October 28, 2020 Last revised: December 14, 2020 Gum disease
Every person has experienced gum disease at least once. And these ailments cannot be considered trivial, as some patients think frivolously. Most gingivitis (gum inflammation) requires a serious approach and timely treatment. In advanced cases, such ailments can lead to loosening of teeth and their loss. One of the most dangerous types is ulcerative gingivitis (or ulcerative-necrotic). We suggest you read more about the main signs, symptoms and treatment of such gingivitis in this publication.
Etiology
Pathogens
The cause of the development of necrotizing ulcerative gingivitis is a bacterial infection in the pathogenic microflora. The causative agents are anaerobic bacteria, spirochetes and fusobacteria.
“Flocks” of such pests live in the mouth of every healthy person, but their number is negligible and they are not dangerous.
If a person does not follow the rules of hygiene or his immunity weakens, anaerobic spirochetes and fusobacteria begin to actively multiply. The toxic products of their vigorous vital activity “poison” the periodontal area.
Microcirculation of fluid in tissues is disrupted, they do not receive the necessary nutrients. Necrosis occurs - destruction and “death” of cells.
Fusobacteria
General factors
Develops against the background of conditions and diseases that weaken the body’s immune defense:
- asthenia and chronic fatigue;
- diseases of the cardiovascular system;
- HIV infection, tuberculosis;
- recent acute respiratory viral infections;
- constant stress;
- long-term sleep disorders;
- endocrine disorders.
Other causes are acute poisoning, including heavy metals (mercury, lead, bismuth), smoking, drug use, and poor nutrition.
The peak incidence occurs in the winter-spring period, when the body lacks vitamins and is weakened by seasonal diseases - colds, flu, sore throat, etc. For students - during sessions from a high stress load.
Causes
People with reduced local immunity are more susceptible to pathology. Exposure to negative factors provokes the proliferation of colonies of fusobacteria and Vincent's spirochete, which leads to the development of the inflammatory process. There are general prerequisites and local factors that cause the development of necrotizing gingivitis.
Local reasons
Local reasons include:
- improper brushing technique;
- damaged teeth that irritate the oral mucosa;
- dentures of the wrong size;
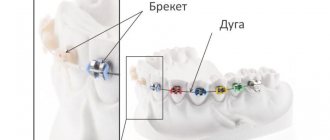
- incorrect installation of braces;
- long-term illnesses that can weaken the immune system;
- chronic infectious pathologies of the oral cavity;
- abnormal position of teeth;
- poor oral hygiene.
Common reasons
The following can provoke the development of the disease: chronic fatigue, constant lack of sleep, frequent hypothermia, hypovitaminosis, stressful situations, chronic diseases, radiation exposure, poor diet, intoxication, bad habits.
Pathology accompanies chronic serious diseases or is provoked by a combination of the above factors.
Symptoms
- Severe pain in the affected area of the oral mucosa, swelling and redness;
- ulcers covered with a whitish or dirty gray coating;
- foul breath with a strong smell of rot;
- involuntary bleeding of the gums;
- deformation of the gingival papillae - from triangular they turn into trapezoidal;
- strongly expressed tartar – abundant plaque and hard deposits.
The lesion first appears in the area of one to three teeth. In a matter of days it spreads to the entire gingival margin.
Clinical picture
Local symptoms are accompanied by general malaise. The face takes on an earthy color, the skin turns pale. Body temperature rises to 37.5-39 degrees, submandibular lymph nodes enlarge and become painful.
Patients complain about:
- headache;
- muscle weakness;
- aching joints;
- insomnia;
- problems with the stomach and intestines;
- loss of appetite.
In a general blood test, you can see increased leukocytes and ESR (erythrocyte sedimentation rate) - a laboratory indicator, changes in which indicate an inflammatory pathological process in the body.
Definition of disease
Acute, ulcerative gingivitis is an inflammatory process in the gums, which is accompanied by ulceration of the gingival tissue and its necrosis. Usually the edge of the gum and its papillae are affected, but the disease can also affect a more impressive area.
Ulcerative gingivitis occurs in an acute form. Rarely, but chronic ulcerative gingivitis also occurs.
The basis of this inflammatory process is alteration, that is, changes in the structure of tissues and cells. Usually alteration does not lead to tissue death, but in the case of gingivitis it can lead to tissue death. This article will tell you about hypertrophic gingivitis.
Diagnostics
Symptoms of pathology are visible upon visual examination. To confirm, a scraping is taken from the surface of the ulcers and the samples are checked for the presence of anaerobic and fusobacteria, spirochetes.
Differential diagnosis
The task of differential diagnosis is to distinguish Vincent's stomatitis from ulcerative inflammation of the gums, which manifests itself against the background of blood diseases - leukemia, infectious mononucleosis and agranulocytosis. To do this, they take a peripheral blood test - from the vascular bed, that is, the usual finger prick blood test.
To differentiate ulcerative-necrotizing gingivitis from allergic stomatitis, an additional bacterioscopic examination - a smear - will be required. If it is suspected that inflammation has developed due to mercury poisoning, a urine test is performed.
If the pathology appears suddenly, it is recommended to take tests for HIV infection and syphilis, and be checked for cancer.
Diagnosis methods
To confirm the presence of pathology, the dentist conducts an examination, after which the appropriate examinations are prescribed:
- a blood test to determine increased ESR and leukocytosis;
- bacteriological examination of plaque covering ulcers in order to detect spirochetes or fusobacteria and the sensitivity of bacteria to antimicrobial drugs;
- RIF allows you to determine bacterial antigens in saliva;
- the level of immunoglobulin in saliva indicates the development of a local inflammatory process;
- orthopantomography is performed to assess the condition of the jaw bones;
- Rheoparodontography allows you to determine blood circulation in periodontal tissues.
