999 06/18/2019 4 min. Periodontal diseases are widespread, so it is necessary to use advanced methods to make the most accurate diagnoses and differentiate one pathology from another. For this reason, various periodontal indices have been developed that make it possible to monitor the dynamics of pathology development over a given time period, assess the prevalence and depth of the pathological process, and compare the effectiveness of different treatment methods. In this review we will talk about this method of research as the Schiller-Pisarev test, its advantages, disadvantages and features.
Determination of the diagnostic method - Schiller-Pisarev test in dentistry
The high prevalence of periodontal pathologies and the need for their objective diagnosis in dentistry have led to the emergence of a whole set of indices. These indices are aimed at monitoring the dynamics of the disease over a certain time period, assessing the depth and extent of the pathological process, allowing one to compare the effectiveness of the therapeutic methods used, and processing the results mathematically.
There are several types of periodontal indices - complex, irreversible, reversible.
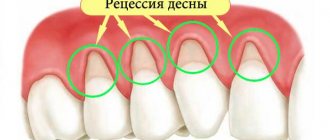
Reversible indices assess the dynamics of the pathological process and the effectiveness of the treatment methods used. They are calculated taking into account indicators, pocket depth, and tooth mobility. Irreversible characterizes the degree of bone tissue resorption and gum atrophy. Complex ones allow for a comprehensive assessment of the condition of periodontal tissues.
The Schiller-Pisarev test assumes intravital staining of gum glycogen - the content of this component increases significantly with. That is, intense staining of the gums indicates that it is inflamed. The test can also be used after completion of a course of treatment and to draw up a further course of action.
The Schiller Pisarev test is carried out for the purpose of
Its principle is to stain the gum glycogen with Schiller-Pisarev solution (reaction with iodine). During inflammation, glycogen accumulates in the gums due to keratinization of the epithelium.
Therefore, when interacting with iodine, inflamed gums are stained more intensely than healthy ones. It takes on shades from light brown to dark brown.
More intense coloring indicates a greater degree of inflammation.
The Schiller-Pisarev test is carried out as follows: dry the examined area of the gum with a cotton swab, isolate it from saliva and lubricate it with a cotton ball soaked in Lugol's solution or Schiller-Pisarev solution. The Schiller-Pisarev test is used in children to detect gingivitis.
To do this, the gums are stained with the following solution: potassium iodide – 2.0 crystalline iodine – 1.0 distilled water – up to 40.0. Healthy gums are not stained by this solution.
A change in its color under the influence of this solution occurs during inflammation, and then the test is considered positive.
PMA index - Papillary - Marginal - Alveolar index.
To assess the severity of gingivitis and record the dynamics of inflammatory processes in the gums, the PMA index is used. The condition of the gums of each tooth is assessed visually after staining it with Schiller-Pisarev solution. In this case, the inflamed areas of the gums acquire a brown color due to the presence of glycogen in them.
The RMA index is assessed using the following codes and criteria:
0 – no inflammation (the gums are not stained with Schiller-Pisarev solution)
1 – inflammation of only the gingival papilla (P)
2 – inflammation of the marginal gum (M)
3 – inflammation of the alveolar gum (A)
The PMA index is equal to the sum of the points of the examined teeth divided by the product of the number 3 by the number of examined teeth as a percentage.
The PMA index is calculated using the formula: PMA = (sum of points) / (3 * number of teeth examined) * 100%
The amount of tooth integrity, while maintaining the integrity of the dentition, is taken into account depending on age:
6 – 11 years – 24 teeth
12 – 14 years – 28 teeth
15 years and older – 30 teeth
If there are missing teeth, then divide by the number of teeth present in the oral cavity.
Ideally, the PMA index tends to zero. The higher the digital value of the index, the higher the intensity of gingivitis.
Evaluation criteria for the RMA index:
Ó 30% or less – mild severity of gingivitis
Periodontal diseases are widespread, so it is necessary to use advanced methods to make the most accurate diagnoses and differentiate one pathology from another.
For this reason, various periodontal indices have been developed that make it possible to monitor the dynamics of pathology development over a given time period, assess the prevalence and depth of the pathological process, and compare the effectiveness of different treatment methods.
In this review we will talk about this method of research as the Schiller-Pisarev test, its advantages, disadvantages and features.
Determination of the diagnostic method - Schiller-Pisarev test in dentistry
The high prevalence of periodontal pathologies and the need for their objective diagnosis in dentistry have led to the emergence of a whole set of indices.
These indices are aimed at monitoring the dynamics of the disease over a certain time period, assessing the depth and extent of the pathological process, allowing one to compare the effectiveness of the therapeutic methods used, and processing the results mathematically.
There are several types of periodontal indices - complex, irreversible, reversible.
