Limb paresthesia is not a disease. This is a clinical symptom indicating trophic disorders occurring in the area of passage of a particular nerve. In order to understand what paresthesia of the limbs is and what symptoms it gives, it is necessary to take a short excursion into the anatomy and physiology of the human body.
So, every cell of the human body is controlled by the autonomic nervous system. It is connected to the central nervous system via the spinal cord, located in the spinal canal of the spinal column. Paired radicular nerves arise from the spinal cord. They pass through the foraminal openings in the vertebral bodies, branch and are directed to different parts of the body. They are the basis of the entire innervation system of the human body.
Root nerves contain two types of axons: motor and sensory. With the help of the first type, a signal is transmitted to the muscle fiber that some action is required in response to a command or external irritation. Sensitive (or sensory) types of axonal nerve fibers transmit information to the brain structures about the state of body tissues, the result of their interaction with the environment; thus, the brain learns that a cold or hot substance is touching the skin, or that a compressive or wounding effect occurs.
This article describes in detail what it is - paresthesia of the limbs, what symptoms it gives and what treatment can be used to restore impaired sensitivity. But first, we offer a definition. Paresthesia is a type of disturbance of skin sensitivity, accompanied by the sensation of crawling goosebumps, electric shocks, and increased pain that is inadequate to the force of impact.
Paresthesia of the upper and lower extremities is always associated with damage to the exclusively sensory (sensitive) type of axons. The cause may be nerve compression, inflammation, swelling, impaired microcirculation of blood and lymphatic fluid, or traumatic disruption of integrity. In order to effectively treat paresthesia of the extremities, it is necessary to first exclude the causes of its occurrence and treat the underlying disease, which is accompanied by a similar symptom.
It makes no sense to treat paresthesia separately, since the symptom of the disease can only be dealt with by eliminating pathological changes in the tissues of the human body. Accordingly, any therapy should begin with a differential diagnosis. For an experienced neurologist, just one face-to-face examination of the patient with a series of functional diagnostic tests is often sufficient to make an accurate diagnosis. In case of difficulty, radiography of the cervical and lumbar spine, MRI of large nerve plexuses, tunnels, angiography and neurography may be recommended.
In Moscow, you can make an initial free appointment with a neurologist at our manual therapy clinic. Here you will be given a preliminary diagnosis and prescribed additional examination (if necessary). The doctor will give individual recommendations for the treatment of the identified pathology.
Causes of paresthesia of the arms and lower extremities
All causes of paresthesia of the limbs can be divided into several large groups: inflammation, trauma, compression, infection and tumors. Let's look at these causes of paresthesia of the upper and lower extremities in more detail.
Let's start with the most common option - compression. This is the pressure exerted on the passing nerve fiber. It can be caused by the following negative factors:
- development of osteochondrosis of the spinal column with gradually developing protrusion, extrusion and disc herniation;
- displacement of the vertebral bodies and pinching of the radicular nerves;
- spasm and tonic muscle tension in the paravertebral region during any pathological processes;
- poor posture (scoliosis, kyphosis, lordosis, round back, stoop);
- Bechterew's disease (ankylosing spondylitis), in which there is a violation of the patency of the nerve fiber;
- deposition of calcium salts (osteophytes) on the edges of the vertebral bodies;
- violation of the patency of the tunnels in which large nerves are located (sciatic, median, ulnar, tibial, etc.);
- lymphadenitis putting pressure on regional nerve plexuses (for example, brachial).
Inflammatory diseases accompanied by numbness and the occurrence of paresthesia in certain areas of the upper and lower extremities include lymphadenitis, myositis, neuritis, etc. Infectious inflammation can be provoked by tuberculosis bacillus, staphylococcus, streptococcus (with erysipelas of the leg), Haemophilus influenzae, etc.
Among the probable causes of the development of paresthesia of the upper or lower extremities, injuries and their long-term consequences often appear:
- fractures and cracks of long tubular bones, resulting in impaired nerve conduction;
- sprains and ruptures of ligament and tendon tissue (swelling and hematoma develop, which compress the nerve fiber passing next to them);
- the formation of coarse scar tissue that interferes with the normal process of innervation of certain areas of the upper and lower extremities;
- cuts and other types of violation of the integrity of the nerve fiber itself.
