars, the first small molars and then the second small molars. Less commonly, the cause of the inflammatory process is the second large molars and second incisors, then the first incisors, canine, and wisdom teeth.
Etiology. When examining pus in the case of acute purulent periostitis, a mixed microflora is found, consisting of streptococci and staphylococci of various types, gram-positive and gram-negative bacilli and often putrefactive bacteria. Among them, up to 75% are anaerobic bacteria and 25% are aerobic flora.
Pathogenesis. Acute purulent periostitis is a complication of acute or chronic periodontitis, including marginal one. This process can also occur with difficult teething, suppuration of radicular cysts, inflammation of semi-impacted, impacted teeth, odontomas, periodontal diseases, and also complicate conservative dental treatment. Sometimes the disease develops after a traumatic tooth extraction or when an infection is activated after this intervention. General unfavorable factors - cold, overwork, stressful situations - serve as a background for the formation of the inflammatory process. In acute and aggravated chronic periodontitis, the purulent focus may not be emptied through the tooth canal or gum pocket, or the outflow through them may be insufficient. Exudate begins to spread from the periodontium towards the periosteum. The infection penetrates through small holes in the compact lamina of the alveoli along the nutrient canals and osteon canals. Changes in the alveolar wall, namely osteoclastic resorption, are of particular importance. Microorganisms can also spread from the periodontium to the periosteum through the lymphatic vessels. Violation of the integrity of periodontal tissues during acute and exacerbation of chronic periodontitis determines the functional insufficiency of nonspecific and specific humoral and cellular reactions to suppress infectious effects. Antigenic irritation increases sensitization, hemodynamics are disrupted. In this regard, inflammation in the periosteum of the jaw as a protective reaction manifests itself clearly and is characterized by a normergic, sometimes hyperergic inflammatory reaction. Due to the individual characteristics of the body's reactions (immunity imbalance), in some patients a sluggish course of periostitis of the jaw is noted, as well as a primary chronic form, reflecting a general hypergic or local hyperergic inflammatory reaction.
Pathological anatomy. With the development of an acute process in the periosteum, its thickening due to edema, disintegration and partial detachment from the underlying bone are macroscopically observed. Microscopically, it and the adjacent soft tissues are infiltrated with leukocytes, there are vascular changes (vascular congestion, stasis and areas of hemorrhage in certain places). Infiltrates of round and plasma cell elements are located around the vessels of the periosteum. Along with this, fibrinoid swelling (homogenization) of connective tissue fibers and vessel walls is possible. The inner layer of the periosteum quickly melts under the exfoliated periosteum, and serous-purulent exudate containing many neutrophilic leukocytes accumulates between it and the bone. In the serous exudate, leukocytes accumulate around microorganisms - microabscesses occur. These foci merge with each other, forming a significant mass of purulent exudate, which further exfoliates the periosteum (Fig. 7.11).
As a result of necrosis of the periosteum area and its subsequent melting, the integrity of the detachments from the bone of the inflamed periosteum is disrupted and purulent masses break through under the mucous membrane, most often the vestibule of the mouth. Around the periosteal perforation site, the vessels are often filled with purulent blood clots with partially destroyed walls. On the 5th-6th day, the abscess usually breaks through the mucous membrane into the oral cavity. In some cases, as a reflection of the intensity and severity of the process, axillary resorption of bone tissue is possible. Due to resorption of bone tissue, expansion of the brain cavities and nutrient canals, thinning of the cortical layer of the jaw occurs and even the formation of defects in it. This promotes the proliferation of leukocytes into bone tissue. At the same time, the bone marrow appears swollen, and in some areas of the bone marrow cavities there is leukocyte infiltration. Sometimes, with significant detachment of the periosteum by purulent exudate, the blood supply to the cortical layer can be disrupted and certain areas of the surface layers of the bone become necrotic. Secondary cortical osteomyelitis of the jaw develops. With this process, massive infiltration of fibrous structures of expanded bone marrow cavities by leukocytes is diagnosed (G.A. Vasiliev).
With the development of periostitis of the jaw against the background of repeated exacerbations of periodontitis in the bone and along the periphery of the subperiosteal abscess, periosteal new bone formation, compaction of the bone pattern, and bone sclerosis can be observed. Typically, these morphological changes occur in children, adolescents, and young healthy people and are interpreted as chronic periostitis (ostitis) of the jaw (Ya.M. Biberman, A.G. Shargorodsky, V.V. Roginsky).
The clinical picture of acute purulent periostitis of the jaw is varied and depends on etiological, pathogenetic factors, localization and extent of the inflammatory process. One should distinguish between acute serous, acute purulent limited, purulent diffuse, chronic periostitis. More often, damage to the periosteum on the vestibular surface of the jaws is observed. With purulent limited periostitis, damage to the periosteum of the alveolar process of the jaws is noted; in a diffuse process, it also affects the body of the lower jaw to its base. Acute serous periostitis on the vestibular side of the jaw in the first 1-3 days is characterized by pain and severe swelling of the surrounding soft tissues. Under the influence of thermal procedures, the pain intensifies, the cold soothes it for a while. When swelling occurs on the face and pus breaks through the mucous membrane, the pain decreases significantly. The vault of the oral vestibule is smoothed due to a dense, painless infiltrate. Percussion of the tooth is painful. The patient often notes that first there was pain in the tooth area, and after 1-2 days the soft tissues “swelled”. An incision along the vault of the vestibule of the mouth indicates plethora of tissues, but pus cannot be visually noted. If a tooth is removed, pus is released from the alveoli.
