Sialadenitis of the submandibular salivary gland (submandibulitis) is an inflammatory process that disrupts the function of salivation, which is important for digestion. Pathology can be primary or secondary. More often it develops against the background of other infectious processes in the oral cavity and distant organs.
Sialadenitis of the submandibular salivary gland (diagnosis and treatment) is a qualification of a dentist, who should be contacted if symptoms of the disease appear.
Content
- What is submandibular sialadenitis
- Classification of acute and chronic forms of submandibulitis
- Clinic: manifestations and symptoms
- Diagnostics
- Clinical and laboratory diagnostic methods
- Instrumental diagnostic methods
- Treatment of sialadenitis of the submandibular salivary gland
- Drug treatment of submandibulitis
- Etiotropic therapy
- Pathogenetic therapy
- Symptomatic drugs and doses
- Physiotherapy
- Treatment at home
- Treatment of calculous sialadenitis
- Surgical treatment
Tumors of the salivary glands
About 60% of all diagnosed neoplasms of the salivary glands are benign in nature. These are adenomas, adenolymphomas, papillary cystadenolymphomas and polymorphic tumors. The remaining 40% are intermediate stages (mucoepidermoid neoplasms and carcinomas), as well as sarcomas and cancers, accounting for 10-25% of cases.
To make a correct diagnosis, a complete examination is necessary, which includes, in addition to the standard set of laboratory tests, diagnostic methods such as:
- Ultrasound;
- X-ray examination;
- MRI;
- biopsy;
- histological examination.
In most cases, surgical treatment is indicated, which consists of removing the tumor node.
What is submandibular sialadenitis?
Submandibular or submandibular sialadenitis develops when an infectious agent enters the gland of the same name. Another reason may be a blockage of the duct when foreign bodies penetrate into it or stones form. In the second case, calculous sialadenitis is diagnosed, and its treatment is very different from other forms.
Primary sialadenitis can be caused by viral infections, various fungi and bacteria. They enter through the oral cavity, along with blood, lymph and contact. Non-infectious sialadenitis occurs when poisoned with salts of heavy metals, when they are excreted along with saliva.
The submandibular gland is paired, therefore left-sided, right-sided and bilateral sialadenitis can be diagnosed. There is also a possibility of damage to several glands at once: parotid, sublingual, minor salivary glands.
Classification of acute and chronic forms
Sialadenitis can occur acutely or chronically. Each form has its own manifestations. Acute serous sialadenitis without treatment turns into purulent. Chronic inflammation develops after acute inflammation, then the symptoms subside somewhat, but pathological changes increase, and treatment has not been fully carried out.
Classification of sialadenitis:
- Acute - viral (influenza, epidemic, cytomegalovirus) and bacterial (lymphogenous, postoperative, contact, obstructive).
- Chronic - parenchymal (inflammation of the parenchyma), sialodochitis (damage to the ducts), interstitial (inflammation of the connective tissue stroma).
Subacute and chronic processes occur more often in the submandibular gland. The main risk factor is saliva retention, but the formation of stones in this gland is rare. Long-term chronic inflammation can lead to atrophy.
Clinical manifestations and symptoms
Due to the retention of saliva inside the gland ducts, the gland swells, which is accompanied by paroxysmal pain. After eating, the swelling subsides and remains moderate with a long course of the disease.
With chronic inflammation, you can see swelling of the sublingual fold and papilla (the place where the duct opens into the oral cavity). Pressing on them is accompanied by the release of cloudy saliva. In subacute cases, pus may come out.
In acute sialadenitis, the sublingual fold is greatly enlarged and thickened. Inflammation is accompanied by general symptoms of intoxication. The patient has:
- body temperature rises;
- worried about weakness;
- headache appears;
- regional lymphadenopathy (enlarged lymph nodes).
When pressing on the gland, purulent exudate is released from it.
Symptoms of the disease
The main symptoms of sialadenitis include the following:
- pain while chewing;
- redness, swelling of the cheeks, neck;
- violation of taste perception;
- unpleasant taste in the mouth;
- dry mucous membranes;
- general deterioration of health;
- difficulty opening the mouth.