Reversible indices assess the dynamics of the pathological process and the effectiveness of the treatment methods used. They are calculated taking into account indicators of bleeding gums and bad breath, pocket depth, and tooth mobility. Irreversible characterizes the degree of bone tissue resorption and gum atrophy. Complex ones allow for a comprehensive assessment of the condition of periodontal tissues.
The Schiller-Pisarev test involves intravital staining of gum glycogen - the content of this component increases significantly during periodontal inflammation. That is, intense staining of the gums indicates that it is inflamed. The test can also be used after completion of a course of treatment and to draw up a further course of action.
Advantages and disadvantages
An important component of implantation at all stages is an accurate index assessment of the condition of peri-implant tissues, implants and supported prostheses.
The Schiller-Pisarev test is quite effective and allows you to diagnose a wide range of conditions - gum inflammation, periodontal destruction, the amount of tartar, plaque, the need for certain therapeutic measures and their volume.
The relationship between the elements of the implant and adjacent tissues and its difference from a natural tooth may make complex periodontal studies impossible.
The Schiller-Pisarev test is quite accurate and objective and has two interpretation options. The first is visual, based on the nature of the gum staining, the second is numerical, that is, index. The problem with the methodology is that dental indices from 30-50 years ago do not meet the current needs of modern implantology.
That is, they can be used, but when interpreting the results, it will be necessary to take into account the full list of current changes and improvements in the field of prosthetics.
At the same time, it is the Schiller-Pisarev test that is considered the most informative of all similar diagnostic methods and allows the results to be most successfully adapted to the conditions of endosseous implantation.
However, the convention of numerical values still does not disappear anywhere, since diagnostics are carried out using markers, and not high-precision digital equipment. Modern researchers say that the Schiller-Miller test is still relevant, but should be used with certain modifications and clarifications.
How is the procedure performed?
The essence of the Schiller-Pisarev test is to lubricate the gums with a solution of iodine and potassium. As a result, areas with deep connective tissue lesions become stained - this is due to the accumulation of large volumes of glycogen in areas of inflammation.
The tests are repeated from time to time - if the treatment is carried out correctly, the condition of the gums will improve, and the inflammation will subside or disappear altogether.
That is, if the therapy is correct, then repeated tests should be weakly positive or negative.
Gum staining is due to the high amount of glycogen. When the inflammation passes, there is less glycogen, and the tissues cease to be intensely stained. In this way, the intensity and degree of development of the disease is determined.
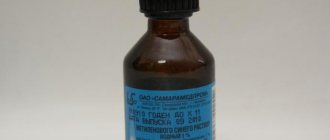
Composition of the solution
To take Schiller-Pisarev samples, the composition of the solution is used in the following proportions:
- crystalline iodine – 1.0;
- potassium iodide – 2.0;
- distilled water – 40.0.
Similar article – Are diseases transmitted through oral sex?
Before using therapeutic and prophylactic toothpaste (Parodontax, Parodontol paste), the gum mucosa is lubricated with a special solution, then the degree of staining is determined, and the data obtained is recorded in the disease history. Control – after 1, 2, 3, 6 and 12 months.
Result: index calculation, assessment of gum condition
For objectification purposes, the Schiller-Pisarev test is expressed in numbers (scores). The color of the papillae is rated at 2 points, the gingival margins at 4, and the gingival alveoli at 8 points. The total amount obtained is then divided by the number of teeth in the study area. That is, the calculation formula looks like this:
Iodine number = Sum of assessments for each tooth / Number of teeth examined.
The result is an iodine number in points. Evaluation of results by points:
- mild inflammation – up to 2.3 points;
- moderate inflammation – 2.67-5.0 points;
- severe inflammation – 5.33-8.0 points.
The peripheral circulation index (abbreviated as IPC) is also determined separately, taking into account the ratio of the time of resorption of hematomas that appeared under vacuum and the resistance of gingival capillaries. Test indicators are assessed in points, their ratio is expressed as a percentage. The index is calculated using the following formula:
- resistance of gum capillaries (scores);
- period of hematoma resorption (scores).
Based on index indicators, the functional state of the peripheral circulatory system is assessed. An IPC from 0.8 to 1.0 is considered normal, 0.6-0.7 is a good condition, 0.075-0.5 is a satisfactory condition, and from 0.01 to 0.074 is a decompensated state. You may be interested in learning how to strengthen teeth with periodontal disease.
The point system used to calculate the IPC (points are points)
| Resistance of gum capillaries | Period of resorption of vacuum hematomas |
| 1-10 seconds, 1 b. | 2.5 days, 10 b. |
| 11-20 seconds, 2 b. | 3 days, 20 b. |
| 21-30 seconds, 4 b. | 3.5 days, 40 b. |
| 31-40 seconds, 6 b. | 4 days, 60 b. |
| 41-50 seconds, 8 b. | 4.5 days, 80 b. |
| from 50 seconds, 10 b. | 5 days, 100 b. |
For more information about diagnosing and treating periodontal disease, watch the video
conclusions
- To diagnose periodontal diseases and evaluate the effectiveness of treatment, various methods are used, including periodontal indices.