Limited purulent periostitis from the vestibular surface of the jaw is characterized by complaints of intense pain, swelling of the soft tissues of the face, impaired general health, and increased body temperature. At first, the pain and swelling are slight, then quickly, over 2-3 days, they intensify. The pain sometimes spreads to the entire jaw, radiating along the branches of the trigeminal nerve - to the ear, temple, eye.
The general condition of acute limited purulent periostitis is satisfactory, body temperature is elevated within 37.5-38 °C; with diffuse damage to the periosteum of the alveolar process and the body of the jaw - a state of moderate severity and body temperature up to 38.5-39 ° C. As a result of the resulting intoxication, general weakness, headache, weakness, loss of appetite, and insomnia appear. In acute purulent periostitis of the alveolar process, inflammatory swelling occurs on the vestibular side in the area of the soft tissues surrounding the jaw. Its localization and distribution depend on the tooth that was the source of infection. Thus, with periostitis, which has developed as a result of a purulent process in the upper incisors, there is significant swelling of the upper lip, spreading to the wings and bottom of the nose. The enlarged lip protrudes sharply forward. If the purulent process spreads from the upper canine and upper small molars, then the purulent focus can be localized in the periosteum covering the alveolar process and the area of the canine fossa; in this case, collateral edema covers a significant area of the middle and lower third of the face. The tissues of the cheek, cheekbone, lower and often upper eyelids swell. Acute periostitis, which developed as a result of a purulent process of the upper molars, is characterized by swelling of the cheek, zygomatic, parotid areas, reaching almost to the auricle. Sometimes the swelling spreads to the lower eyelid.
The third upper molar can serve as a source of infection, and periostitis occurs in the area of the tubercle of the upper jaw. Swelling on the face appears later than usual and is localized in the buccal and temporal areas.
Acute purulent periostitis, caused by the lower incisors, is characterized by swelling of the lower lip, chin area and sometimes the anterior part of the submental triangle. As the infection spreads from the canine and small molars, collateral swelling of the lower buccal region and corner of the mouth develops, descending into the submandibular triangle. With purulent periostitis in the area of large molars of the lower jaw, collateral swelling of the lower part of the buccal, submandibular and parotid-masticatory areas develops. The most pronounced general symptoms and local diffuse swelling of the tissues occur when the process spreads to the periosteum of the base of the lower jaw. The spread of the process to the periosteum of the lower jaw branch causes inflammatory infiltration of the masseter and medial pterygoid muscles, which leads to their inflammatory contracture (I, II degrees).
In acute purulent periostitis, regional lymphadenitis of varying degrees of severity is observed. In the vestibule of the mouth, there is hyperemia and swelling of the mucous membrane of the alveolar process, transitional fold and cheek over 3-5 teeth. Due to inflammatory infiltration, the transitional fold thickens, smoothes out, and upon palpation, a diffuse, painful, roll-like infiltrate is diagnosed. After 5-6 days, and sometimes earlier, the area of the periosteum breaks through as a result of necrosis and its melting under the influence of pus, which penetrates under the mucous membrane. The pain is significantly reduced. Along the transitional fold there is a limited swelling in the form of a roller, covered with a thin mucous membrane. Pus often shines through, giving a yellowish color to the mucous membrane; upon palpation, fluctuation is clearly visible. The abscess can spontaneously open into the oral cavity, after which the pain subsides and the inflammatory phenomena subside. With periostitis of the lower jaw from the lingual surface of the alveolar part, the patient experiences pain when swallowing and speaking.
Acute periostitis from the lingual surface of the alveolar part and the body of the lower jaw is characterized by collateral edema and enlarged lymph nodes in the submandibular triangle. Sometimes the swelling of the tissues of the buccal area is not clearly expressed. Mouth opening is free, but sometimes due to infiltration of the medial pterygoid muscle it can be painful and limited. When examining the oral cavity itself, swelling and infiltration of the periosteum in the inner surface of the jaw is recorded, and upon palpation in this area - pain. Swelling and hyperemia of the mucous membrane may appear in the area of the sublingual fold. Possible swelling of the palatoglossus and velopharyngeal arches. Movement of the tongue becomes difficult and painful, opening the mouth is limited and painful.
In case of acute purulent periostitis of the alveolar process of the upper jaw from the side of the oral cavity itself (palatal abscess), there are no changes on the face, enlarged submandibular lymph nodes are palpated. With a palatal abscess, a swelling is visible on the hard palate, which quickly takes on a hemispherical or oval shape. There is no significant inflammatory edema in its circumference due to the absence of a submucosal layer. The enlargement of the abscess leads to smoothing of the transverse palatal folds. On palpation, softening and fluctuation are determined in the central part of the infiltrate. A palatal abscess is characterized by the spread of inflammatory swelling from the hard palate to the mucous membrane of the soft palate, palatoglossus and velopharyngeal arches, resulting in pain when swallowing. The accumulation of purulent exudate under the periosteum of the hard palate causes exfoliation of soft tissues from the bone, which is accompanied by pain, often pulsating in nature, aggravated by talking and eating. A week or more after the onset of the disease, the abscess breaks out and pus pours into the oral cavity. Diagnosis of acute purulent periostitis of the jaw is based on clinical data and laboratory tests. In patients with acute purulent periostitis of the jaw, a blood test revealed an increased number of leukocytes to 10.0-12.0-109/l (in some patients the number of leukocytes was 8.0-9.0-1 C/l), significant neutrophilia (up to 70 -78%), ESR remains normal in a significant number of patients, sometimes increases to 15-20 mm/h, very rarely - up to 50-60 mm/h. An increase in ESR during the course of the disease may indicate a failure of surgical intervention or the development of secondary cortical osteomyelitis. There are basically no changes in the urine, only in some patients protein is detected - from traces to 0.33 g/l and leukocytes - 10-20 per field of view. There are no changes in the jaw bone on the x-ray.
