Causes of apical periodontitis
Whether it is primary apical periodontitis or periodontitis after treatment, it is important to thoroughly understand the development features and causes of apical periodontitis.
Development is influenced by many reasons, including:
- Bacterial infection
- Trauma (traumatic periodontitis)
- Iatrogenic factor
- Chemical agents (medicated periodontitis)
- Idiopathic factor
Bacterial infection
Bacterial infection occupies a leading place among all factors that can cause periodontitis.
Developing their vital activity on the surfaces of the buccal mucosa, tonsil crypts, dorsal surface of the tongue, and tooth surfaces, microbes can migrate and cause inflammation of various structures, including the apical periodontium. The routes of penetration into the apical periodontium are considered to be the root canal of the tooth, along with it the lateral tubules, or the gingival sulcus through damaged root cement.
Many clinical authors consider pulp necrosis to be the main unfavorable situation in the development of periodontitis. The process involves anaerobic flora (veillonella, fusobacteria, actinomycetes, bacteroides), this flora causes destructive changes in the tissues of the apical periodontium.
Endotoxins, formed due to damage to the wall of gram-negative microorganisms, play an important role. They are taken up by antigen presenting cells (APCs), which activate T lymphocytes. The produced cytokines activate IL-1, IL-4, IL-5, IL-6, which are necessary to “turn on” granulocytes and IL-8. At the same time, bacterial endotoxin (LPS), derived from gram-negative bacteria, is involved in the activation of macrophages.
All this is aimed at the specific phagocytosis of microbes from the root canal. A side effect is bone resorption through the RANKL system, induced by tumor necrosis factor and IL-1B produced by macrophages.
An acute or chronic traumatic factor causes pulp ischemia and subsequent necrosis. While necrotic masses have a cytotoxic effect, apical periodontitis develops. Acute is understood as a strong short-term impact on the periodontium of the tooth, for example, a blow, perforation of the wall, as well as due to surgical manipulations (removal of a tumor, formations, cysts). Due to acute trauma, hemorrhage occurs in the periodontium, and acute phenomena occur.
Chronic trauma is long-term and occurs during orthodontic treatment or occlusal trauma. Accompanied by destructive changes at the tops of the roots.
Iatrogenic triggers can be the absence or incorrect diagnosis, errors at the stages of treatment of caries or pulpitis, overestimation of fillings or orthopedic structures, non-compliance with the exposure time of devitalizing agents, removal of aggressive liquids and filling materials beyond the apex of the tooth root, allergies to medications.
Among idiopathic periodontitis, there is an influence of petrificates and denticles, somatic pathology, and age.
Description of the periodontium and its functions
Periodontium is a tissue that provides fixation of tooth roots in the sockets of the jaw bones.
It connects the teeth to the bone base of the lower jaw and the mucous membrane of the oral cavity. Periodontal development begins with the eruption of teeth and ends when they fall out. Periodontal tissues ensure the integrity of teeth and effectively protect the anatomical structures they cover from the effects of various damaging factors.
The periodontal structure includes:
- Jaw.
- Periodontal ligament.
- Gum.
- Gingival groove.
- Cement (covers the root of the tooth).
- Dentine.
- Pulp.
- Enamel (covers the crown of the tooth).
The main components of the periodontium are the gums, periodontal ligaments, dental cementum and alveolar bone. Alveolar bone is a differentiated structure of the mandibular bone. It is responsible for fixing the roots of teeth in the dental alveoli.
The periodontal ligament consists of collagen fibers that connect the root surface of the teeth (cementum) to the alveolar bone. Like a hydraulic shock absorber, the periodontal ligament absorbs the pressure exerted on the alveolar bone when it catches food and tears it apart. These specialized fibers improve the pressure resistance of the underlying bone tissue and produce painful stimulation when their resistance reaches an upper limit.
Cement covers the roots of the teeth. It has the same structure as bone tissue, but it lacks lacunae and canals. The gums cover the underlying alveolar bone and fit tightly to the base of the crown of the teeth. They consist of squamous keratinized epithelium, which is distinct from the supernumerary, vascularized, and nonkeratinized mucosa. Each gum is formed by two parts:
- the free part, which is located at the level of the tooth crown. It protects the space (gum sulcus) surrounding the crown of the tooth. Normally, the depth of the gingival grooves in cats does not exceed 0.5 mm. It is the gingival groove that is the most vulnerable point of connection between the gums and the tooth. This closed space is surrounded by tissue on all sides, which contributes to the accumulation of dental plaque and various food debris in it. Due to its histological structure, the tissues that form the gingival sulcus are highly susceptible to inflammatory processes, which serves as a trigger for the development of periodontal diseases. Therefore, special attention should be focused on the treatment of periodontal diseases and their prevention;
- the part of the gum adjacent to the tooth and alveolar bone is the most important barrier to the spread of bacteria. The junction of the gums protrudes above the base of the tooth crown and enhances this protective function.
The oral cavity of cats is never sterile. This is evidenced by the fact that every day a large number (up to 100 million) of bacteria are released from it with saliva. Therefore, in animals it is always possible to detect foci of inflammation of varying severity in the oral mucosa. Thus, the concept of “normal” periodontium is very relative, and it is used exclusively for clinical purposes. The criterion for assessing the condition of periodontal tissue in cats is the absence of visible signs of inflammation and maintaining the depth of the gingival grooves at a level of less than 0.5 mm.
Plaque forms on the entire surface of the teeth as a result of their contact with saliva. Due to the peculiarities of the anatomical structure of the tissues that are most predisposed to the formation of dental plaque, it is found only on the crowns of teeth, at the junction of the gums and at the point of contact of adjacent teeth.