As the tumor grows, pressure is exerted on the soft tissue surrounding the tumor. When a nerve fiber enters this zone, severe paresthesia is observed. Other potential causes may also include:
- incorrectly chosen position for night sleep;
- violation of workplace ergonomic rules;
- engaging in certain types of professional activities (most often, as a result of this, carpal tunnel syndrome occurs);
- the habit of sitting with one leg crossed over the other;
- development of diabetic angiopathy with impaired blood supply to distant areas of the arms and legs;
- atherosclerosis of small blood vessels against the background of high cholesterol levels in the blood;
- development of varicose veins of the lower extremities with impaired outflow of venous blood and edema syndrome;
- Raynaud's disease;
- improper application of a hemostatic tourniquet.
When you first contact your doctor, you must honestly talk about all your existing risk factors for developing nerve fiber trophism disorders. If you smoke, drink alcoholic beverages, or regularly violate your diet, you should inform your doctor about this. So, if you have recently begun to notice that you are drinking too much liquid, then you are very likely at risk of developing impaired glucose tolerance and diabetes. And these diseases can provoke the appearance of systematic transient paresthesias of the upper (arms) and lower extremities.
Changes in the oral mucosa in diseases of the nervous system - presentation
Changes in the oral mucosa in diseases of the nervous system. Ananyev Alexander Dmitrievich 4th year, 5th group
Glossalgia. Stomalgia. Glossalgia - paresthesia of the tongue (burning, tingling, tingling, numbness). Stomalgia is a disease manifested by constant pain and paresthesia in the mucous membrane of the oral cavity and tongue.
Etiology and pathogenesis Currently, these diseases are polyetiological diseases. In pathogenesis, the main role belongs to the pathology of the autonomic nervous system, which is supported by irritation of the neuro-reflex circuit at its various levels. Glossalgia and stomalgia most often develop against the background of diseases of the gastrointestinal tract and liver, vascular lesions, diseases of the central and peripheral nervous system, and endocrine disorders. Common diseases that lead to disorders of the nervous system cause a decrease in the threshold for the perception of irritations, which contributes to the development of the disease.
Clinical picture of stomalgia Burning of the tongue, which sometimes affects the entire oral mucosa; patients describe the symptom as “as if sprinkled with hot pepper”; The occurrence of unusual sensations, “it seems like goosebumps are crawling in the mouth” (tingling, swelling, scratching) in all parts of the oral cavity or in a separate part of it (the side surface and tip of the tongue, gums, palate and pharynx).
Clinical picture Some patients experience a decrease or increase in pain sensitivity in the oral cavity, and taste sensations change; An unreasonable increase in salivation is not uncommon; 1/3 of patients may experience constant dry mouth, with saliva becoming thick and viscous, and externally foamy-white.
Clinical picture of glossalgia Complaints 1. Constant or periodic burning 2. Tingling in the tongue 3. Dry mouth 4. Feeling of fatigue after speaking 5. Pain in the tongue 6. Unpleasant sensations intensify with excitement, in the evening
Clinical picture Objective changes in the tongue with glossalgia are absent or insignificant (swelling, slight atrophy of the tongue papillae). Pain and discomfort are often concentrated on the tip of the tongue (anterior third) and the lateral surface, less often on the back and root (posterior third) of the tongue. As a rule, all discomfort disappears while eating.
Clinical picture Those suffering from glossalgia experience pronounced neuropsychic disorders: an unbalanced psycho-emotional state with a tendency to depressive reactions, anxious suspiciousness, poor sleep.
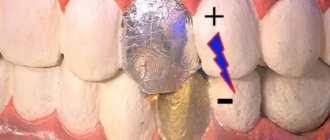
Clinical picture Local irritants are of particular importance: sharp edges of damaged teeth, defective dentures, dentition defects, galvanic syndrome phenomena, decreased height of the lower part of the face.
Differential diagnosis Neuralgia of the lingual nerve Severe paroxysmal pain in one half of the tongue occurs suddenly during eating, talking, and radiates along the nerve. Often combined with neuralgia of the third branch of the trigeminal nerve. There is often a history of severe hypothermia. Outside of attacks there is usually no pain.
Differential diagnosis Neuritis of the lingual nerve The pain is unilateral and localized in the anterior two-thirds of the tongue. In the same area, superficial sensitivity is partially or completely lost, which manifests itself in a feeling of numbness and paresthesia, sometimes a decrease or perversion of taste. The pain is constant, intense, aggravated by eating and talking.