Differential diagnosis. Despite the vivid clinical symptoms of acute purulent periostitis of the jaw, mistakes are sometimes made in its diagnosis. This process should be differentiated from acute periodontitis, abscesses of a number of localizations, phlegmons, lymphadenitis, acute sialadenitis and, most importantly, from acute osteomyelitis of the jaw. A.I. Evdokimov (1955) gives clear criteria for differentiating the disease: “Odontogenic periostitis as an independent nosological unit should be distinguished from diffuse acute periodontitis and osteomyelitis. The difference between periostitis and periodontitis is determined by the localization of the source of inflammation, when the latter occurs inside the socket, and periostitis occurs on the surface of the alveolar process. Collateral edema in periodontitis is limited to the gums, without spreading to soft tissues. The distinction between periostitis and osteomyelitis is justified by the nature of the clinical course and the absence of bone lesions during periostitis in the form of sequestration formation and microscopic changes in the bone structure.” In addition, in contrast to acute periodontitis, in acute periostitis of the jaw, pain sensitivity upon percussion of the tooth that was the source of infection is absent or insignificant. Inflammatory changes in the mucous membrane along the transitional fold in acute periodontitis occur in the form of edema, and in acute periostitis of the jaw - inflammatory infiltration. In acute periodontitis, unlike purulent periostitis, pus is not found when the periosteum is dissected. The differential diagnosis of acute periostitis of the jaw from purulent lesions of the salivary glands is based on the fact that during acute inflammation of the parotid and submandibular salivary glands, a dense, painful gland is palpated deep in the edematous tissues, and purulent secretion is released from its ducts.
Acute purulent periostitis must be differentiated from acute osteomyelitis of the jaw. Acute osteomyelitis of the jaw is characterized by severe intoxication of the body: a febrile type of temperature reaction, headache, fatigue, weakness, chills, sweat, etc. The reaction of the regional lymph nodes is more pronounced. Periosteal thickening of the bone is observed on both sides of the jaw: in the oral cavity, inflammatory changes in the mucous membrane occur both on the side of the vestibule and the oral cavity itself. Percussion of several teeth corresponding to the area of the affected bone is painful, and they are mobile. In the lower jaw with osteomyelitis, numbness of the lower lip and skin of the chin is diagnosed - Vincent's symptom.
Acute periostitis of the jaw is differentiated from purulent diseases of the perimandibular soft tissues - abscess, phlegmon, lymphadenitis. With periostitis, the tissues are swollen and soft to the touch; with abscess, phlegmon, lymphadenitis, dense limited or diffuse infiltration is palpated. When an abscess or phlegmon is located in the superficial areas of the face and neck adjacent to the upper and lower jaw, the skin over the infiltrate is welded together, shiny and hyperemic. When deep areas of the face are affected, perifocal edema is recorded in tissues visible during external examination, but unlike periostitis, there are no characteristic changes along the transitional fold.
Particular difficulties for the differential diagnosis are periostitis of the lower jaw on the lingual side and an abscess of the anterior part of the sublingual region or the posterior part - the maxillo-lingual groove. With purulent processes in the anterior and posterior parts of the sublingual space, an enlarged sublingual ridge is visible due to a dense and painful infiltrate. With an abscess of the maxillo-lingual groove, mouth opening is limited and swallowing is painful. At the same time, as with periostitis, the infiltrate is located along the alveolar process, mouth opening is often not limited.
Periostitis of the lower jaw on the lingual side can be mistaken for inflammation of the duct of the submandibular salivary gland, but when the salivary stone is located in the duct, the infiltrate is located along its course, and thick viscous saliva or purulent-mucous secretion is released from the outlet. By palpation, a foreign body (stone) can be identified and this can be further confirmed by x-ray. With periostitis, the localization of the infiltrate and the presence of clean saliva make it possible to refute the diagnosis of sialadenitis.
Treatment of acute purulent periostitis of the jaw should be complex and include surgical opening of the abscess, conservative drug therapy, etc. In the initial stage of acute periostitis of the jaw (acute serous periostitis), in some cases it is necessary to open the tooth cavity, remove decay from the canal and create conditions for outflow, and in others, to remove the tooth that is the source of infection. These therapeutic measures, carried out under infiltration or conduction anesthesia, together with incisions along the transitional fold to the bone, drug therapy (blockade with anesthetics, antibiotics, proteolytic enzymes, hormones) can help to subside the inflammatory phenomena.