- The essence of the Schiller-Pisarev technique is to stain the gums.
Areas deeply affected by the inflammatory process will become stained. Based on the intensity of staining, the stage of the pathology can be determined. It also allows you to distinguish periodontal disease from other similar pathologies. For more information on how periodontitis differs from periodontal disease, see this material. - The Schiller-Pisarev test involves two interpretation options - visual, based on the nature of gum staining, and numerical or index.
- To take Schiller-Pisarev samples, a solution of potassium iodide, crystalline iodine and distilled water is used.
- The main index indicators are the resistance of gum capillaries and the time of resorption of vacuum hematomas.
Periodontist: what he treats and what he does during the appointment
Characteristic signs and features of the course of acute gingivitis
Orthopantomography of the dentition: how it is done and why it is needed in dentistry
Chronic periodontitis: signs of periodontal disease and its treatment
RMA index. — Schiller-Pisarev test. — Gingival index GI. — Communal periodongal index CPI. — Complex periodongal index KPI. — Gum recession index. — Gingival attachment loss index. — Diagnosis of risk factors for the development of periodontal pathology and drawing up a plan of preventive measures.
When assessing the condition of the periodontium using visual and tactile methods, pay attention to the condition of the gums (color, size, shape, density, bleeding), the presence and location of the periodontal junction relative to the enamel-cementum border (i.e., the presence and depth of pockets), on tooth stability.
To standardize and simplify registration records produced for clinical and epidemiological purposes, in our country and in the world it is common to use gingival and periodontal indices, which more or less fully describe the condition of the entire periodontium or its “sign” areas.
Schiller-Pisarev test
Designed to clarify the boundaries and degree of inflammation using vital tissue staining.
During inflammation, glycogen accumulates in the tissues, the excess of which can be detected by a qualitative reaction with iodine: a few seconds after the application of an iodine-containing preparation (most often this is Schiller-Pisarev solution), the tissues of the inflamed gums change their color in the range from light brown to dark brown. depending on the amount of glycogen, i.e. on the severity of inflammation.
Similar article – Read the Chichagov method
The sample can be assessed as negative (straw-yellow color), weakly positive (light brown color) or positive (dark brown color).
This test cannot be used to diagnose periodontal pathology in children under 6 years of age, since their healthy gums contain a large amount of glycogen.
Gingival index GI (Loe, Silness, 1963)
The index involves assessing the condition of the periodontium based on clinical signs of gum inflammation - hyperemia, swelling and bleeding when touched with an atraumatic probe in the area of six teeth: 16, 21, 24, 36, 41, 44.
The condition of four areas of the gums near each tooth is studied: the medial and distal papilla on the vestibular side, the edge of the gums on the vestibular and lingual sides.
The condition of each section of the gum is assessed as follows: 0 - gums without signs of inflammation; 1 - slight discoloration, slight swelling, no bleeding during examination (mild inflammation); 2 - redness, swelling, bleeding during examination (moderate inflammation);
3 - severe hyperemia, edema, ulceration, tendency to spontaneous bleeding (severe inflammation).
Source: https://lechenie-nog.info/proba-shillera-pisareva-provoditsja-s-celju/
Advantages and disadvantages
An important component of implantation at all stages is an accurate index assessment of the condition of peri-implant tissues, implants and supported prostheses. The Schiller-Pisarev test is quite effective and allows you to diagnose a wide range of conditions - this is periodontal destruction, the amount of tartar, plaques, the need for certain therapeutic measures and their volume.
The relationship between the elements of the implant and adjacent tissues and its difference from a natural tooth may make complex periodontal studies impossible.
The Schiller-Pisarev test is quite accurate and objective and has two interpretation options. The first is visual, based on the nature of the gum staining, the second is numerical, that is, index. The main problem of the technique is that dental indices from 30-50 years ago do not meet the current needs of modern implantology.
That is, they can be used, but when interpreting the results, it will be necessary to take into account the full list of current changes and improvements in the field of prosthetics. At the same time, it is the Schiller-Pisarev test that is considered the most informative of all similar diagnostic methods and allows the results to be most successfully adapted to the conditions of endosseous implantation. However, the convention of numerical values still does not disappear anywhere, since diagnostics are carried out using markers, and not high-precision digital equipment. Modern researchers say that the Schiller-Miller test is still relevant, but should be used with certain modifications and clarifications.
Schiller test in dentistry. Functional tests
> Family
Periodontal diseases are widespread, so it is necessary to use advanced methods to make the most accurate diagnoses and differentiate one pathology from another.
For this reason, various periodontal indices have been developed that make it possible to monitor the dynamics of pathology development over a given time period, assess the prevalence and depth of the pathological process, and compare the effectiveness of different treatment methods.
