Symptoms of acute tooth pulpitis
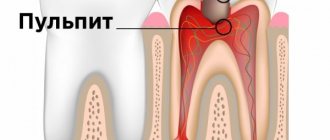
All types of pulpitis have one common feature: damage to the pulp - connective tissue with a large number of microvessels and nerves. It is the presence of a large number of nerve endings that explains the fact that the disease is almost always accompanied by severe pain. Acute pulpitis is considered a signal that pathogenic bacteria have entered the tooth cavity and caused inflammation. Despite the fact that this form is often the initial stage of pulp damage, it causes a number of very unpleasant sensations in the patient from the very beginning.
List of characteristic features
- Sudden attacks of acute pain (on average 10–20 minutes), worsening at night and usually subsiding during the day.
- Reaction to stimuli (usually hot and cold).
- Painful sensations can be localized both within the tooth and can be felt in the temples, ears, and even in healthy teeth (in the second case, these are symptoms of diffuse pulpitis).
The average duration of acute pulpitis is about two weeks. After this period, the disease usually acquires a chronic stage. Due to the gradual destruction of nerve fibers, the pain becomes aching, less pronounced, but longer lasting. Of course, acute pulpitis does not occur on its own, but is a consequence of bacterial activity.
Forms of pulpitis
According to the nature of the inflammatory process:
- acute is the first stage of inflammation, which lasts from 3 to 5 days. At this stage, inflammation affects only the coronal part of the pulp;
- chronic - if acute pulpitis is not treated in time, it becomes chronic. The dental nerve begins to gradually die, dead tissue accumulates in the tooth cavity, and the pain is mild or completely absent. May occur with periodic exacerbations.
By localization of inflammation:
- deep root pulpitis - the infection spreads along the entire length of the root canal and can extend beyond its limits through the apex (apical foramen);
- pulpitis under a filling – secondary caries that forms under a filling can also cause pulpitis;
- two- and three-channel pulpitis - the inflammatory process develops in molars and premolars and covers all root canals, which complicates the task for the dentist.
Pulpitis of temporary teeth is also a common occurrence. Baby teeth in children have weak enamel and a wide pulp chamber, so inflammation of the dental nerve develops rapidly. The danger is that the infection can get into the periodontal tissues and damage the buds of permanent teeth.
Causes of acute pulpitis
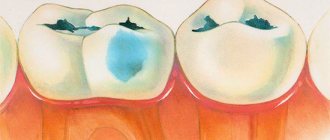
- Complications of caries. Neglected or incompletely cured caries leads to the penetration of streptococci into the pulp through the dentin tubules - bacteria that have an acid-forming function and thereby create the foundation for the development of infection.
- Injuries of a mechanical or chemical nature that violate the integrity of the tooth. Without a protective layer of enamel and dentin, the pulp becomes extremely vulnerable to bacteria and the effects of the external environment.
- Gum disease in which infection spreads through open periodontal pockets.
- Unsuccessful dental treatment (infection, damage to tooth tissue, etc.).
Definition of disease
Simply put, pulpitis is an inflammation of the dental nerve accompanied by unbearable pain.
The disease affects:
- connective tissue;
- periosteum;
- periodontium - a complex of soft fibers surrounding the tooth and holding it in the alveolar socket;
- bone trunk.
Pulpitis (classification, diagnosis, treatment) is identified as a separate area of dentistry. With this disease, dental tissues react sharply to external stimuli, especially to temperature effects.
The pain intensifies at night. In terms of prevalence, pulpitis is second only to caries. Every 5th patient goes to the dentist with this particular disease. According to the WHO classification, pulpitis is assigned code KO4.0.
This disease is defined as acute or chronic inflammatory pathology of the pulp. The destructive process affects periapical tissues. Pulp is the loose structure of connective fibers that fill the dental cavity.
They contain nerve endings, blood vessels and lymphatic vessels. Inflammation of this connective tissue, which is responsible for nourishing the teeth, is called pulpitis.