In case of acute purulent periostitis of the jaw, emergency surgical intervention is indicated - opening the purulent subperiosteal focus and creating an outflow of exudate (primary surgical treatment of a purulent wound), which is usually carried out on an outpatient basis, sometimes in a hospital. Surgery for acute purulent periostitis is performed under local anesthesia - conduction or infiltration anesthesia, using a thin needle through which the anesthetic solution is injected slowly under the mucous membrane and the tissue is infiltrated along the intended incision line. The needle should not be inserted into the abscess cavity. Sometimes the operation is performed under anesthesia. Medicinal preparation of patients has a good effect. If the subperiosteal abscess is located in the area of the vestibule of the mouth, then it is better to make the incision with a beak-shaped scalpel parallel to the transitional fold through the entire infiltrated area; dissect the mucous membrane, submucosal tissue and periosteum to the bone, respectively, of 3-5 teeth. To prevent the edges of the wound from sticking together and to ensure the drainage of pus, a narrow strip of thin (glove) rubber is loosely inserted into the wound.
If the abscess is localized under the periosteum in the area of the tubercle of the upper jaw, the incision should be made along the transitional fold in the area of the molars of the upper jaw, but to open the inflammatory focus with a raspatory or grooved probe, one should pass from the wound along the bone in the direction of the tubercle of the upper jaw (back and inward). In the same way, a purulent focus is opened during periostitis of the upper jaw, passing upward with a probe towards the canine fossa.
It is recommended to open the inflammatory focus during periostitis from the lingual surface of the lower jaw by making an incision in the mucous membrane of the alveolar part to the bone, in the place of the greatest protrusion of the infiltrate. A grooved probe is passed down the surface of the bone and, pushing back the periosteum, allows the pus to drain out. For palatal abscess, the incision is made in the area of greatest tissue bulging, slightly away from the base of the alveolar process, or at the midline of the palate, parallel to it. Then a wide strip of thin (glove) rubber is inserted into the surgical wound, which avoids sticking of the edges of the wound and creates conditions for good outflow of pus. The best results will be obtained by excision of a small triangular-shaped section of the mucous membrane from the wall of the abscess, which ensures a freer outflow of pus. When opening an inflammatory focus in the area of the periosteum of the lower jaw branch on its outer and inner surface, special techniques are used. In case of periostitis on the inner surface of the jaw branch, an incision is made with a sickle-shaped scalpel with a limiter or a regular scalpel to the bone, tissue is dissected in the retromolar region (at the base of the palatoglossal arch), and a rasp is passed to the inner surface of the jaw branch, creating an outflow of exudate from the source of inflammation.
The subperiosteal abscess on the outer surface of the lower jaw branch should be opened with an incision made vestibular at the level of the 2nd and 3rd large molars along an oblique line to the bone, then with a rasp they pass subperiosteally in the direction of the angle of the lower jaw, retracting the masticatory muscle outward. After opening the lesion, a rubber strip must be inserted deeply into the wound for drainage. The lack of effect from such an intervention the next day is the basis for hospitalization and surgical intervention through external access. After opening the purulent focus, it is advisable to let the patient rinse the horn with a weak solution of potassium permanganate or 1-2% sodium bicarbonate solution, and also wash the wound with a solution of ethacridine lactate, gramicidin, chlorhexidine. A good effect is achieved by irrigating the abscess cavity with a solution of dimexide with oxacillin in 50 ml of distilled water and applying 40% dimexide liniment to the wound for 15 minutes.
If the tooth that was the source of infection is destroyed and does not represent functional or aesthetic value, then it should be removed simultaneously with the opening of the subperiosteal abscess. This will improve the emptying of the purulent focus and will contribute to a more rapid subsidence of inflammatory phenomena. In some cases, tooth extraction is postponed due to the expected technical difficulties of this operation or the unsatisfactory condition of the patient; in others, the tooth is preserved: its cavity is opened, the root canal is freed from decay products, and then conservative treatment of chronic periodontitis is carried out.
Drug treatment of acute purulent periostitis consists of prescribing drugs: sulfonamide (norsulfazole, sulfadimethoxine, sulfadimezin, etc.), nitrofuran (furazolidone, furadonin), antihistamine (diphenhydramine, suprastin, diazolin, etc.), calcium, pyrazolone derivatives (analgin, amidopyrine, phenacetin etc., as well as their combinations), vitamins (multivitamins, vitamin C 2-3 g per day). In recent years, they have begun to refuse to prescribe sulfonamide drugs due to the low sensitivity of the microflora to them, and if the patient’s condition requires more effective anti-inflammatory treatment, antibiotics and nitazol preparations are used. On the 2nd day after the operation, the patient is examined, the degree of subsidence of inflammatory phenomena is determined and, depending on this, additional treatment is prescribed. When dressings, local treatment of the wound is carried out. In case of acute purulent periostitis of the jaw, for a more rapid cessation of inflammatory phenomena on the 2nd day after opening the abscess, physical treatment methods should be prescribed: light and heat therapy (sollux lamp), warm baths of antiseptic or deodorizing solutions, ointment dressings (Dubrovin dressings, with Vaseline, 20% camphor oil, sea buckthorn oil, rose hips), UHF, microwave, fluoridation, laser therapy with helium-neon, infrared laser beams, exercise therapy.
In most cases, inflammatory phenomena quickly (after 2-3 days) subside. If the subsidence of inflammation is delayed, then 2-3 blockades are carried out: infiltration of the surrounding inflammatory tissues from the skin with 0.25-0.5% solutions, anesthetics - lidocaine or ultracaine 1.8-3.6 ml with isotonic sodium chloride solution (40- 50 ml) and antibiotic lincomycin. Some weakened patients, as well as those with increasing inflammation, are prescribed antibiotics. A prerequisite for the effectiveness of antibiotic therapy is opening the abscess (primary surgical treatment). Combination antibacterial therapy aimed at anaerobic and aerobic infection is recommended: lincomycin, macrolides (rulid, macropen, sumamed, azithromycin), broad-spectrum antibiotics (semi-synthetic penicillins, tetracycline, oletethrin, oxacillin), metronidazole derivatives, etc. Treatment in the clinic carried out within 5-6 days; In the hospital, injections of these drugs are given 3-4 times a day for 6-7 days.