In acute sialadenitis, symptoms increase quickly and can also subside quickly. However, in the absence of proper treatment, the disease can become chronic, so even if you feel better, it is important to consult a dentist.
Lack of therapy can cause complications, the most common of which include the formation of ulcers (abscesses), secondary infection - the addition of a bacterial infection to a fungal infection, etc. This will require more serious intervention and long-term treatment, so you should not postpone a visit to the doctor.
Diagnostics
Sialadenitis can be diagnosed by several specialists, depending on age, main complaints, and concomitant diseases. A preliminary diagnosis can be made by:
- dentist;
- surgeon;
- pediatrician;
- infectious disease specialist;
- venereologist;
- rheumatologist;
- phthisiatrician
Differentiation of various forms of inflammation is possible through instrumental and laboratory diagnostics. The initial visit to the patient includes examination of the gland, palpation, and medical history. After this, the doctor prescribes the necessary tests.
Instrumental diagnosis of submandibulitis
For submandibular sialadenitis, intraoral radiography is prescribed. It allows you to see the stones. For more detailed visualization of pathological changes, ultrasound is prescribed.
Additionally carried out:
- sialography;
- sialotomography;
- thermography;
- sialoscintigraphy.
The methods allow one to distinguish inflammation from salivary stones, cysts, tumors, regional lymphadenopathy, and sialoadenosis.
Treatment of sialadenitis of the submandibular salivary gland
Complex treatment of sialadenitis includes drug therapy (symptomatic and etiotropic), physiotherapy, general strengthening measures, surgical removal of stones and the gland itself in severe cases of the disease.
In chronic cases, drug therapy is supplemented with physiotherapy and massage. If conservative measures are ineffective, surgery is performed on the submandibular salivary gland.
Drug treatment
The main drugs for sialadenitis are antiviral or antibiotics, non-steroidal anti-inflammatory drugs, local antiseptics, painkillers. For viral inflammation, mouth irrigation with interferon is prescribed. In bacterial cases, proteolytic agents and antibiotics are instilled directly into the gland duct.
Etiotropic therapy
Etiotropic treatment includes the use of antiviral or antibacterial agents, depending on the origin of the disease.
For viral inflammation, the drugs Viferon, Interferon, Laferon are prescribed for a course of 5-7 days. Treatment may be extended. Lozenges are used 3-4 times a day after meals.
Antibacterial therapy is carried out more often with Penicillin or Gentamicin. The medicine is injected directly into the gland, and in severe cases it is taken orally.
Pathogenetic treatment
To increase salivation, the patient is prescribed a 1% solution of pilocarpine for oral administration, 4 drops. This promotes contraction of the smooth muscles of the ductal apparatus, which facilitates the outflow of secretions. To eliminate the inflammatory process, novocaine blockades can be performed.
Compresses with 30% demixide are applied locally to the affected area. The procedure is carried out once a day for 25 minutes. A mandatory recommendation during treatment will be to follow a diet. The patient should eat salivary foods, which include crackers, lemon, sauerkraut, and cranberries.
Symptomatic treatment
To eliminate symptoms, painkillers, antipyretics, and anti-inflammatory drugs are used. NSAIDs have such actions - Ibuprofen, Nimesulide, Ketanov, Nise, Paracetamol. They are taken as needed when there is pain and fever. Usually one tablet is prescribed 2-3 times a day during periods of severe symptoms.
Physiotherapeutic methods in the treatment of the salivary gland
During the period of remission of sialadenitis, therapy is supplemented with physiotherapy. UHF, electrophoresis with galantamine, galvanization, and fluctuarization are more often prescribed. Chronic sialadenitis is also treated with these procedures and massage.
Forms of chronic inflammation
Chronic inflammatory diseases of the salivary glands vary in form. Interstitial sialadenitis - observed in 85% of patients with damage to the parotid glands, more often in women and in old age. It is asymptomatic for a long time.
Progresses slowly, accompanied by a gradual narrowing of the ducts. An exacerbation begins suddenly, the gland becomes enlarged, painful, but has a smooth surface. After therapeutic measures, the size does not return to normal.