In this review we will talk about this method of research as the Schiller-Pisarev test, its advantages, disadvantages and features.
Determination of the diagnostic method - Schiller-Pisarev test in dentistry
The high prevalence of periodontal pathologies and the need for their objective diagnosis in dentistry have led to the emergence of a whole set of indices.
These indices are aimed at monitoring the dynamics of the disease over a certain time period, assessing the depth and extent of the pathological process, allowing one to compare the effectiveness of the therapeutic methods used, and processing the results mathematically.
There are several types of periodontal indices - complex, irreversible, reversible.
Reversible indices assess the dynamics of the pathological process and the effectiveness of the treatment methods used. They are calculated taking into account indicators of bleeding gums and bad breath, pocket depth, and tooth mobility. Irreversible characterizes the degree of bone tissue resorption and gum atrophy. Complex ones allow for a comprehensive assessment of the condition of periodontal tissues.
The Schiller-Pisarev test involves intravital staining of gum glycogen - the content of this component increases significantly during periodontal inflammation. That is, intense staining of the gums indicates that it is inflamed. The test can also be used after completion of a course of treatment and to draw up a further course of action.
Advantages and disadvantages
An important component of implantation at all stages is an accurate index assessment of the condition of peri-implant tissues, implants and supported prostheses.
The Schiller-Pisarev test is quite effective and allows you to diagnose a wide range of conditions - gum inflammation, periodontal destruction, the amount of tartar, plaque, the need for certain therapeutic measures and their volume.
The relationship between the elements of the implant and adjacent tissues and its difference from a natural tooth may make complex periodontal studies impossible.
The Schiller-Pisarev test is quite accurate and objective and has two interpretation options. The first is visual, based on the nature of the gum staining, the second is numerical, that is, index. The problem with the methodology is that dental indices from 30-50 years ago do not meet the current needs of modern implantology.
That is, they can be used, but when interpreting the results, it will be necessary to take into account the full list of current changes and improvements in the field of prosthetics.
At the same time, it is the Schiller-Pisarev test that is considered the most informative of all similar diagnostic methods and allows the results to be most successfully adapted to the conditions of endosseous implantation.
However, the convention of numerical values still does not disappear anywhere, since diagnostics are carried out using markers, and not high-precision digital equipment. Modern researchers say that the Schiller-Miller test is still relevant, but should be used with certain modifications and clarifications.
How is the procedure performed?
The essence of the Schiller-Pisarev test is to lubricate the gums with a solution of iodine and potassium. As a result, areas with deep connective tissue lesions become stained - this is due to the accumulation of large volumes of glycogen in areas of inflammation.
The tests are repeated from time to time - if the treatment is carried out correctly, the condition of the gums will improve, and the inflammation will subside or disappear altogether.
That is, if the therapy is correct, then repeated tests should be weakly positive or negative.
Gum staining is due to the high amount of glycogen. When the inflammation passes, there is less glycogen, and the tissues cease to be intensely stained. In this way, the intensity and degree of development of the disease is determined.
Composition of the solution
To take Schiller-Pisarev samples, the composition of the solution is used in the following proportions:
- crystalline iodine – 1.0;
- potassium iodide – 2.0;
- distilled water – 40.0.
Before using therapeutic and prophylactic toothpaste (Parodontax, Parodontol paste), the gum mucosa is lubricated with a special solution, then the degree of staining is determined, and the data obtained is recorded in the disease history. Control – after 1, 2, 3, 6 and 12 months.
Result: index calculation, assessment of gum condition
For objectification purposes, the Schiller-Pisarev test is expressed in numbers (scores). The color of the papillae is rated at 2 points, the gingival margins at 4, and the gingival alveoli at 8 points. The total amount obtained is then divided by the number of teeth in the study area. That is, the calculation formula looks like this:
Iodine number = Sum of assessments for each tooth / Number of teeth examined.
The result is an iodine number in points. Evaluation of results by points:
- mild inflammation – up to 2.3 points;
- moderate inflammation – 2.67-5.0 points;
- severe inflammation – 5.33-8.0 points.
The peripheral circulation index (abbreviated as IPC) is also determined separately, taking into account the ratio of the time of resorption of hematomas that appeared under vacuum and the resistance of gingival capillaries. Test indicators are assessed in points, their ratio is expressed as a percentage. The index is calculated using the following formula:
- resistance of gum capillaries (scores);
- period of hematoma resorption (scores).
Based on index indicators, the functional state of the peripheral circulatory system is assessed. An IPC from 0.8 to 1.0 is considered normal, 0.6-0.7 is a good condition, 0.075-0.5 is a satisfactory condition, and from 0.01 to 0.074 is a decompensated state. You may be interested in learning how to strengthen teeth with periodontal disease.
