Acute periodontitis
Acute periodontitis is an acute inflammation of the periodontium.
Etiology. Acute purulent periodontitis develops under the influence of mixed flora, where streptococci predominate (mainly non-hemolytic, as well as viridian and hemolytic), sometimes staphylococci and pneumococci. Possible rod-shaped forms (gram-positive and gram-negative), anaerobic infection, which is represented by obligate anaerobic infection, non-fermenting gram-negative bacteria, veillonella, lactobacilli, yeast-like fungi. In untreated forms of apical periodontitis, microbial associations number 3-7 types. Pure cultures are extremely rarely isolated. With marginal periodontitis, in addition to the listed microbes, there is a large number of spirochetes, actinomycetes, including pigment-forming ones. Pathogenesis. An acute inflammatory process in the periodontium primarily occurs as a result of the penetration of infection through an opening in the apex of the tooth, or less often through a pathological periodontal pocket. Damage to the apical part of the periodontium is possible due to inflammatory changes in the pulp, its necrosis, when the abundant microflora of the tooth canal spreads into the periodontium through the apical opening of the root. Sometimes the putrefactive contents of the root canal are pushed into the periodontium during chewing, under the pressure of food.
Marginal, or marginal, periodontitis develops as a result of the penetration of infection through the gum pocket due to injury or the contact of medicinal substances, including arsenic paste, on the gum. Microbes that have penetrated into the periodontal gap multiply, form endotoxins and cause inflammation in periodontal tissues. Some local features are of great importance in the development of the primary acute process in the periodontium: lack of outflow from the pulp chamber and canal (presence of an unopened pulp chamber, filling), microtrauma during active chewing load on a tooth with an affected pulp. General reasons also play a role: hypothermia, past infections, etc., but most often the primary impact of microbes and their toxins is compensated by various nonspecific and specific reactions of periodontal tissues and the body as a whole. Then an acute infectious-inflammatory process does not occur. Repeated, sometimes prolonged exposure to microbes and their toxins leads to sensitization, and antibody-dependent and cellular reactions develop. Antibody-dependent reactions develop as a result of immune complex and IgE-mediated processes. Cellular reactions reflect a delayed-type allergic hypersensitivity reaction. The mechanism of immune reactions, on the one hand, is due to a violation of phagocytosis, the complement system and an increase in polymorphonuclear leukocytes; on the other hand, by the proliferation of lymphocytes and the release of lymphokines from them, causing destruction of periodontal tissue and resorption of nearby bone. Various cellular reactions develop in the periodontium: chronic fibrous, granulating or granulomatous periodontitis. Violation of protective reactions and repeated exposure to microbes can cause the development of an acute inflammatory process in the periodontium, which in essence is an exacerbation of chronic periodontitis. Clinically, they are often the first symptoms of inflammation. The development of pronounced vascular reactions in a fairly closed periodontal space, an adequate protective response of the body, as a rule, contributes to inflammation with a normergic inflammatory reaction.
The compensatory nature of the response of periodontal tissues during a primary acute process and exacerbation of a chronic one is limited by the development of an abscess in the periodontium. It can be emptied through the root canal, gum pocket when opening a periapical lesion or removing a tooth. In some cases, under certain general and local pathogenetic conditions, a purulent focus is the cause of complications of odontogenic infection, when purulent diseases develop in the periosteum, bone, and perimaxillary soft tissues.
Pathological anatomy. During an acute process, the main phenomena of inflammation appear in the periodontium - alteration, exudation and proliferation. Acute periodontitis is characterized by the development of two phases - intoxication and a pronounced exudative process. During the intoxication phase, various cells migrate—macrophages, mononuclear cells, granulocytes, etc.—to the area where microbes accumulate. In the phase of the exudative process, inflammatory phenomena increase, microabscesses form, periodontal tissue melts and a limited abscess is formed. On microscopic examination, in the initial stage of acute periodontitis, one can see hyperemia, swelling and a small leukocyte infiltration of the periodontal area around the root apex. During this period, perivascular lymphohistiocytic infiltrates containing single polynuclear cells are detected. As the inflammatory phenomena further increase, leukocyte infiltration intensifies, capturing larger areas of the periodontium. Separate purulent lesions form - microabscesses, and periodontal tissue melts. Microabscesses connect with each other, forming an abscess. When a tooth is removed, only individual remaining areas of sharply hyperemic periodontium are revealed, and throughout the rest of the root the root is exposed and covered with pus.