The purpose of diagnosis is not only to confirm the presence of pathology, but also to exclude secondary gingivitis, the appearance of which is provoked by pathologies of the circulatory system or tuberculosis.
You may need to consult a hematologist, immunologist or other specialist. Treatment is prescribed taking into account the updated diagnosis.
Diagnostics allows us to exclude symptomatically similar diseases:
- Acute leukemia is characterized by pale mucous membranes, infiltrates and hemorrhages. Manifested by deviations in blood test parameters.
- Lead or bismuth gingivitis - insufficient blood supply to the periodontium causes the formation of ulcers. Pathology is determined by the Rotter test, in which a solution of dichlorophenolindophenol is injected into the forearm. With a low concentration of vitamin C, it will take more than 10 minutes for the solution to discolor, which completely eliminates necrotizing gingivitis.
Forms
Spicy
The first sign is severe sharp pain in the periodontal tissues. The mucous membrane becomes bright red, and it becomes difficult to chew due to swelling and pain.
Chronic
Symptoms of a chronic course are not as pronounced as acute ones. The mouth smells unpleasant; upon medical examination, small ulcers and lesions are found in the area of the gingival margin and gingival papillae. The chronic form occurs in adolescents who systematically ignore hygiene rules.
Chronic gingivitis
Ulcerative gingivitis in children
This disease most often occurs in children aged 2 to 5 years. However, school-age children are also susceptible to it.
Important! The main characteristic symptoms of acute gingivitis in children are: swelling, redness, pain, bleeding from the gums, bad breath, general weakness, and sometimes increased general temperature. There is also a lot of deposits on the teeth and gums, and the tongue is an unnatural white-gray color.
Causes of acute gingivitis in a child:
- The child does not brush his teeth well, does not use special rinses, does not floss;
- Mechanical injuries, thermal or chemical effects on soft tissues;
- Anomalies of bite, lip or tongue frenulum;
- Prolonged teething, caries, premature removal of baby teeth;
Note! The occurrence of the disease in children is also facilitated by poor nutrition, weakened immunity, chronic and infectious diseases, and general poor condition of the body.
Treatment of ulcerative necrotic gingivitis
Therapy is aimed at eliminating the manifestations of the disease and eliminating the causes. It is carried out only by a periodontist in a clinical setting.
Local therapy
- Anesthesia
The procedures are performed only under application and infiltration or conduction anesthesia.
- Tartar removal
Soft plaque and hard deposits can be removed by professional cleaning.
- Treatment of ulcers
Necrotic masses are removed by applications of enzymes: trypsin, iruxol, etc., the area under them is thoroughly disinfected with antiseptic and antimicrobial drugs - chlorhexidine, asepta, listerine, gel with metronidazole, sanguarine.
- Drug therapy
The doctor prescribes antibiotics: metronidazole, doxycycline, trichomonacid, penicillin.
- Complete sanitation of the oral cavity
Treatment will help prevent germs from entering vulnerable tissues after procedures.
After eliminating the source of infection, patients at home rinse with antiseptic solutions and apply Metrogil-Denta gel to the affected areas of the mucous membrane until the wounds are completely healed.
General treatment
After local procedures, patients are prescribed a diet - easily digestible food high in protein, phosphorus and fluorine, and drinking plenty of fluids. Vitamin complexes are also prescribed.
With proper therapy, patients feel better within a day or two: swelling goes away, pain subsides, appetite and the ability to chew appear. Normally, after 3-6 days, signs of inflammation disappear. In the chronic form, this occurs a little later. After one or two months - a follow-up visit to the doctor. You will then need to visit your dentist every six months for a year.
Despite the optimistic prognosis, dead mucosal tissue cannot be restored. In extreme cases, gingivoplasty will be required.
Possible complications
With mild stages of the disease and timely consultation with a doctor, you can quickly get rid of unpleasant symptoms and partially restore the structure of the gums. But already deformed gums will remain that way.
Moderate and severe gingivitis can cause complications in the form of bleeding ulcers . The consequences of these disorders can be destruction and receding of the upper part of the gum. After treatment of the last stages of the disease, scars remain on the gums.
Untimely treatment allows the disease to progress from a milder form to a complex or chronic one. In advanced lesions, the likelihood of tooth loss increases. In mothers breastfeeding, this disease provokes periodontal disease, which leads to abscesses and tooth loss.
To prevent the occurrence of gingivitis, you need to exercise, follow a diet, maintain a balance of vitamins and microelements in the body, constantly carry out hygiene procedures in the oral cavity, try not to get into stressful situations, periodically visit the dentist for preventive examinations, stop smoking and drinking alcohol. The disease should not be left to chance, as untimely treatment will lead to irreversible consequences in the future.
Folk remedies for Vincent's stomatitis
The disease can only be treated with traditional dental medicine. Folk remedies will help complement the main treatment and speed up healing.
To relieve inflammation after dental procedures, rinsing with decoctions and tinctures based on:
- calendula;
- oak bark;
- St. John's wort;
- daisies.
Oak bark decoction
Prevention
The main measure to prevent the development and avoid recurrence of gingivitis is to maintain high quality oral hygiene.
Dentists also call several more preventive measures in relation to this pathology:
- Timely treatment of dental and systemic diseases.
- Quitting drinking alcohol and smoking.
- Proper nutrition and adherence to its regime.
- Regular preventive examinations and dental cleanings.
- Elimination of stressful situations.
- Strengthening the immune system.