The point system used to calculate the IPC (points are points)
| Resistance of gum capillaries | Period of resorption of vacuum hematomas |
| 1-10 seconds, 1 b. | 2.5 days, 10 b. |
| 11-20 seconds, 2 b. | 3 days, 20 b. |
| 21-30 seconds, 4 b. | 3.5 days, 40 b. |
| 31-40 seconds, 6 b. | 4 days, 60 b. |
| 41-50 seconds, 8 b. | 4.5 days, 80 b. |
| from 50 seconds, 10 b. | 5 days, 100 b. |
For more information about diagnosing and treating periodontal disease, watch the video
conclusions
- To diagnose periodontal diseases and evaluate the effectiveness of treatment, various methods are used, including periodontal indices.
- The essence of the Schiller-Pisarev technique is to stain the gums.
Areas deeply affected by the inflammatory process will become stained. Based on the intensity of staining, the stage of the pathology can be determined. It also allows you to distinguish periodontal disease from other similar pathologies. For more information on how periodontitis differs from periodontal disease, see this material. - The Schiller-Pisarev test involves two interpretation options - visual, based on the nature of gum staining, and numerical or index.
- To take Schiller-Pisarev samples, a solution of potassium iodide, crystalline iodine and distilled water is used.
- The main index indicators are the resistance of gum capillaries and the time of resorption of vacuum hematomas.
Periodontist: what he treats and what he does during the appointment
Characteristic signs and features of the course of acute gingivitis
Orthopantomography of the dentition: how it is done and why it is needed in dentistry
Chronic periodontitis: signs of periodontal disease and its treatment
Methods for clinical and epidemiological assessment of periodontal condition
RMA index. — Schiller-Pisarev test. — Gingival index GI. — Communal periodongal index CPI. — Complex periodongal index KPI. — Gum recession index. — Gingival attachment loss index. — Diagnosis of risk factors for the development of periodontal pathology and drawing up a plan of preventive measures.
When assessing the condition of the periodontium using visual and tactile methods, pay attention to the condition of the gums (color, size, shape, density, bleeding), the presence and location of the periodontal junction relative to the enamel-cementum border (i.e., the presence and depth of pockets), on tooth stability.
For more detailed studies of the condition of the periodontium, radiography is used (parallel technique, orthopantomogram, tomogram), electronic devices are less often used to determine the degree of tooth mobility, and diagnostic bacteriological tests are performed (see below). In periodontological practice, a special card is filled out, in which the degree of pathological changes in the area of each tooth is recorded during the initial examination of the patient, and the dynamics of the condition during treatment are noted.
To standardize and simplify registration records produced for clinical and epidemiological purposes, in our country and in the world it is common to use gingival and periodontal indices, which more or less fully describe the condition of the entire periodontium or its “sign” areas.
Schiller-Pisarev test
Designed to clarify the boundaries and degree of inflammation using vital tissue staining.
During inflammation, glycogen accumulates in the tissues, the excess of which can be detected by a qualitative reaction with iodine: a few seconds after the application of an iodine-containing preparation (most often this is Schiller-Pisarev solution), the tissues of the inflamed gums change their color in the range from light brown to dark brown. depending on the amount of glycogen, i.e. on the severity of inflammation.
The sample can be assessed as negative (straw-yellow color), weakly positive (light brown color) or positive (dark brown color).
This test cannot be used to diagnose periodontal pathology in children under 6 years of age, since their healthy gums contain a large amount of glycogen.
Gingival index GI (Loe, Silness, 1963)
The index involves assessing the condition of the periodontium based on clinical signs of gum inflammation - hyperemia, swelling and bleeding when touched with an atraumatic probe in the area of six teeth: 16, 21, 24, 36, 41, 44.
The condition of four areas of the gums near each tooth is studied: the medial and distal papilla on the vestibular side, the edge of the gums on the vestibular and lingual sides.
The condition of each section of the gum is assessed as follows: 0 - gums without signs of inflammation; 1 - slight discoloration, slight swelling, no bleeding during examination (mild inflammation); 2 - redness, swelling, bleeding during examination (moderate inflammation);
3 - severe hyperemia, edema, ulceration, tendency to spontaneous bleeding (severe inflammation).
GI for the periodontium of one tooth as an average value calculated from data on the condition of each section of the gum:
If we sum up all the GI values of the teeth and divide by the number of teeth examined, we obtain the GI value of the examined individual:
Interpretation: 0.1-1.0 - mild gingivitis; 1.1—2.0—moderate gingivitis;
2.1-3.0 - severe gingivitis.
Communal Periodontal Index CPI (1995)
The CPI (Community Periodontal Index) is intended to determine the condition of the periodontium in epidemiological studies. The situation is assessed based on the following criteria: the presence of subgingival stone, gum bleeding after gentle probing, and the presence and depth of pockets.
To determine the index, it is necessary to have special probes that unify and facilitate epidemiological surveys.