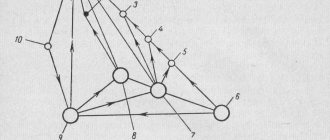
An acute purulent process in the periodontium causes changes in the tissues surrounding it (bone tissue of the alveolar walls, periosteum of the alveolar process, peri-maxillary soft tissues, tissues of regional lymph nodes). First of all, the bone tissue of the alveoli changes. In the bone marrow spaces adjacent to the periodontium and located over a considerable extent, bone marrow edema and varying degrees of pronounced, sometimes diffuse, infiltration of neutrophilic leukocytes are noted. In the area of the cortical plate of the alveoli, lacunae filled with osteoclasts appear, with a predominance of resorption (Fig. 7.1, a). Restructuring of bone tissue is observed in the walls of the socket and mainly in the area of its bottom. The predominant resorption of bone leads to the expansion of the holes in the walls of the socket and the opening of the bone marrow cavities towards the periodontium. There is no necrosis of the bone beams (Fig. 7.1, b). Thus, the restriction of the periodontium from the alveolar bone is broken. In the periosteum covering the alveolar process, and sometimes the body of the jaw, in the adjacent soft tissues - gums, peri-maxillary tissues - signs of reactive inflammation are recorded in the form of hyperemia, edema, and inflammatory changes are also observed in the lymph node or 2-3 nodes, respectively, of the affected periodontal tissue of the tooth. . Inflammatory infiltration is observed in them. In acute periodontitis, the focus of inflammation in the form of abscess formation is mainly localized in the periodontal fissure. Inflammatory changes in the alveolar bone and other tissues are reactive, perifocal in nature. And it is impossible to interpret reactive inflammatory changes, especially in the bone adjacent to the affected periodontium, as its true inflammation.
Clinical picture . In acute periodontitis, the patient indicates pain in the causative tooth, which intensifies when pressing on it, chewing, and also when tapping (percussion) on the chewing or cutting surface. The feeling of “growing” or lengthening of the tooth is characteristic. With prolonged pressure on the tooth, the pain subsides somewhat. Subsequently, the pain intensifies, becoming continuous or with short light intervals. They are often pulsating. Thermal effects, the patient taking a horizontal position, touching the tooth, and biting increase the pain. The pain spreads along the branches of the trigeminal nerve. The general condition of the patient is satisfactory. On external examination, as a rule, there are no changes. Enlargement and tenderness of the lymph node or nodes associated with the affected tooth are observed. Some patients may have mildly expressed collateral edema of the perimaxillary soft tissues adjacent to this tooth. Percussion is painful in both vertical and horizontal directions. The mucous membrane of the gums, alveolar process, and sometimes the transitional fold in the projection of the tooth root is hyperemic and swollen. Palpation of the alveolar process along the root, especially corresponding to the opening of the apex of the tooth, is painful. Sometimes, when pressing with an instrument on the soft tissues of the vestibule of the mouth along the root and transitional fold, an impression remains, indicating their swelling.
Diagnosis is based on the characteristic clinical picture and examination data. Temperature stimuli and electrical odongometry data indicate a lack of pulp response due to its necrosis. On an x-ray during an acute process of pathological changes in the periodontium, it is possible not to detect or to detect an expansion of the periodontal fissure, blurred cortical plasticity of the alveoli. With an exacerbation of the chronic process, changes characteristic of granulating, granulomatous, and rarely fibrous periodontitis occur. As a rule, there are no changes in the blood, but in some patients leukocytosis (up to 9-109/l), moderate neutrophilia due to band and segmented leukocytes are possible; ESR is often within normal limits.