Parenchymatous - also almost always affects the parotid glands. Patients are of any age; women are more likely to get sick. The hidden current lasts for many years. The clinical picture of an exacerbation does not differ from acute sialadenitis. In the initial stage, patients note the appearance of abundant salty mucus in the mouth when pressing on the parotid area.
Then pain, thickening, lumpiness of the gland, and pus in the saliva appear. Dryness, painful swallowing or chewing are not typical.
Sialodochitis is the name given to isolated lesions of the ducts. It often develops in old age due to the anatomical expansion of the excretory tract. The main symptom is excessive salivation when eating and talking. This contributes to the formation of jams in the corners of the mouth.
Treatment at home
At home, treatment includes taking medications prescribed by a doctor, following a diet, and using folk remedies. Some recipes can be used for sialadenitis, but only to eliminate individual symptoms and improve overall well-being. Home remedies cannot cure sialadenitis and must be approved by the person treating it.
Alternative treatment that can be carried out along with drug therapy:
- Ointment based on tar. A spoon of Vaseline is mixed with ten spoons of tar. The product is applied to the skin in the gland area 2 times a day.
- Yarrow tincture compress. The flowers of the plant are passed through a meat grinder, poured with boiling water, and infused for a week. Gauze soaked in the solution is applied to the affected area for 20 minutes once a day.
- Propolis and mumiyo. Chew the mummy every day for a month, then drink half a spoon of propolis tincture.
Every day during the treatment period, you can rinse your mouth with decoctions of chamomile, calendula, and sage. Also, to stimulate the immune system, it will be useful to take echinacea tincture 30 drops 3 times a day.
Timofeev 1-3 volume / volume 2 / 23. NON-TUMOR DISEASES OF SALIVARY GLANDS / 23.4. SIALOSES
23.4. SIALOSES
Synonyms: sialadenosis, sialozoadenitis, interstitial sialadenitis, symptomatic sialopathy, hypertrophic sialosis, benign salivary gland hypertrophy
and etc.
The term "sialosis"
was introduced by S. Rauch in 1956. This term combines dystrophic diseases of the salivary glands, which are caused by general disorders in the body and lead to pathological changes in secretion. Inflammatory changes in the glands are considered secondary, which arise as a result of infection entering the gland through the ductogenic route (due to decreased salivation). This term emphasizes the primarily non-inflammatory nature of the disease. The term was adopted by WHO and included in the International Histological Classification of Tumors of the Salivary Glands in 1974 in the group “tumor-like lesions”, as well as in 1991.
Etiology.
Depending on the reasons that cause dystrophic changes in the large salivary glands, sialoses were divided by many scientists into separate groups. To date, many classifications of sialosis have been proposed (S. Rauch, 1959; G. Siefert, 1966; V.S. Kovalenko, 1970; I.F. Romacheva, 1973; J. Haubrich, 1976; G.I. Semenchenko, A.F. Kovalenko , 1982; BC Kolesov, 1987; AM Solntsev et al., 1991, etc.).
In our clinic, based on etiological principles, we use the classification of AM Solntsev et al. (1991), which distinguishes the following types of sialosis:
- endocrine;
- neurogenic;
- related to nutritional disorders (nutritional);
- mixed;
- unknown etiology.
Endocrine sialoses
develop with endocrine diseases, hormonal changes and other disorders (dysfunction of the gonads, diabetes, diffuse toxic goiter, menopause, etc.).
Neurogenic sialosis
occurs with osteochondrosis of the cervical spine, with mental trauma, vegetative neurosis, diencephalic syndrome, etc. Autonomic dysregulation, caused predominantly by the sympathetic part of the autonomic nervous system, plays an important role in pathogenesis.
Alimentary sialoses
are observed with emaciation, diseases of the gastrointestinal tract (hepatitis, cirrhosis of the liver, colitis, pancreatitis, etc.), with irrational fasting, etc.
Mixed sialoses
- with a combination of the previously listed etiological factors.
Sialosis of unknown etiology
- the cause of the disease cannot currently be determined.