The probe for determining CPI has standard parameters: a relatively small mass (25 g) to reduce the aggressiveness of diagnostic probing, a scale for determining the depth of the subgingival space, and a button-shaped thickening at the tip, which serves both as protection against trauma to the epithelium of the dentogingival junction and as a scale element.
The probe scale is arranged as follows: the diameter of the “button” is 0.5 mm, at a distance from 3.5 mm to 5.5 mm there is a black mark, at a distance of 8.5 and 11.5 mm there are two rings (Fig. 6.12) .
To determine the periodontal condition of a tooth using the CPI index, perform the following steps.
1. The working part of the probe is placed parallel to the long axis of the tooth in one of four loci: in the distal and medial sections of the vestibular and oral surfaces.
2. The button of the probe with minimal pressure (up to 20 g) is inserted into the space between the tooth and soft tissues until an obstacle is felt, i.e. to the periodontal junction. Pressure restrictions are necessary to prevent destruction of the dentoepithelial junction.
Since objective measurements of pressure are impossible in this situation, it remains to train the researcher's proprioceptive control of muscle efforts.
To do this, the researcher must place a button probe on his nail and record in muscle memory a force sufficient to ischemia the nail bed, but painless.
Source: https://dobriydoc-krd.ru/semya/proba-shillera-v-stomatologii-funkczionalnye-proby
How is the procedure performed?
The essence of the Schiller-Pisarev test is to lubricate the gums with a solution of iodine and potassium. As a result, areas with deep connective tissue lesions become stained - this is due to the accumulation of large volumes of glycogen in areas of inflammation. The tests are repeated from time to time - if the treatment is carried out correctly, the condition of the gums will improve, and the inflammation will subside or disappear altogether. That is, if the therapy is correct, then repeated tests should be weakly positive or negative.
Gum staining is due to the high amount of glycogen. When the inflammation passes, there is less glycogen, and the tissues cease to be intensely stained. In this way, the intensity and degree of development of the disease is determined.
Composition of the solution
To take Schiller-Pisarev samples, the composition of the solution is used in the following proportions:
- crystalline iodine – 1.0;
- potassium iodide – 2.0;
- distilled water – 40.0.
Before using therapeutic and prophylactic toothpaste (, Parodontol), the gum mucosa is lubricated with a special solution, then the degree of staining is determined, the data obtained is recorded in the history of the disease. Control – after 1, 2, 3, 6 and 12 months.
Indications
In gynecology, colposcopy together with the Schiller test is considered mandatory in the case of preventive medical examinations.
In addition, this technique is prescribed in the following situations:
- spotting after sexual intercourse;
- together with a biopsy to study the condition of the genital organs;
- in case of presence of papillomavirus;
- when checking for malignant formations and precancerous conditions;
- in the presence of various inflammatory processes;
- as a control for various therapeutic procedures related to the cervix;
- before planning a pregnancy.
This test is also performed if itching, unusual discharge or chronic infectious diseases occur.
Thanks to the Schiller test, a gynecologist can detect many diseases of the cervix, which in the initial stages occur without pronounced symptoms.
The test performed so well that many do not even think about the fact that the results obtained may not always be accurate. But the procedure has disadvantages, this is explained by the following factors:
- the epithelium does not in all cases react with iodine present in Lugol's solution;
- after menopause, the upper female layers of the uterus become thinner and stop coloring;
- due to improperly placed speculum, there is a possibility of injury to the epithelial layers.
But these factors arise quite rarely, and when choosing a quality clinic, their likelihood is reduced to zero.
Interpretation:
Periodontium is a complex of tissues that have genetic and functional similarities: periodontium, alveolar bone, gums with periosteum and dental tissue (cement, enamel).
The depth of the periodontal sulcus is usually from 0.5 to 2.0 mm. Its base is located at the site of the intact junction of the epithelium with the tooth. Clinically, the gingival sulcus is a gap between healthy gums and the surface of the tooth; it is revealed by careful probing.
Periodontitis is an inflammation of periodontal tissues, characterized by progressive destruction of periodontal tissue and bone. The etiological factor is dental plaque. Local causes of artificial origin: - crown. Deeply advanced under the gum or incorrectly manufactured. Protruding edges of fillings.
Pathogenesis of local factors:
GL → gingivitis → formation of GL → formation of a pathological periodontal pocket → tooth mobility → tooth extraction.
If the dentogingival junction is disturbed, a pathological dentogingival pocket is formed, the depth upon probing is more than 3 mm.
Complex periodontal index KPI
(Leus P.I.) represents the average value of signs of periodontal damage from risk factors to the developed stage of the disease.
Formula KPI = Sum of characteristics (codes)
where: n is the number of sextants examined (one tooth from each sextant, usually 6).