Differential diagnosis Allergy to plastic A burning sensation occurs soon after the start of using removable dentures made of acrylic plastic. Swelling and hyperemia of the oral mucosa correspond to the boundaries of the prosthesis. Complaints and hyperemia disappear a few days after stopping the use of prostheses. Positive allergy tests to plastic.
Differential diagnosis Desquamative glossitis Pain in the tongue appears and intensifies when eating irritating foods. Characteristic foci of desquamation of the filiform papillae of the tongue in the form of reddish spots that tend to constantly migrate.
Differential diagnosis Candidiasis History of taking antibiotics, glucocorticosteroids, diabetes mellitus. The mucous membrane of the oral cavity is hyperemic, there is a white coating on the back of the tongue and in the folds. Bacterioscopy reveals an abundance of Candida fungus, mycelium, and blastospores.
Differential diagnosis Vitamin B12 deficiency Complaints of severe pain when eating irritating foods. “Lacquered” tongue of crimson color, bright crimson stripes and spots on the mucous membrane of the cheeks.
Treatment General treatment Antidepressants Tranquilizers (Elenium, tazepam, phenazepam, etc.) B vitamins Stimulation of salivation (1% pilocarpine solution) Treatment of identified concomitant diseases
Treatment Local treatment Trimecaine blockades of the lingual nerve (610 blockades with a 1% trimecaine solution every other day or daily) Iron preparations (gemostimulin, ferroplex, ferrocal, etc.) Keratoplastics Local anesthetics in the form of applications and oral baths Physiotherapy (1% solution of vitamin PP, 25 % sodium chloride solution)
Taste disturbance Taste disturbance or taste sensitivity disorder can manifest itself in its complete loss, decrease, increase and perversion. This applies to all types of taste sensitivity or just some of them. Taste disturbances can occur due to injuries, lesions of the oral mucosa, vitamin deficiencies, diseases of the gastrointestinal tract, peripheral nerves, central nervous system, and neuroses.
Taste disturbance Unilateral taste disturbance on the anterior two-thirds of the tongue indicates damage to the peripheral nerve of the chorda tympani, lingual nerve, facial nerve, and solitary fasciculus. Taste fibers are located next to other fibers almost along their entire path, therefore, simultaneously with damage to the peripheral taste nerves, other types of innervation are usually disrupted, which makes it possible to determine the location of the lesion (for example, when the lingual nerve is damaged, all types of superficial sensitivity of the tongue are disrupted).
Taste disturbance Bilateral, less often unilateral, complete loss of taste occurs with organic lesions of the central nervous system (brain tumors, neurosyphilis). Perversion of taste or loss of taste is not uncommon during hysteria.
Clinic 1. total ageusia - inability to distinguish between sweet, salty, bitter and sour tastes; 2. partial ageusia - impaired ability to perceive certain taste sensations; 3. specific ageusia - inability to distinguish the taste of certain substances; 4. total hypogeusia - decreased taste sensitivity to all substances; 5. partial hypogeusia - decreased taste sensitivity to certain substances; 6. dysgeusia - perversion of taste sensations, i.e. incorrect sensation of taste of a particular substance, or taste sensations in the absence of a taste stimulus.
Treatment Treatment methods for patients with taste disorders are few. When changing the composition of saliva, the use of artificial saliva is effective. If necessary, it is advisable to treat bacterial and fungal diseases of the oral cavity. If the patient’s general condition allows, a positive effect can be obtained by discontinuing medications that impede cell regeneration. In some cases, a certain improvement is achieved by using zinc preparations and vitamins. There is no specific treatment for sensory-neural taste disorders.
Salivation disorders 2 types of salivation disorders Hypersalivation Hyposalivation
Hypersalivation Long-term sharp hypersalivation (increase in the amount of saliva by 2-3 times) is observed with some organic lesions of the autonomic centers: parkinsonism, pseudobulbar palsy, post-stroke hemiplegia. In parkinsonism, hypersalivation can be combined with impaired swallowing. This leads to saliva leaking from the mouth and constant spitting. Increased tone of the vagus nerve (vagotonia) of various etiologies, helminthic infestation also lead to increased salivation. False hypersalivation often occurs, when patients complain of excessive salivation, but this is not confirmed by objective examination. This phenomenon occurs in neurosis accompanied by obsessive states, as well as in violation of the act of swallowing in the case of organic lesions of the central nervous system.