Exodus. Timely initiation and proper treatment of acute purulent periostitis of the jaw ends in recovery. After 3-5 days, patients become able to work. With a palatal abscess, the thickness and density of the soft tissues detached from the palate do not allow the abscess to open spontaneously. This often leads to necrosis of the cortical parts of the bone and the development of secondary cortical osteomyelitis. Errors in treatment, progression of the inflammatory process in some patients cause chronicity of the disease, the occurrence of chronic periostitis or the spread of purulent exudate into the bone, the development of acute osteomyelitis of the jaw or into the perimandibular soft tissues with the formation of an abscess or phlegmon.
Prevention of acute periostitis of the jaw consists of sanitation of the oral cavity and treatment of chronic odontogenic lesions.
Did you like the article? Share with friends
0
Similar articles
Next articles
- Chronic periostitis of the jaw
- Assessment of the thickness of tissue removed during tooth preparation using the temporary crown method
- Separation and protection of adjacent teeth during preparation
- Odontogenic osteomyelitis of the jaw
- Acute stage of osteomyelitis of the jaw
Previous articles
- Treatment of chronic periodontitis
- Acute periodontitis
- Classification of periodontitis
- Local complications arising after tooth extraction
- Local complications arising during tooth extraction
Add a comment
Who suffers from the disease?
Purulent periostitis mainly affects adults, but during the eruption of the first teeth or during injury, the disease can develop even in childhood. Diagnosis in this case can be quite difficult due to the fact that the symptoms of the disease are very similar to osteomyelitis.
Although, there are also characteristic signs of the described illness: restlessness of the child, bad behavior, crying, problems sleeping, redness of the gums, swelling on one side, severe pain when touching the sore area and a sharp rise in temperature.
In most cases, the disease is observed in children 3-4 years old and has a severe course. You should seek help from a doctor as soon as possible, without delaying treatment of acute purulent odontogenic periostitis, as this can lead to quite dangerous pathologies.
Periostitis in children
If the disease occurs in a child due to a carious tooth, it is removed, thus eliminating the source of infection
The approach to the treatment of periostitis in childhood is practically no different from the treatment of adults.
If the disease occurs in a child due to a carious tooth, it is removed, thus eliminating the source of infection.
If it is necessary to preserve the tooth, an incision is made in the gum and drainage is installed to drain the pus.
At the same time, therapy is carried out using antibacterial drugs approved in childhood.
Main types of disease
Diagnosis of acute periostitis is carried out by comparing the symptoms characteristic of all types of this disease. Comparison helps determine the form of the pathology and create a comprehensive and effective treatment for a specific case.
According to genesis and distribution, the inflammatory process is divided into the following types:
- odontogenic – appears as a result of other oral diseases;
- traumatic - caused by mechanical damage to the jaw;
- lymphogenous - the infectious process invades the lymphatic system;
- hematogenous - infection spreads through the bloodstream.
The most common form of the disease appears in humans when exposed to odontogenic factors. But in rare cases, other types of diseases are also diagnosed, which are treated depending on the cause of their occurrence.
Development of the disease
Depending on the severity of the symptoms and severity of the lesion, dentists distinguish between acute and chronic periostitis. Chronic develops for a long time, and its symptoms are mild. With this disease, a person experiences an overgrowth of bone tissue in the area of the affected jaw, accompanied by progressive ossification. This process is almost irreversible and very dangerous. Only timely detection of inflammation of the periosteum will help prevent complications.
Acute periostitis is characterized by severe symptoms, therefore, as already mentioned, it is simply impossible not to notice the disease. There is a purulent and serous form of the pathology. With serous periostitis, a certain amount of serous fluid accumulates in the affected area of the mouth. For a purulent type of lesion, an abscess under the periosteum is considered characteristic. These two forms of pathology, if treated incorrectly or untimely, can quickly become chronic.
Classification
Simple periostitis is an aseptic process and occurs as a result of injuries (fractures, bruises) or inflammatory foci localized near the periosteum (in muscles, bones).
More often, areas of the periosteum covered with a thin layer of soft tissue are affected, for example, the olecranon or the anterior internal surface of the tibia.
A patient with periostitis complains of moderate pain. When examining the affected area, slight swelling of the soft tissues, local elevation and pain on palpation are revealed. Simple periostitis usually responds well to treatment. In most cases, the inflammatory process stops within 5-6 days. Less commonly, a simple form of periostitis develops into chronic ossifying periostitis. Fibrous periostitis occurs with prolonged irritation of the periosteum, for example, as a result of chronic arthritis, bone necrosis or chronic trophic ulcer of the leg.
Characterized by a gradual onset and chronic course.