Differential diagnosis . Acute periodontitis is differentiated from acute pulpitis, periostitis, osteomyelitis of the jaw, suppuration of the root cyst, acute odontogenic sinusitis. Unlike pulpitis, in acute periodontitis the pain is constant, and in diffuse inflammation of the pulp it is paroxysmal. In acute periodontitis, in contrast to acute pulpitis, inflammatory changes are observed in the gum adjacent to the tooth; percussion is more painful. In addition, electrical odontometry data helps in diagnosis. Differential diagnosis of acute periodontitis and acute purulent periostitis of the jaw is based on more pronounced complaints, feverish reaction, the presence of collateral inflammatory edema of the peri-maxillary soft tissues and diffuse infiltration along the transitional fold of the jaw with the formation of a subperiosteal abscess. Percussion of the tooth during periostitis of the jaw is less painful, unlike acute periodontitis. Based on the same, more pronounced general and local symptoms, differential diagnosis of acute periodontitis and acute osteomyelitis of the jaw is carried out. Acute osteomyelitis of the jaw is characterized by inflammatory changes in the adjacent soft tissues on both sides of the alveolar process and the body of the jaw. In acute periodontitis, percussion is sharply painful in the area of one tooth, in osteomyelitis - in several teeth. Moreover, the tooth that was the source of the disease reacts to percussion less than neighboring intact teeth. Laboratory data - leukocytosis, ESR, etc. - allow us to distinguish between these diseases.
Purulent periodontitis should be differentiated from suppuration of a perihilar cyst. The presence of limited bulging of the alveolar process, sometimes the absence of bone tissue in the center, and displacement of teeth, in contrast to acute periodontitis, characterize a suppurating perihilar cyst. An x-ray of a cyst reveals a round or oval area of bone resorption.
Acute purulent periodontitis must be differentiated from acute odontogenic inflammation of the maxillary sinus, in which pain can develop in one or more adjacent teeth. However, congestion of the corresponding half of the nose, purulent discharge from the nasal passage, headache, and general malaise are characteristic of acute inflammation of the maxillary sinus. Violation of the transparency of the maxillary sinus, revealed on an x-ray, allows you to clarify the diagnosis.
Treatment. Therapy of acute apical periodontitis or exacerbation of chronic periodontitis is aimed at stopping the inflammatory process in the periodontium and preventing the spread of purulent exudate into the surrounding tissues - the periosteum, perimaxillary soft tissues, bone. Treatment is predominantly conservative and is carried out according to the rules set out in the corresponding section of the textbook “Therapeutic Dentistry” (2002). Conservative treatment is more effective with infiltration or conduction anesthesia with 1-2% solutions of lidocaine, trimecaine, ultracaine.
A more rapid subsidence of inflammatory phenomena is facilitated by a blockade - the introduction of an infiltration anesthesia type of 5-10 ml of a 0.25-0.5% solution of an anesthetic (lidocaine, trimecaine, ultracaine) with lincomycin into the area of the vestibule of the mouth along the alveolar process, respectively, to the affected one and 2-3 neighboring teeth. The anti-edematous effect is provided by the introduction of the homeopathic remedy “Traumel” in the amount of 2 ml along the transitional fold or external dressings with ointment of this drug.
It must be borne in mind that without the outflow of exudate from the periodontium (through the tooth canal), blockades are ineffective and often ineffective. The latter can be combined with an incision along the transitional fold to the bone, with perforation of the anterior wall of the bone using a bur, corresponding to the peri-apical part of the root. This is also indicated in case of unsuccessful conservative therapy and an increase in inflammatory phenomena, when it is not possible to remove the tooth due to some circumstances. If treatment measures are ineffective and inflammation increases, the tooth should be removed. Tooth extraction is indicated when there is significant destruction, obstruction of the canal or canals, or the presence of foreign bodies in the canal. As a rule, tooth extraction leads to rapid subsidence and subsequent disappearance of inflammatory phenomena. This can be combined with an incision along the transitional fold to the bone in the area of the root of the tooth affected by acute periodontitis. After tooth extraction during a primary acute process, curettage of the hole is not recommended, but should only be washed with a solution of dioxidine, chlorhexedine and its derivatives, gramicidin. After tooth extraction, pain may intensify and body temperature may rise, which is often due to the traumatic nature of the intervention. However, after 1-2 days, these phenomena, especially with appropriate anti-inflammatory drug therapy, disappear.