In recent years, a new group of sialoses has been identified, which arise under conditions of environmental pollution with fluorides and radionuclides
(V.I. Mitchenok, 1996).
Experimental models of autoimmune, metabolic and neurocircular sialosis have been developed (G. Seifert, 1962; L.D. Chulak, 1983, etc.).
Clinic.
The clinical manifestations of sialosis are similar to each other, regardless of the etiological factors that caused them. They are characterized by recurrent enlargement, more often of the parotid glands, less often of other large salivary glands. Swelling appears more often for no apparent reason. Patients usually associate this with hypothermia, overheating, food intake, colds and other factors. The swelling lasts from several days to several weeks, and then the size of the gland slowly returns to normal.
The frequency of relapses may vary (from once a week to once every six months). The size of the enlarged salivary glands varies: from barely noticeable to pronounced swelling.
In the development of sialosis, BC Kolesov (1987) distinguishes 3 stages: initial (stage of hypersecretion),
clinically pronounced
(stage of exhaustion of secretion and dystrophic changes in the epithelium)
and late
(stage of lipomatosis and fibrosis).
Patients usually turn to a doctor for medical help in the clinically expressed stage of the disease.
On examination, there is facial asymmetry due to unilateral enlargement of the parotid gland or bilateral enlargement of the parotid glands is observed. The swelling is usually painless or slightly painful. The skin color is not changed. The skin is pulled into the fold easily (with slight swelling) and with difficulty (with its final increase). Mouth opening is free. The mucous membrane of the oral cavity is usually less moisturized and may be hyperemic, because. Most patients consult a doctor in the stage of exhaustion of secretion (clinically pronounced stage of sialosis). The mouth of the excretory duct is not changed. When massaging the gland, most subjects release clear saliva from the duct, less often viscous saliva with streaks of mucus or fibrin flakes, and in some cases cloudy saliva. Salivation from the affected gland (or two glands) is reduced. A.F. Kovalenko (1982) revealed a sharp violation of the enzyme-secreting function of the salivary glands.
When performing sialography of the parotid glands, the following changes are revealed: narrowing of small and larger ducts, depletion of the gland parenchyma pattern (Fig. 23.4.1 -23.4.3). The narrowing of all excretory ducts is due to their compression due to hypertrophy and hyperplasia of gland parenchyma cells. But along with this, inflammatory changes are observed in the gland in the form of periductal round cell infiltrates, and in the late stage of sialosis - replacement of gland parenchyma cells with adipose or fibrous tissue with lymph-plasma cell infiltration (BC Kolesov, 1987). The cytological picture of saliva changes (Figure 23.4.4).
Laboratory tests of blood and urine showed no significant changes. With exacerbation of inflammatory phenomena, neutrophilia, acceleration of ESR, etc. are observed.
Rice. 23.4.1.
Appearance of a patient with endocrine sialosis (a). Sialogram of the parotid gland in the phase of filling the parenchyma (b) and the phase of resorption and emptying (c).
Rice. 23.4.1.
(continuation)
Diagnostics
This disease presents certain difficulties due to the variety of etiological factors that cause the development of sialosis. The diagnosis is based on anamnesis, clinical examination of the patient, the results of sialography and sialometry, as well as data from a morphological study of salivary gland biopsies. These patients need to undergo a full examination to identify existing diseases in other organs and systems.
Treatment
In patients with sialosis, treatment should, first of all, be aimed at eliminating the disease that was the cause of the development (etiotropic) of dystrophic changes in the gland (hormonal, neurogenic, etc.). That is, treatment of patients with sialosis should be carried out in collaboration with an endocrinologist, neurologist, gynecologist, therapist or other specialist.
The dentist's treatment is symptomatic and consists of increasing the salivary function of the gland, i.e. aimed at combating xerostomia (dry mouth) and its consequences. To normalize salivation, acupuncture, galvanization and electrophoresis of novocaine (hydrocortisone, iodine, galantamine, etc.) are used on the area of the salivary glands. In our clinic, for many years, to improve the salivary function of the major salivary glands during sialosis, blockades (with anesthetics) of the superior cervical and stellate ganglia of the neck have been used (see description in section 9.2, volume I of this Manual). Salivation returns to normal within 6-8 months, and
then the course of blockades is repeated.