The patient's complaints are usually caused by the underlying disease. In the affected area, slight or moderate swelling of the soft tissues is detected; upon palpation, a dense, painless thickening of the bone is determined. With successful treatment of the underlying disease, the process regresses. With a long course of periostitis, superficial destruction of bone tissue is possible; there is evidence of isolated cases of malignancy of the affected area. Purulent periostitis develops when infection penetrates from the external environment (with wounds with damage to the periosteum), with the spread of microbes from a neighboring purulent focus (with a purulent wound, phlegmon, abscess, erysipelas, purulent arthritis, osteomyelitis) or with pyaemia. Usually the causative agent is staphylococcus or streptococcus. The periosteum of long tubular bones - humerus, tibia or femur - is most often affected. With pyemia, multiple lesions are possible. At the initial stage, the periosteum becomes inflamed, serous or fibrinous exudate appears in it, which subsequently turns into pus. The inner layer of the periosteum becomes saturated with pus and separates from the bone, sometimes over a considerable length. A subperiosteal abscess forms between the periosteum and the bone. Subsequently, several flow options are possible. In the first variant, the pus destroys a section of the periosteum and breaks into the soft tissues, forming a paraosseous phlegmon, which can subsequently either spread to the surrounding soft tissues or break out through the skin. In the second variant, the pus exfoliates a significant area of the periosteum, as a result of which the bone is deprived of nutrition and an area of superficial necrosis is formed. In case of unfavorable development of events, necrosis spreads into the deep layers of the bone, pus penetrates into the bone marrow cavity, and osteomyelitis occurs. Purulent periostitis is characterized by an acute onset. The patient complains of intense pain. The body temperature is elevated to febrile levels, chills, weakness, fatigue and headache are noted. When examining the affected area, swelling, hyperemia and sharp pain on palpation are revealed. Subsequently, a center of fluctuation is formed. In some cases, erased symptoms or a primarily chronic course of purulent periostitis are possible. In addition, acute or malignant periostitis is distinguished, characterized by a predominance of putrefactive processes. With this form, the periosteum swells, easily collapses and disintegrates, and the bone deprived of periosteum is shrouded in a layer of pus. Pus spreads to soft tissues, causing cellulitis. Septicopyemia may develop. Serous albuminous periostitis usually develops after injury, most often affecting the metadiaphyses of long bones (femur, shoulder, fibula and tibia) and ribs.
It is characterized by the formation of a significant amount of viscous serous-mucosal fluid containing a large amount of albumin.
Exudate can accumulate subperiosteally, form a cyst-like sac in the thickness of the periosteum, or be located on the outer surface of the periosteum. The area of exudate accumulation is surrounded by red-brown granulation tissue and covered with a dense membrane. In some cases, the amount of liquid can reach 2 liters. With subperiosteal localization of the inflammatory focus, detachment of the periosteum is possible with the formation of an area of bone necrosis. The course of periostitis is usually subacute or chronic. The patient complains of pain in the affected area. At the initial stage, a slight increase in temperature is possible. If the lesion is located near a joint, restriction of movement may occur. Upon examination, swelling of the soft tissues and pain on palpation are revealed. The affected area is compacted at the initial stages, and subsequently a softening area is formed and fluctuation is determined. Ossifying periostitis.
A common form of periostitis that occurs with prolonged irritation of the periosteum.
It develops independently or is a consequence of a long-term inflammatory process in the surrounding tissues. Observed in chronic osteomyelitis, chronic varicose ulcers of the leg, arthritis, osteoarticular tuberculosis, congenital and tertiary syphilis, rickets, bone tumors and Bamberger-Marie periostosis (a symptom complex that occurs in certain diseases of the internal organs, accompanied by thickening of the nail phalanges in the form of drumsticks and deformation of nails in the form of watch glasses). Ossifying periostitis is manifested by the proliferation of bone tissue in the area of inflammation. Stops progressing with successful treatment of the underlying disease. If it persists for a long time, in some cases it can cause synostosis (fusion of bones) between the bones of the tarsus and wrist, tibia or vertebral bodies. Tuberculous periostitis, as a rule, is primary, most often occurs in children and is localized in the area of the ribs or skull.
The course of such periostitis is chronic.
The formation of fistulas with purulent discharge is possible. Syphilitic periostitis can be observed with congenital and tertiary syphilis.
In this case, the initial signs of damage to the periosteum in some cases are detected already in the secondary period. At this stage, small swellings appear in the periosteum area and sharp flying pains occur. In the tertiary period, as a rule, the bones of the skull or long tubular bones (usually the tibia) are affected. A combination of gummous lesions and ossifying periostitis is observed; the process can be either limited or diffuse. Congenital syphilitic periostitis is characterized by ossifying lesions of the diaphyses of tubular bones. Patients with syphilitic periostitis complain of intense pain that worsens at night. Palpation reveals a round or fusiform limited swelling of dense elastic consistency. The skin over it is not changed, palpation is painful. The outcome may be spontaneous resorption of the infiltrate, proliferation of bone tissue, or suppuration with spread to nearby soft tissues and the formation of fistulas.
Degrees of the disease
Conventionally, the disease, depending on the area of distribution, in dentistry is divided into diffuse and organic degrees.
The latter is characterized by inflammation of 1-3 teeth, while with diffuse lesions can spread to almost the entire jaw. In dentistry, the diffuse form of pathology is quite rare and is characterized by its unpredictability.
This classification of periostitis helps the specialist make an accurate diagnosis, and then prescribe effective and comprehensive treatment for the pathology.
Treatment
Treatment goals: · elimination of the inflammatory focus; · relief of symptoms of intoxication; · restoration of jaw function; · prevention of complications.
Treatment tactics [ 1,6,7,10,11,12 ] . 1. Clinical and x-ray examination; 2. Surgical treatment; 3. Drug treatment; 4. Preventive measures; 5. Other types of treatment (physiotherapy, exercise therapy, massage, etc.).