Hyposalivation Hyposalivation and, especially, its extreme manifestation xerostomia, cause patients a feeling of dryness in the oral cavity, difficulty eating and speaking, pain from spicy and hard foods, a burning sensation, and roughness of the mucous membrane. An increase in the tone of the sympathetic nervous system can also lead to hyposalivation, for example, in hyperthyroidism, during menopause, and in neurotic conditions. As a temporary phenomenon, xerostomia can occur during acute infectious diseases and poisoning (botulism), after taking certain medications (for example, atropine).
Treatment Hypersalivation Elimination of the underlying disease. A temporary reduction in salivary secretion can be achieved by using atropine preparations. Hyposalivation Elimination of the cause that caused hyposalivation, Sanitation of the oral cavity. Vitamin therapy (A, B1, B2, B6, B12, C, E), Sex hormones (according to indications).
Transient paresthesias in the limbs
Transient paresthesia in the limbs - what is it and why is such a condition dangerous? Let's expand. So, paresthesia is a violation of sensitivity due to damage to the sensory nerve fiber. Transient paresthesia is a type of sensitivity disorder that occurs suddenly and, a few minutes after the elimination of the negative influence factor, disappears without a trace without drug intervention.
The most common transient paresthesias in the extremities occur when the position for night sleep or prolonged sitting is chosen incorrectly (for example, in public transport). If you immediately stand on your feet after a night's sleep in an uncomfortable position, you may feel that your limbs are not obeying. A person in such a situation may even fall.
If you sit for a long time with one leg crossed over the other, then in the lower leg area you may feel a decrease in skin sensitivity, crawling and mild pain. After the legs are lowered to the floor, these sensations pass. These are transient paresthesias in the limbs. They are usually associated with exposure to external pathogenic factors. Internal diseases are not detected with such paresthesias.
Change in taste
Changes in taste recorded in 68% of patients. It has been proven that changes in taste have a peripheral origin, because After anesthesia, the sensation goes away.
As a rule, we are talking about a decrease in taste sensitivity, its complete loss or perversion, the latter is typical for bitter products.
Changes in taste are also characteristic of many diseases of the digestive tract, some types of neuroses, tongue injuries, and neuralgia.
Due to the fact that the main “sensors” of taste are located on the tongue - the papillae, various infectious and non-infectious diseases can provoke a decrease in sensitivity, but this type of decrease in sensitivity is still reversible.
Changes in the sensitivity of the anterior third of the tongue indicate damage to the peripheral nerves.
Due to the fact that the taste buds are located next to the nerves, damage to the peripheral innervation provokes the involvement of other types of nerves in the process, which will facilitate the diagnosis.
Changes in taste perception of the posterior third of the tongue - the glossopharyngeal nerve is affected. Bilateral or unilateral loss of sensitivity indicates brain damage - neurosyphilis, tumor processes. Perversion of taste is also characteristic of hysterical states.
We suggest you read: How to treat the oral cavity with chickenpox
Symptoms of paresthesia of the limbs with osteochondrosis
Osteochondrosis (degenerative dystrophic disease) of the spinal column is the leading cause of the development of constantly present paresthesias in the upper and lower extremities.
Symptoms of paresthesia of the lower extremities with osteochondrosis are as follows:
- there are acute pains in the region of the spine that is responsible for the innervation of the limbs;
- first, numbness occurs in individual areas;
- then pain appears, radiating to the arm or leg;
- unpleasant sensations are unilateral (on the side of the affected radicular nerve);
- paresthesia does not go away with changes in body position.
If paresthesia appears during osteochondrosis, this is a negative sign for further prognosis. At a minimum, the patient develops protrusion of the intervertebral disc and severe radicular syndrome. If treatment is not started, atrophy of the nerve fiber and complete loss of skin sensitivity along the affected nerve are possible.
Main symptoms: dentistry
The most typical symptom is glossalgia - a symptom complex that combines the following symptoms:
- Xerostomia or, conversely, increased salivation;
- Burning sensation in the tongue and throughout the mouth;
- Impaired taste perception;
- Paresthesia;
- Painful sensations of varying degrees of intensity;
- And etc.