Average KPI = Sum of individual KPI
Number of persons examined
Methodology: visually, using an angular probe, soft dental plaque, bleeding of the gingival sulcus, subgingival tartar, pathological periodontal pockets and pathological tooth mobility are determined and, if a sign is present, recorded in digital terms according to the following scheme:
| Signs | Criteria | Codes |
| Not defined | MN and signs of periodontal damage are not detected during examination using an angular probe | |
| Plaque | Any number of lesions determined by a probe on the surface of the tooth crown, in the interdental spaces or subgingival area | |
| Bleeding | Bleeding visible to the naked eye upon slight probing of the periodontal sulcus (pocket) | |
| Tartar | Any number of glands in the subgingival area | |
| Gingival or periodontal pocket identified by a probe more than 3 mm deep | ||
| Mobility | Pathological tooth mobility grade 2-3 (the tooth moves without effort by more than 1 mm) |
If there are signs, the existing higher code value is registered.
Depending on age, the following teeth are examined:
3 – 4 years 55, 51, 65,75,71,85.
7 – 14 years 16, 11, 26, 36, 31.46.
15 years and older 17/16, 11, 26/27, 37/36, 31, 46/47.
In this case, we examine 10 teeth from 6 sextants. Of two adjacent molars, we select the one with the larger code to calculate the index. We do not take into account the tooth with a lower code; as a result, we leave 6 teeth for calculating the index.
INTERPRETATION
Notes:
- If the first molar is missing, we examine only the second molar and vice versa.
If both 6 and 7 are missing, then 5→8→4.
If all the teeth in a sextant are missing, then this is most often a consequence of periodontitis (mobility) and this sextant is assessed with code 5 for calculating the index.
If there are crowns on the teeth, nearby teeth within the sextant are examined.
If all the teeth in the sextant have crowns, then examine the teeth with crowns.
To determine the CPITN index, the dentition is conventionally divided into 6 parts (sextants) including the following teeth:
In persons under 20 years of age, 6 teeth are examined: 16, 11, 26, 36, 31, 46; over 20 years old: 17/16, 11, 26/27, 37/36, 31, 46/47.
When examining each pair of each molar, only one code characterizing the worst condition is taken into account and recorded.
CPITN index codes and criteria :
Code 0 – healthy tissue
Code 1 – bleeding during probing
Code 2 – tartar
Code 3 – PZDK 4-5 mm
Code 4 – PZDK 6 mm or more
The examination is carried out using a periodontal button probe. Recommended areas for probing are: medial, median and distal areas, both on the vestibular, lingual and palatal surfaces.
To determine the need for periodontal disease treatment, patients may be categorized based on the following criteria:
0 – there is no need to treat this patient;
1 – improvement of oral hygiene is necessary;
2 - improving oral hygiene, professional hygiene;
3 - improving oral hygiene, professional hygiene, curettage;
4 - improving oral hygiene, professional hygiene, deep curettage, patch surgery, orthopedic treatment.
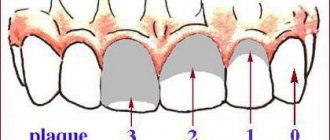
Soft dental plaque is clearly visible to the eye, is easily collected with a probe, and actively absorbs dyes. Soft plaque may not be immediately visible. Therefore, to identify it, preliminary staining with contrast dyes is necessary. The use of various dyes makes it possible to detect the presence of dental plaque and the places where they accumulate the most.
One of the criteria for assessing oral hygiene is an indicator that informs about the size of the surface of the tooth crown covered with plaque. Since dental deposits are usually colorless, they are determined using dyes (Bismarck brown, basic fuchsin red solution, Lugol’s solution, fluorescent sodium solution, etc.)
The use of various dyes makes it possible to detect the presence of dental plaque and the places where they accumulate the most. These substances can be used both for individual control by the patient himself and to determine the level of oral hygiene by a doctor.
Dyes for individual use
As a rule, they are either solutions for rinsing the mouth or coloring tablets for dissolving or chewing. Based on the intensity and location of the staining, a person himself can adjust his teeth cleaning technique. This is also helped by the use of individual dental mirrors with or without lighting.
Dyes for medical use are usually solutions that are applied directly to the surfaces of teeth using swabs or soaked beads.
Means for indicating dental plaque are used:
For the purpose of demonstrating plaque and hard deposits on teeth.
To assess the effectiveness of occupational hygiene.
To teach daily oral hygiene.
To identify plaque in hard-to-clean places. What to choose to identify plaque in a given situation depends on the doctor.