To prevent complications after tooth extraction, you can inject anti-staphylococcal plasma into the dental alveolus, wash it with streptococcal or staphylococcal bacteriophage, enzymes, chlorhexidine, gramicidin, leave an iodoform swab and a sponge with gentamicin in the mouth. General treatment of acute or exacerbation of chronic periodontitis consists of prescribing oral pyrazolone drugs - analgin, amidopyrine (0.25-0.5 g each), phenacetin (0.25-0.5 g each), acetylsalicylic acid (0.25-0.5 g each). 0.5 g). These drugs have analgesic, anti-inflammatory and desensitizing properties. Some patients are prescribed sulfonamide drugs according to indications (streptocide, sulfadimezin - 0.5-1 g every 4 hours or sulfadimethoxine, sulfapyridazine - 1-2 g per day). However, the microflora, as a rule, is resistant to sulfonamide drugs. In this regard, it is more advisable to prescribe 2-3 pyrosolone drugs (acetylsalicylic acid, analgin, amidopyrine) 1/4 tablets of each, 3 times a day. This combination of drugs gives an anti-inflammatory, desensitizing and analgesic effect. Weakened patients burdened with other diseases, especially the cardiovascular system, connective tissue, and kidney diseases are treated with antibiotics - erythromycin, kanamycin, oletethrin (250,000 units 4-6 times a day), lincomycin, indomethacin, voltaren (0. 25 g) 3-4 times a day. Foreign specialists, after tooth extraction due to an acute process, necessarily recommend treatment with antibiotics, considering such therapy also as a prevention of endocarditis and myocarditis. After tooth extraction in acute periodontitis, in order to stop the development of inflammatory phenomena, it is advisable to use cold (an ice pack on the soft tissue area corresponding to the tooth for 1-2-3 hours). Next, warm rinses, Sollux are prescribed, and when the inflammatory phenomena subside, other physical methods of treatment are prescribed: UHF, fluctuarization, electrophoresis of diphenhydramine, calcium chloride, proteolytic enzymes, exposure to helium-neon and infrared lasers.
Exodus. With proper and timely conservative treatment, in most cases of acute and exacerbation of chronic periodontitis, recovery occurs. (Insufficient treatment of acute periodontitis leads to the development of a chronic process in the periodontium.) It is possible for the inflammatory process to spread from the periodontium to the periosteum, bone tissue, peri-maxillary soft tissues, i.e. Acute periostitis, osteomyelitis of the jaw, abscess, phlegmon, lymphadenitis, inflammation of the maxillary sinus may develop.
Prevention is based on sanitation of the oral cavity, timely and correct treatment of pathological odontogenic lesions, functional unloading of teeth using orthopedic treatment methods, as well as on carrying out hygienic and health measures.
Did you like the article? Share with friends
0
Similar articles
Next articles
- Treatment of chronic periodontitis
- Acute purulent periostitis of the jaw
- Chronic periostitis of the jaw
- Assessment of the thickness of tissue removed during tooth preparation using the temporary crown method
- Separation and protection of adjacent teeth during preparation
Previous articles
- Classification of periodontitis
- Local complications arising after tooth extraction
- Local complications arising during tooth extraction
- Minimally invasive therapy with the Vector system and its role in the complex treatment of periodontal diseases
- Creating surface shine for composite restorations
Add a comment
Laboratory and instrumental methods for diagnosing dental diseases
Additional diagnostics:
- thermodiagnostics;
- electroodontodiagnostics (EDD);
- X-ray methods;
- laboratory research.
Thermodiagnostics
Thermal diagnostics is a method for determining the sensitivity of the pulp to temperature stimuli. It is carried out by exposing the carious cavity to cold or heated gutta-percha water heated to 60–70 degrees.
Thus, differential diagnosis : the reaction associated with the pain that the tooth exhibits indicates a particular disease. Rapidly passing pain is typical for a diagnosis such as caries without complications. Prolonged pain is a sign of pulpitis, while the absence of painful manifestations may indicate the death of the pulp and the development of periodontitis.
Electroodontodiagnosis
EDI – determination of the sensitivity of the nerve endings of the pulp to the effects of direct electric current. This method effectively carries out differential diagnosis of dental caries, identifies diseases of the pulp (pulpitis and its forms), and periodontal disease.