Despite lengthy research, doctors have not found the exact cause of these symptoms and xerostomia in particular.
https://www.youtube.com/watch?v=ytpressru
As a rule, the manifestation of symptoms in the oral cavity begins in the age group after 40–50 years, more often in women.
This circumstance allowed us to make the assumption that xerostomia is associated with menopause and a decrease in hormonal activity. This theory has its supporters and opponents.
Disturbances in trophism and transmission of nerve impulses in the oral cavity result in a burning sensation - the main manifestation of the pathology of the nervous system.
Despite the length of time spent studying this issue. Scientists have not been able to find a clear cause of this syndrome or the mechanism of its development.
The medical term syndrome refers to a whole group of symptoms; accordingly, burning mouth syndrome will be manifested by pain, burning in the mucous membrane and tongue, impaired salivation and changes in taste.
A long-term study of the effects of body pathologies on the work and functions of the oral cavity has made it possible to identify the main symptoms, each of which will be characteristic of a specific disease.
Dentistry – pain in the oral cavity, and with difficult localization.
Characteristics of pain may vary:
- superficial,
- deep,
- tip of the tongue or spread throughout the organ,
- move to the mucous membrane, pharynx and even lips,
- Dentistry is often combined with a burning sensation in the mouth, xerostomia, and taste disturbances.
This complex of unpleasant sensations provokes irritability and disrupts social adaptation. The level of pain, although different in nature, is equal in intensity to toothache.
This symptom is characteristic of most diseases of the nervous system that are associated with circulatory disorders - neurosyphilis.
Carrying out dental procedures and trauma to the mucous membrane from tooth fragments and dentures can intensify the symptoms of the disease.
We invite you to read: Correction of open bite in children and adults
If left untreated, symptoms can persist for a long time, alternating between moments of remission and exacerbation.
In patients with dentistry, it turns out that in painful areas it is reduced, and patients have mental manifestations - hidden depression.
https://www.youtube.com/watch?v=https:accounts.google.comServiceLogin
Patients themselves tend to focus their attention on the slightest pain and become completely immersed in the disease, exaggerating their sensations.
Before treating limb paresthesia
It is very important, before starting to treat paresthesia of the extremities, to conduct a differential diagnosis and exclude the possibility of developing dangerous infections and malignant neoplasms that compress the nerve fiber. To diagnose a disease that causes paresthesia of the limbs as a clinical symptom of its course, the following examination methods are used:
- X-ray image of the spine (in case of paresthesia of the upper extremities, you need to take an image of the cervical and cervicothoracic region, in case of damage to the lower extremities - lumbar and lumbosacral);
- angiography and neuromyography - allow you to evaluate the conductivity of the nerve impulse and the condition of sensory axons;
- Dopplerography of blood vessels allows us to exclude atherosclerosis, narrowing of the lumen due to diabetes mellitus and the development of varicose veins;
- Ultrasound of soft tissues to exclude the risk of developing focal infections and tumors;
- MRI and CT if it is difficult to make an accurate diagnosis.
You can start diagnosing by visiting a neurologist. In Moscow, this doctor conducts initial free consultations with patients in our manual therapy clinic. Make an appointment at a time convenient for your visit.
Treatment of paresthesia of the upper and lower extremities
To treat limb paresthesia, it is important to identify the underlying disease. This condition is only a conical symptom and does not require separate therapy. Moreover, treatment of paresthesia of the upper extremities (as well as the lower ones) separately from the underlying disease will not bring a positive result.
Thus, if paresthesia of the lower extremities is associated with the development of an intervertebral hernia in the lumbar spine, then treatment must begin with a procedure of traction traction of the spine. During this effect, the intervertebral spaces will be increased and the compression exerted on the radicular nerves will be completely eliminated. The pain will go away and the paresthesia syndrome will disappear. Then the doctor develops an individual course of treatment for osteochondrosis.
It may include osteopathy and massage, reflexology, kinesiotherapy, therapeutic exercises and much more. Paresthesia of the upper extremities with brachial plexitis is treated in a similar way. First, the doctor finds the cause of the damage to the structure of the brachial nerve plexus. Then he applies techniques to restore physiological nerve conduction. And only after this begins treatment of the identified disease.
If you require treatment for paresthesia of the lower or upper extremities, then make an appointment for a free appointment with a neurologist at our manual therapy clinic in Moscow. After the examination and diagnosis, the doctor will tell you about all the possibilities and prospects for using manual therapy methods in your individual case.