Non-drug treatment: · The regimen in the early postoperative period is semi-bed, in the postoperative period it is general. With conservative treatment - general. · Diet table - after surgical treatment - No. 1a, 1b, subsequently No. 15.
Drug treatment:
| № | Drug, release forms | Dosing | Duration and purpose of use |
| Antibiotic prophylaxis | |||
| 1 | Cefazolin powder for solution for injection 500 mg and 1000 mg | 1 g IV (children at the rate of 50 mg/kg once) | 1 time 30-60 minutes before the skin incision; for surgical operations lasting 2 hours or more - an additional 0.5-1 g during surgery and 0.5-1 g every 6-8 hours during the day after surgery to prevent inflammatory reactions |
| 2 | Cefuroxime + Metronidazole Cefuroxime powder for solution for injection 750 mg and 1500 mg Metronidazole solution for infusion 0.5% - 100 ml | Cefuroxime 1.5-2.5 g, IV (for children at the rate of 30 mg/kg once) + Metronidazole (for children at the rate of 20-30 mg/kg once) 500 mg IV | 1 hour before the incision. If the operation lasts more than 3 hours, repeat after 6 and 12 hours similar doses, in order to prevent inflammatory reactions |
| If you are allergic to β-lactam antibiotics | |||
| 3 | Vancomycin powder for solution for infusion 500 mg and 1000 mg | 1 g IV (for children at the rate of 10-15 mg/kg once) | 1 time 2 hours before the skin incision. No more than 10 mg/min is administered; the duration of infusion should be at least 60 minutes in order to prevent inflammatory reactions |
| Opioid analgesics | |||
| 4 | Tramadol solution for injection 100mg/2ml 2 ml or 50 mg orally | Adults and children over 12 years of age are administered intravenously (slow drip), intramuscularly at 50-100 mg (1-2 ml of solution). If there is no satisfactory effect, an additional administration of 50 mg (1 ml) of the drug is possible after 30-60 minutes. The frequency of administration is 1-4 times a day, depending on the severity of the pain syndrome and the effectiveness of therapy. The maximum daily dose is 600 mg. Contraindicated in children under 12 years of age. | for pain relief in the postoperative period, 1-3 days |
| 5 | Trimeperidine injection solution 1% 1 ml | 1 ml of 1% solution is administered intravenously, intramuscularly, subcutaneously; if necessary, it can be repeated after 12-24 hours. The dosage for children over 2 years of age is 0.1 - 0.5 mg/kg body weight, if necessary, repeated administration of the drug is possible. | for pain relief in the postoperative period, 1-3 days |
| Nonsteroidal anti-inflammatory drugs | |||
| 6 | Ketoprofen solution for injection 100 mg/2 ml 2 ml or orally 150 mg prolonged 100 mg. | The daily dose for intravenous injection is 200-300 mg (should not exceed 300 mg), followed by oral administration of prolonged capsules 150 mg 1 time per day, caps. tab. 100 mg twice a day | The duration of treatment with IV should not exceed 48 hours. The duration of general use should not exceed 5-7 days, for anti-inflammatory, antipyretic and analgesic purposes. |
| 7 | Ibuprofen suspension for oral administration 100 mg/5 ml 100 ml or orally 200 mg; granules for solution for oral administration 600 mg | For adults and children over 12 years of age, ibuprofen is prescribed 200 mg 3-4 times a day. To achieve a rapid therapeutic effect in adults, the dose can be increased to 400 mg 3 times a day. Suspension - a single dose is 5-10 mg/kg of the child’s body weight 3-4 times a day. The maximum daily dose should not exceed 30 mg per kg of body weight of the child per day. | No more than 3 days as an antipyretic. No more than 5 days as an analgesic with anti-inflammatory, antipyretic and analgesic purposes. |
| 8 | Paracetamol 200 mg or 500 mg; suspension for oral administration 120 mg/5 ml or rectally 125 mg, 250 mg, 0.1 g | Adults and children over 12 years of age weighing more than 40 kg: single dose - 500 mg - 1.0 g (1-2 tablets) up to 4 times a day. The maximum single dose is 1.0 g. The interval between doses is at least 4 hours. The maximum daily dose is 4.0 g. Children from 6 to 12 years old: single dose – 250 mg – 500 mg, 250 mg – 500 mg up to 3-4 times a day. The interval between doses is at least 4 hours. The maximum daily dose is 1.5 g - 2.0 g. | The duration of treatment when used as an analgesic and as an antipyretic is no more than 3 days. |
| Hemostatic agents | |||
| 9 | Etamsylate solution for injection 12.5% - 2 ml | 4-6 ml of 12.5% solution per day. For children, a single dose of 0.5-2 ml is administered intravenously or intramuscularly, taking into account body weight (10-15 mg/kg). | If there is a risk of postoperative bleeding, it is administered for prophylactic purposes. |
| Antibacterial drugs | |||
| 10 | Amoxicillin clavulanic acid (drug of choice) | Intravenously Adults: 1.2 g every 6-8 hours. Children: 40-60 mg/kg/day (for amoxicillin) in 3 injections. | With the development of odontogenic periostitis and osteomyelitis, the course of treatment is 7-10 days |
| 11 | Lincomycin (alternative drug) | Use intramuscularly, intravenously (drip only). It cannot be administered intravenously without prior dilution. Adults: 0.6-1.2 every 12 hours. Children: 10-20 mg/kg/day in 2 administrations. | With the development of odontogenic periostitis and osteomyelitis, the course of treatment is 7-10 days |
| 12 | Ceftazidime (if P. aeruginosa is isolated) or | Intravenously and intramuscularly Adults: 3.0 - 6.0 g/day in 2-3 injections (for Pseudomonas infection - 3 times a day) Children: 30-100 mg/kg/day in 2-3 injections; | With the development of odontogenic periostitis and osteomyelitis, the course of treatment is 7-10 days |
| 13 | Ciprofloxacin (for P. aeruginosa isolation) | Intravenously Adults: 0.4-0.6 g every 12 hours. Administered by slow infusion over 1 hour. Contraindicated in children. | With the development of odontogenic periostitis and osteomyelitis, the course of treatment is 7-10 days |
Features of therapy
Treatment of the disease must be comprehensive. When initial symptoms of jaw inflammation appear, it is important to immediately seek help from a doctor. He will conduct a visual inspection, which will reveal the area of the lesion. To clarify the diagnosis, it is important to conduct a blood test in the laboratory. With the development of a purulent process, the level of leukocytes and ESR will be high.