Indicators of dental plaque include a number of substances. Erythrosine tablets and solutions stain dental plaque red. Their disadvantage is the simultaneous staining of the oral mucosa. After treatment with sodium fluorescein, dental plaque acquires a yellow glow when irradiated with a special light source, without staining the gums. Combined solutions have been developed that make it possible to determine the age of dental plaque. So, when treated with such a solution, an immature (up to 3 days) dental plaque turns red, and a mature one (over 3 days) turns blue. Preparations based on iodine, fuchsin, and Bismarck brown can be used as coloring agents. Examples of coloring substances include Dent tablets (Japan), Espo-Plak (Paro), Red-Cote liquid and tablets (Butler), Plaque test (Vivadent) - an indicator liquid for visual detection of dental plaque under halogen light. Coloring agents can be supplied as impregnated beads for use on dental surfaces
Plaque indicators
In dental practice, 0.75% and 6% solutions of basic fuchsin, 4-5% alcohol solution of erythrosine, erythrosine in tablets (6-10 mg each), Schiller-Pisarev solution, 2% aqueous solution of methylene are used as diagnostic stains for dental plaque. blue.
Fuchsin (Fuchsini) is a basic solution of fuchsin. Colors dental plaque crimson. The drug is used for rinsing.
Rp.: Fuchsini bas. 1.5 Spiritus aethylici 75% 25 ml DS 15 drops per 1/2 glass of water (for rinsing the mouth for 20 s)
Erythrosin is a red dye of low toxicity. Contains iodine. Available in the form of a 4-5% alcohol solution and tablets (Mentadent C-Plague, Oga] In Einfarb Plagueindikator, Plague-Farbetabletten, etc.).
Rp.: Sol. Erythrosini 5% 15 ml DS Apply with a cotton swab to the surface of the teeth
Rp.: Tab. Erythrosini 0.006 N. 30 DS Chew 1 tablet for 1 minute
Fluorescein is a plaque dye that does not contain iodine, so it can be used in patients who are sensitized to iodine. Fluorescein-stained plaque is visible only under ultraviolet light. Available under the names “Plak-Lite” (“Blendax”), “Fluorescein” 0.75%.
Schiller-Pisarev solution stains dental plaque yellow-brown. The drug is applied to the surface of the teeth using a cotton swab.
Rp.: lodi 1.0 Kalii iodidi 2.0 Aq. destill. 40 ml MDS Schiller-Pisarev solution. Apply with a cotton swab to the surface of the teeth
Methylene blue (Methylenum coeruleum) is used to identify dental plaque: a 1-2% aqueous solution of methylene blue is applied to the surface of the teeth using a cotton swab.
Rp.: Methyleni coerulei 2.0 Aq. dcstiil. 100 ml MDS To lubricate the surface of teeth
Lugol's solution: Composition: KI - 2.0 g I crystalline - 1.0 g distilled water - 17 ml Method and mechanism are the same as in the previous dye
Disclosing Solution (60ml) —
Directions for use: Prepare a solution: 10 drops of indicator per 30 ml of water. Rinse your mouth. Do not swallow! Colored areas indicate the presence of bacterial plaque. Carry out additional cleaning of problem areas.
Katerol -
Plaque indicator, liquid for removing plaque and cleaning teeth.
KATEROL is an indicator of dental plaque (dental plaque), a drug for removing dental plaque and cleaning teeth.
Ingredients: hydrochloric acid, iodine, acetone, excipients. Properties: Caterol softens calculus deposits and destroys supragingival plaque, facilitating subsequent mechanical removal using instruments.
Caterol also helps detect plaque and tartar by turning it yellow.
Contraindications: allergy to iodine or its derivatives.
Instructions for use.
Using a thick cotton ball soaked in Caterol and wrung out well, thoroughly rub the tartar deposits, trying to avoid contact with the gum as much as possible.
Wait a few seconds for the stone to soften before mechanical.
Curaprox tablets -
It colors old plaque blue and new plaque red. Ideal for home use. Each tablet is individually packaged.
Liquid Curadent
Curadent for plaque detection is a two-color liquid that detects plaque. Old plaque turns blue, and fresh plaque turns red. (60 ml - 1,615 rubles).
Plaque Agent (
Docdont) - mouth rinse to detect plaque (500 ml - 400 rubles)
The mouthwash is suitable for both adults and children.
The mouthwash does not contain erythrosine, so it is successfully used by both adults and children. This method of identifying plaque is especially suitable for children, since they cannot always assess whether they have carried out the process of cleaning their teeth correctly. And if you rinse your mouth with this solution before doing this, you can monitor the quality of cleaning.
Recommendations: Use by children under 12 years of age should be under adult supervision. Pour 10 ml of mouthwash into a measuring cup, rinse your mouth for 30 seconds, and spit it out. Clean blue areas thoroughly with a toothbrush and toothpaste.
Plaquetest tablets for detecting dental plaque
Plaquetest tablets for detecting dental plaque. Old dental plaque is painted dark blue, new plaque is purple-red.
To carry out the test:
Place the tablet on your tongue (half is enough for children), chew it and spread it over the entire dentition with your tongue. Spit it out - it's done! The paint is easily removed with regular tooth brushing.
Ingredients: lactose, magnesium stearate, silicon dioxide, meadow mint, CI 42090 (food coloring), CI 45410 (food coloring).