Healthy teeth respond to currents of up to 6 µA; with the development of deep caries, the reaction occurs only with a current strength of 15 - 20 µA, i.e. Sensitivity in a diseased tooth decreases, and with pulpitis - over 20 µA. A reaction to a current of about 60 µA indicates the death of the pulp in the coronal part of the tooth (for example, as a complication of pulpitis), and a current of 100 µA indicates damage to the periodontium and periodontal tissues.
X-ray diagnostic methods
X-ray methods of differential diagnosis are divided into:
- intraoral radiography – used to assess the condition of crowns and root canals, dental and periodontal tissues;
- extraoral (includes orthopantomography, radiography with contrast, tomography) - allows you to determine traumatic injuries, identify tumor formations, the condition of periodontal tissues, jaw joints;
- radiovisiography (in its modern version - digital radiography) - makes it possible to study dental tissue in a targeted manner with minimal radiation exposure to the patient.
Sometimes a luminescence test is used, based on changes in tissue color when exposed to ultraviolet radiation, and the application of markers to the surface of the tooth to detect caries at the stain stage.
Laboratory diagnostic methods include:
- blood and urine tests, gastric juice, oral fluid;
- bacteriological;
- cytological;
- histological examination.
Also, instrumental modern methods for diagnosing dental caries and other dental pathologies use various equipment:
- in endodontics, an electronic device is often used that determines how long the canal in the root of a tooth is - an apexlacator;
- to facilitate visual inspection, they use a dental camera, which displays the tooth and oral cavity in an enlarged view on the screen;
- For even greater magnification (25 times or more), which is especially important for endodontic treatment and diagnosis of subtle pathological processes, a dental microscope is used.
The diagnosis is made more accurately and quickly.
Treatment
At the initial stage of treatment, it is important to repair the damage caused by the injury. It may be necessary to correct the crowns, remove excess parts of the filling, particles of the injured tooth, etc.
After this, they move on to symptomatic treatment. Anti-inflammatory and painkillers are prescribed, as well as physical therapy. When a tooth is displaced, the pulp is checked for vitality and the integrity of the tooth root is ensured using an x-ray examination. Three weeks after treatment, the image must be repeated.
An important task in the treatment of this disease is to stop the outbreak in order to prevent the spread of infection to other parts of the oral cavity.
Note: In addition, it is very important to eliminate the factors that cause inflammation - adjust the crown, polish the filling material, apply orthopedic methods to correct the bite, etc.
It is important to use anesthesia due to severe pain, due to the following reasons:
- The presence of pain from an impact and pain from injury regarding dental problems when a filling or crown is placed incorrectly.
- The presence of pain from the inflammatory process in the periodontium.
In addition to the effects of painkillers, the patient is also prescribed physical therapy.
When a tooth is displaced as a result of injury, endodontic treatment is carried out and the dental organ is strengthened with orthopedic products.
Antibiotics for traumatic periodontitis are usually not used, except as local applications. In this case, inflammation is stopped with the help of antiseptics.
For the inflammatory process in such a disease, the primary goal is to relieve pain, swelling and provide rest to the damaged dental unit.
Then the tooth is treated regarding the situation and the presence of complications.
The result can be predicted based on the following factors:
- how strong the blow was and how badly the tooth was injured;
- the injury is one-time or is the result of permanent injury;
- how quickly after the injury the patient sought specialist help;
- the presence or absence of concomitant diseases - periodontal disease, caries, gingivitis, pulpitis.
If there has been a rupture of the neurovascular bundle, the pulp is removed from the tooth, and then the canals are cleaned and filled.
If a fracture of a dental organ occurs, it is either filled (if only the outer part is fractured, when the nerve is not affected), or the nerve is removed and a stump tab is placed in the tooth, and a crown is placed on it (if the nerve was damaged), or the tooth is removed completely (if the root is has a splintered or longitudinal fracture).
If a tooth has dislocated and left its socket, it can be replanted. The nerve is removed from the tooth, it is filled, and then returned to its original place. To do this, it is important to clear the hole of blood clots, install the tooth in it, and then carefully splint it.