The complex of therapeutic measures includes anti-inflammatory therapy (salol, methenamine, etc.), protease inhibitors (L.D. Chulak, 1983). For sialosis caused by environmental pollution factors (fluorides, radionuclides) V.I. Mitchenok (1996) recommends the use of a complex of medications from vilosen, splenin, potassium orotate, sodium nucleinate, tocopherol acetate and propolis, because These drugs are compatible and mutually potentiate antitoxic, radioprotective, antioxidant and other actions.
Treatment of sialosis is varied, but does not always lead to complete recovery. Therefore, in the late stage of the disease, there may be indications for the use of a surgical treatment method (subtotal or total parotidectomy with preservation of the branches of the facial nerve, extirpation of the parotid gland excretory duct). We recommend surgical treatment only when all other (conservative) methods of therapy do not produce positive results.
It is most difficult to treat patients with mixed forms of sialosis (concomitant diseases mutually aggravate the course of the disease), as well as sialosis of unknown origin.
Rice. 23.4.2
. Appearance of a patient with neurogenic sialosis (a). Sialogram of the parotid gland in the phase of filling the parenchyma (b) and the phase of resorption and emptying (c).
Rice. 23.4.2.
(continuation)
Rice. 23.4.3.
Sialograms of the parotid glands of patients with sialosis (a, b, c, d). There is a narrowing of all excretory ducts. The parenchyma of the gland is not determined.
Rice. 23.4.3.
(continuation).
Rice. 23.4.4. Cytograms of saliva obtained from the parotid gland of patients with sialosis.
Outside the period of exacerbation, squamous epithelial cells with vacuolated
cytoplasm, against the background of detritus, single decaying leukocytes and
squamous epithelial cells (a). In the phase of exacerbation of the clinical course,
neutrophil leukocytes, lymphocytes, squamous epithelial cells without changing them
morphology against the background of detritus and mucus (b).
Treatment of calculous sialadenitis
Calculous sialadenitis of the submandibular salivary gland can be cured with conservative methods. If they are ineffective, surgery will be prescribed.
Treatment includes:
- applying warm compresses;
- rinsing the mouth with antiseptics;
- carrying out baths.
Be sure to follow a salivary diet.
If the stone size is large, the stone is removed surgically. In case of frequent relapse, surgery to remove the gland itself is indicated.
Inflammation of the salivary glands: symptoms, treatment, causes
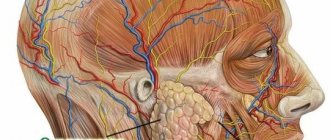
There are not so few salivary glands in humans. Two parotid (one at each ear), two submandibular (on each side under the lower edge of the jaw) and two sublingual. In addition, there are many different small glands in the palate, cheeks, tongue, lips, mucous and submucous of the mouth.
And each of these salivary glands can become inflamed one day, bringing its owner a lot of trouble. This condition will be called sialadenitis. A special case of inflammation of the parotid salivary gland is called mumps. We will talk about inflammation of the salivary glands, symptoms and treatment of sialadenitis below.
Surgery
Surgery for sialadenitis is carried out to remove stones, widen the duct, enucleate the cyst (if there is one) and eliminate purulent complications.
Endoscopic surgery is performed through skin punctures through which an endoscope with a camera is inserted. This method is used to remove the gland and crush the stones. Microsurgical operation allows removal of the pathological focus, preserving the gland and patency of the ducts.
Removal of stone from the submandibular duct is performed under local anesthesia. An incision is made between the hyoid fold and the main tongue. Stones are removed with a surgical spoon or tweezers. After the operation, the wound is not sutured, the patient is prescribed a salivary diet. If the stone is located deep within the gland itself, it is removed along with the stones.
To prevent relapse, you need to maintain oral hygiene, not forgetting to use rinses. A measure to prevent the disease will be regular sanitation at the dentist. It is important to treat infectious diseases until complete recovery, avoid hypothermia, and include more vitamin and salivary foods in the diet.