Acute apical periodontitis
Acute apical periodontitis is usually a consequence of irreversible pulpitis or a complication of endodontic treatment. When inflammation passes from the pulp to the apical periodontium, the patient complains of constant aching pain in a certain tooth with an intensity ranging from moderate to severe. The facial configuration of such a patient is not changed, the lymph nodes may be slightly painful and enlarged. Intraorally, we do not observe any changes in the mucous membrane in the projection of the causative tooth. The tooth itself may be intact, under a permanent filling, or destroyed. Percussion is slightly painful.
The intoxication phase ends as lactic acid accumulates, acidosis develops in the tissues, and the permeability of the vascular wall increases and the release of leukocytes. The exudative phase begins (Acute serous periodontitis according to I. G. Lukomsky)
The patient is bothered by continuous pain; it hurts to touch the tooth. The tooth feels higher than the others (symptom of an “overgrown” tooth). The general condition does not suffer, the lymph nodes are painful and mobile.
In the oral cavity we see a tooth under a filling or with a carious cavity, but it may be intact, percussion is painful, probing is painless. The mucous membrane in the projection of the apex is swollen and hyperemic.
Remember that the serous stage very quickly turns into a purulent stage.
Acute purulent periodontitis according to I. G. Lukomsky
Acute purulent periodontitis is distinguished by a vivid clinical picture, caused by throbbing pain radiating along the branches of the trigeminal nerve. It is very painful for the patient to touch the tooth, so he keeps his mouth half open. The general condition is poor, the lymph nodes are painful and mobile.
In the mouth we see a destroyed, under a filling or intact mobile causative tooth, probing is painless, percussion is sharply painful, the mucous membrane is swollen, hyperemic, painful on palpation.
Purulent exudate can drain through the root canal, periodontal pocket or under the periosteum. After pus penetrates under the periosteum, the patient's condition improves briefly, but periostitis develops.
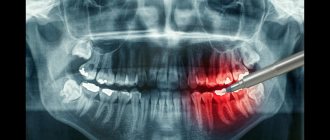
Diagnosis of apical periodontitis
Diagnosis of apical periodontitis is not particularly difficult. It is based on the use of basic and additional methods.
The main ones include clarifying the patient’s complaints, medical history, probing, percussion, palpation and determining tooth mobility.
Additional special methods include determining the electrical excitability of the pulp (reduced to 200 μA), x-ray examination, determining occlusion, fistula tract, and temperature tests.
On an x-ray, the causative tooth may have an extensive filling, a cavity, or previously direct pulp coverage.
There may not be any radiological changes in the area of the root apex; sometimes a slight expansion of the periodontal fissure is observed. Possible clearing may be due to a combination of signs of irreversible pulpitis and acute apical periodontitis.
If there is pus near the apex, the severity of the changes depends on the degree of bone destruction and on the outflow of pus through fenestrations in the cortical plate.
As already mentioned, infection of the apical periodontium can occur not only through the root canal, but also through the periodontal pocket through the gingival sulcus. This condition is called acute periodontal abscess.
The onset is acute, spontaneous pain occurs, the tooth is painful when pressed, and swelling appears due to the presence of pus. A distinctive feature of this pathology is the vital pulp.
In the differential diagnosis of acute purulent periodontitis and periodontal abscess, the main difference is the condition of the pulp. In acute periodontal abscess, the pulp is vital, since the problems begin with the marginal periodontium. The causes of acute periodontal abscess include dental plaque, occlusal trauma, decreased immunity and concomitant pathology. While the cause of acute purulent periodontitis is mostly pulp necrosis.
Symptoms
A yellowish coating and hard deposits are not the only signs of pathology. It can also be identified by the following symptoms:
- The appearance of an unpleasant, putrid odor from the mouth.
- Poor appetite. The animal prefers soft food and refuses hard food.
- Increased salivation, admixtures of blood and pus in the saliva, wet fur in the chin area.
- Changes in the animal's behavior: slurping while chewing, trembling of the lower jaw, constant rubbing of the muzzle with a paw.
- Bleeding, redness of the gums, the presence of massive dark-colored hard deposits on the teeth.
If you press on the gum of a sick animal, gray pus comes out from under it. The teeth may become loose, but due to the long roots they do not fall out for a long time.
Treatment of acute apical periodontitis
Treatment of acute apical periodontitis, if necessary, begins with emergency care. It involves draining purulent contents from the root canal. There is still debate about whether to leave the tooth exposed or not. The positive effect of the “open tooth” has not been scientifically proven. If, after opening the tooth, pus is released from the canal, then we stop the exudation after a few minutes. If it is not possible to stop it, then we warn the patient about the need for drainage. Everything is done under the conditions of applying a rubber dam.
At the same time, antibiotics, anti-inflammatory, and antihistamines are prescribed.
Between visits, it is strongly recommended to close the tooth cavity with a cotton ball to prevent food from getting into the canals. If the period of exacerbation has passed, the tooth should be closed the next day after high-quality mechanical and medicinal treatment of the root canal system.
It has been studied and proven that open teeth secrete more secretory immunoglobulin A compared to closed teeth. It activates epithelial growth factor, which begins the proliferation of the epithelium of the Malasse islets. A cyst forms.
In general, treatment is based on classical endodontics. Temporary root canal filling is allowed between visits for a period of 1 week to six months. Calcium hydroxide has an antiseptic, antibacterial, prolonged therapeutic effect due to its high pH. On the other hand, it can cause obliteration of canals, root resorption, and reduces the elasticity of dentin, increasing the risk of fracture. If there are no complaints or changes at the apex, the canals are filled with permanent materials.
The article was written by O. Vishnyak specifically for the OHI-S.COM website. Please, when copying material, do not forget to provide a link to the current page.