Functions of the pulp:
- plastic, which is realized due to the biological activity of odontoblasts that form the peripheral layer of tissue;
- protective – production of IgG immunoglobulin, disposal of dead cells, formation of tertiary dentin;
- trophic, carried out thanks to the developed vascular network;
- sensory, due to the presence of a large number of nerve endings;
Inflammation of the pulp not only causes severe pain, but also leads to tissue necrosis, which can lead to tooth loss and infection of the entire salivary-jaw apparatus.
Acute diffuse pulpitis
Usually it is the next stage of focal pulpitis (sometimes the peak form of chronic) and appears on the third or fourth day. With diffuse pulpitis, inflammation affects both the coronal and root parts of the pulp. The pain is paroxysmal and long-lasting, with periods of relief being rare. The pain is often radiating and radiates to various parts of the head. The fabric begins to become saturated with exudate.
Some sources also highlight acute fibrous pulpitis, but this is not entirely true. Fibrous pulpitis is a form of chronic; acute fibrous pulpitis is also not a completely correct term. It is a chronic complication of diffuse pulpitis. When gangrenous, extensive tissue necrosis occurs and the tooth often takes on a characteristic gray tint.
Treatment of pulpitis
Pulpitis requires repeated visits to the dentist. Treatment of the initial stage of damage to incisors and canines takes 1–2 visits, more complex cases require 3–4 visits to the doctor. With serous pulpitis, complete recovery is possible with preservation of tissue viability. The first stage of therapy is opening the pulp chamber and removing carious areas. Further steps depend on the degree of tissue damage.
1. Conservative treatment
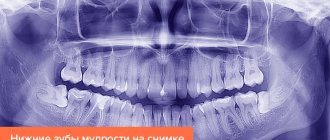
Drug therapy is recommended at the onset of the disease, if it is not aggravated by the inflammatory process. Antibiotics may be prescribed to stop the infection. At the next appointment, using an x-ray, they check whether the inflammation has been eliminated. If the dynamics are positive, a permanent filling is installed. Otherwise, more drastic measures are required: removal of the entire pulp. If you keep the pulp in the canals, the tooth will continue to be nourished and strengthened by dentin.
Devital extirpation
During the first appointment, the carious cavity is opened so that the doctor has access to the pulp. A devitalizing paste is placed there. Namely, today it continues to be briefly called “arsenic”. However, in fact it is a paste based on formaldehyde, resorcinol and paraformaldehyde. They are safe compared to arsenic compounds and are non-toxic. You can walk with a devitalizing paste, which is fixed with a temporary filling, for one week. Usually within 7 days it completely kills the pulp tissue. After the specified period, the dentist removes the paste; it cannot be left in the tooth cavity longer, otherwise it will poison the adjacent tissues, and the tooth will soon crumble.
At the next appointment, the doctor removes the pulp. Large, curved canals are carefully cleaned with special instruments. This procedure is called nerve ablation. Next, the empty canals are disinfected and filled with filling material. It is necessary to fill them completely, otherwise there is a risk of re-inflammation; for this, the doctor measures the length of the canal with apex locator electrodes. They are lowered into each channel, since their length can be different. The obtained data is compared with an x-ray.
The canal is treated, disinfected, and dried. Afterwards, the doctor fills it with special material. Our clinic uses the method of three-dimensional obturation of root canals with thermally modified gutta-percha. Gutta-percha pins are placed in the canals so that the sealer does not reach the upper hole by a few millimeters. Part of the pin is heated and removed. The dentist can monitor the process using x-rays.
When the canals are filled, the dentist again places a temporary filling. It is necessary for the gutta-percha to completely dry out and remove all moisture from it. This takes 4-5 days, after which you can install a permanent filling and restore the tooth.
The main disadvantage of devital extirpation is the duration of treatment, consisting of several visits to the doctor’s office:
- The first step is to open the pulp, remove carious lesions and apply a devitalizing paste.
- The second visit is to remove the nerve, clean the canals and fill them with gutta-percha.
- The final stage is filling and restoration of the tooth.
Diagnosis of acute pulpitis
Diagnosis of acute pulpitis includes several stages. First, the doctor conducts a visual examination of the oral cavity: if the tooth has a carious cavity or is injured, and the patient complains of acute pain, then there is a high probability that we are talking about pulpitis. Acute and chronic pulpitis have quite significant differences, so visual diagnosis alone is impossible.