The most effective diagnostics is considered to be thermography, which uses infrared radiation. With its help, the specialist is able to identify the inflammatory process and the place of its spread. Additionally, the doctor takes x-rays of diseased teeth and identifies all possible additional diseases.
Treatment of acute purulent periostitis is carried out through surgery. In any case, it is important to open the abscess without fail, and then remove all the contents from it.
To do this, the doctor makes a small incision in the area of the affected gum, removes the diseased tissue and installs a special drainage to drain the accumulated pus. The operated area must first be anesthetized with trimecaine or lidocaine.
At the initial stage of the disease, it is customary to use gum irrigation; in more complex situations, local anesthesia is used. Opening the flux yourself is strictly prohibited, as this can only worsen the situation.
Possible consequences
If you consult a dentist in a timely manner, the tooth can be saved. It is treated and then filled. In advanced cases, the inflammatory process is so widespread that the doctor has to remove the tooth.
Therapy may continue for several months. In some cases, due to severe pain in the patient, the abscess is first treated and only after that the dentist begins to treat the teeth themselves. The time of therapy will directly depend on the stage of the disease, the size of the affected area and the characteristics of the pathological process.
At the second stage of therapy, the doctor prescribes medications that help healing. To do this, use antiseptic and cleansing rinses with a warm solution of potassium permanganate or soda. Most often, a doctor prescribes antibiotics to eliminate a bacterial infection. For severe pain, analgesics are used. The specialist may also prescribe anti-inflammatory drugs, antihistamines, vitamins and minerals.
During rehabilitation, the patient is prescribed physical procedures: UHF, neon irradiation, laser therapy, and ultrasound. To improve the condition of the facial muscles, you need to use special therapeutic exercises.
Therapy for the acute form of periostitis at the initial stage of its development lasts only 3-5 days, including surgery and rehabilitation of the patient. If you follow all the doctor’s advice, a person will completely get rid of the problem and continue to live a full life.
At an advanced stage of the disease, longer and more complex treatment is required. The transition of the pathology to a chronic form provokes irreversible changes and regular relapses in the tissues of the periosteum. In this case, the doctor must constantly monitor the patient’s condition and prescribe periodic treatment.
Patients in reviews say that there is no need to be afraid to visit a doctor. A cured disease will help improve your health without large financial costs. But you should not treat damage to the oral cavity yourself, as this can only worsen the condition and lead to irreversible complications.
The outcome will depend on the patient's individual medical history of acute purulent periostitis of the upper jaw.
Diagnostics
Confirmation of the diagnosis is made using radiography
If symptoms of periostitis occur, you should immediately consult a doctor.
Medical intervention is mandatory, as otherwise the risk of complications increases.
To diagnose and treat periostitis, you must consult a dentist.
The doctor examines the patient’s complaints, which allows him to assume the nature of the disease.
During a dental examination, the external symptoms of gumboil are determined: swelling of the tissues, discoloration of the gums, the presence of a fistulous tract. Palpation checks the pain sensitivity of the affected area.
Confirmation of the diagnosis is made using radiography. This method allows you to detect changes in bone tissue caused by inflammation of the periosteum.
The clinical manifestations of periostitis are in many ways similar to other dental diseases.
These include:
The main distinguishing feature of periostitis is the localization of the inflammatory process
Periodontitis;
Also, symptoms of periodontitis may be mistaken for signs of lymphadenitis, sialadenitis, which emphasizes the need for differential diagnosis.
The main distinguishing feature of periostitis is the localization of the inflammatory process.
The affected area is located in the tissues of the periosteum, while in other diseases it is located higher. Swelling with periostitis is less pronounced than with periodontitis.
The difference from osteomyelitis is that the inflammatory infiltrate collects only on one side of the periosteum. Unlike sialadenitis, periostitis is not accompanied by inflammation of the salivary glands.
Reviews from patients
Patients note that to treat the disease at the first stage of its development, only about 660 rubles will be required (opening the abscess). Additional costs are needed to treat complications after periodontitis or pulpitis that appear with advanced periostitis. Tooth extraction will cost 1500-2000 rubles.
Additional expenses include x-rays, anesthetics and antibiotics taken, and in some cases hormonal drugs. With complex treatment, the patient may need about 5,000 rubles, and sometimes more. Therefore, those who have suffered periostitis are advised not to postpone a visit to the dentist.