Each of the forms of acute pulpitis (they will be discussed later) has its own manifestations and characteristics. To identify the type and stage of the disease, specialists resort to x-rays and electroodontic diagnostics (EDD), which determines the reaction of the pulp to electric current. Rheodentography (assessment of the blood supply to the pulp) and a thermal test are also quite often performed. In addition, differential diagnosis of acute pulpitis is necessary in order to make an accurate diagnosis and not confuse pulpitis with other diseases with similar symptoms.
Symptoms
The main symptom of this disease is throbbing toothache. It can radiate to the head and ears, so people with pulpitis sometimes go for help not to the dentist, but to an ENT doctor. The pain intensifies at night, when chewing food, and when the tooth is exposed to low or high temperatures. In addition, pulp inflammation may be indicated by:
- gray enamel of a diseased tooth;
- the presence of an open cavity in the tooth;
- bleeding from a tooth;
- insomnia;
- irritability.
Nonspecific signs of pulpitis include headache and fever.
Treatment of acute tooth pulpitis
Treatment of caries, pulpitis and acute periodontitis forms the basis of the activities of any dental clinic. It is important for the patient to find a doctor whom he can trust with his health. Below is a table that describes the main types and methods of treating acute dental pulpitis.
Treatment methods for acute pulpitis
✔
Classical technique: tooth depulpation, removal of affected tissue and filling.
✔
Biological method of treating acute forms of pulpitis with partial preservation of the pulp. It is carried out in two visits. The first stage involves preparing the tooth, applying therapeutic and insulating spacers, and installing a temporary filling. At the second appointment, a visual inspection and fixation of the permanent filling is performed. This type of treatment is possible only with minimal inflammation of the pulp and at a young age (up to 26-27 years).
Treatment of acute diffuse pulpitis in the vast majority of cases requires complete removal of the pulp. A biological method with the possibility of preserving part of it is possible in a minimal percentage of cases.
Diagnostics
The doctor must be able to distinguish chronic pulpitis, the classifications of which we have examined, from deep caries, since in the treatment of these diseases they resort to different treatment methods. When a tooth is affected by caries, the acute pain that occurs when the unit comes into contact with the irritant subsides immediately after the latter is removed. In the case of pulpitis, it can remain for a long time.
To distinguish pulpitis from chronic periodontitis, you just need to knock on the tooth. With periodontitis, tapping will cause discomfort.
When a person has hypertrophic pulpitis, the tooth begins to bleed at the slightest mechanical impact.
In the case of fibrous pulpitis, the pulp can be seen in the carious cavity under a thin layer of dentin. If the dentist touches this place with a probe, the tooth will “respond” with sharp pain.
To distinguish pulpitis from inflammation of the trigeminal nerve, it is worth remembering that with tooth pathology, painful sensations intensify at night, and with neuralgia, the opposite is true.
Diagnosis of pulpitis consists of the following stages:
- Detailed survey.
- Examination of the oral cavity.
- Probing.
- Temperature test.
- Electroodontodiagnostics.
- Radiography.
Treatment of complicated stages of acute pulpitis
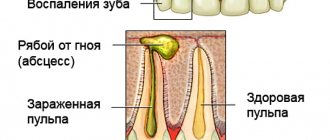
Focal and diffuse pulpitis have their own varieties. The first has serous and purulent forms. Focal acute serous pulpitis often occurs as a complication of caries or during improper treatment of caries. It affects the root part of the pulp, which causes sharp attacks of pain. Diffuse serous acute pulpitis spreads to both the coronal and root parts of the pulp, causing severe swelling, which can develop into phlegmon.
Acute purulent pulpitis (pulp abscess), as the name suggests, is characterized by the accumulation of pus in the pulp chamber, throbbing pain, which can radiate to various parts of the jaw and head (which is why the patient often cannot identify the diseased tooth). For successful treatment, it is necessary to completely remove the pus from the canals, and in most cases the tooth is subsequently killed. Treatment of acute traumatic pulpitis is usually more difficult.