The essence of the disease
Chronic periodontal disease of an inflammatory nature, which is accompanied by the formation of granulomas at the apex of the tooth root, that is, formations separating the source of infection from the healthy part of the tooth, is called granulomatous periodontitis.
Granulomas arise from periodontal tissues in situations where there is activity of a chronic lesion supported by microflora, and the body is able to build a barrier that isolates it.
With periodontitis, inflammation of the periodontium occurs, that is, the tissue connecting the dental roots and the alveolar plates. Thus, the integrity of the ligaments is compromised, and the tissues around the tooth are gradually affected.
This disease can occur without symptoms and manifest itself only during an exacerbation.
Surgery
Surgical treatment consists of removing the tumor along with part of the apex of the tooth root. It begins with strong anesthesia at the treatment site. The dentist then makes an incision in the gum opposite the root tip. Folds back and secures the gingival flap. Using a dental cutter, a “window” is cut into the jaw bone, commensurate with the source of destruction.
Files down the protruding root part. If necessary, fills the remote part of the dental canal. Scrapes out a cavity formed in the jaw bone. Fills it with a special material, which includes healing and restorative substances. Returns the gum flap to its place and applies self-absorbing sutures.
The removed part of the root along with the granuloma
If the neoplasm has grown to more than a third of the tooth root, or it is severely destroyed, the tooth must be removed.
Have you ever encountered similar phenomena?
If the article was useful to you, please like and share the article with friends who will be interested in this topic.
Clinical characteristics
A disease such as granulomatous periodontitis usually does not manifest itself in any way, and it is most often diagnosed accidentally, when checking the condition of the dental organs using an X-ray. The formation characteristic of this disease is represented by a dense sac, firmly attached at one end to the tooth root. Fistulas do not occur on bone tissue. Sometimes the patient complains of long-standing pain in the tooth, which then completely disappeared.
In this case, the tooth, which usually has a filling or crown, is affected by caries underneath, forming a rather large cavity. The color of the tooth may be unnatural. No pain is felt upon probing. An unpleasant odor emanates from the cavity. With percussion there is most often no pain, or instead there is minor discomfort. There may be slight swelling of the mucous membrane, palpation of which passes without pain. Lymph nodes are usually unchanged.
On a note! Where is the best place to treat periodontitis? Experienced doctors advise doing this in clinics that are equipped with a dental microscope. A high-precision device allows you to carry out any manipulation efficiently, carefully, precisely and sparingly, without the risk of perforation or damage to the walls, without grinding down a large amount of healthy tissue, in the presence of narrow and highly curved root canals. Under a microscope, even teeth can be saved, which in clinics without an optical magnifier are usually ordered to be removed. Read about all the benefits of treatment using this high-tech device in the feature article on the website.
This disease can be definitively diagnosed only as a result of electroodontodiagnosis and radiovisiography.
Main types
Let's consider the types of disease:
- Granuloma. With initial inflammation, the periodontium becomes denser, leading to the proliferation of connective tissue. This formation is continuous due to constant exposure to toxins and cells from the root canal. Thus, as a result of the confrontation between destruction and creation, a cavity formation arises, in which there are granulations, fibrous elements, microbes and their dead remains, cells that are responsible for the body’s immune response.
- Cystogranuloma is a formation arising from an ordinary granuloma. Due to the active development of epithelial cells located in the periodontium, the structure of which resembles the structure of the epithelium of the oral mucosa and their inclusion in the formation of a cyst, an internal mucous lining appears. The site of inflammation acquires an acidic environment, which can reduce the rate of cells involved in the formation of bone tissue (osteoblast) and activate cells that destroy it (osteoclasts). The destruction zone of cystogranuloma is 5-8 millimeters, and sometimes reaches a whole centimeter.
- The cyst is a cavity formation that appears as a result of the fusion of the connective tissue capsule and the internal mucous tissue. Continuous strong pressure arising from the secretion produced by the inner layer is transmitted to the surrounding bone tissue, leading to its destruction. The liquid contents of such a formation are gradually filled with cholesterol crystals, which can be seen when the cyst is opened or flows through the fistula.
Types - stages of development
Granulomatous periodontitis has three types - stages of development. First, a granuloma appears, which we described above. Its diameter usually does not exceed five millimeters. Constant infection from the tooth root leads to the full development of the granulomatous capsule. Granuloma is filled with granulations, fibrous tissue, active and dead microorganisms, and toxins.
This is what a granuloma looks like under a microscope
If at this stage of development a rupture of the protective membrane occurs, then the entire contents of the capsule will enter the periodontal and neighboring tissues. Intense inflammation will begin, which can lead to poisoning of the body and infection of internal organs.
Acute periodontitis
Attacks of granulomatous periodontitis in the acute stage occur due to local inflammation of a small area of the jaw. The appearance of pain is provoked by the body’s reaction to the inflammatory focus. The formation of a serous and purulent mass, and then microabscesses, causing an increase in inflammation, which becomes a prerequisite for purulent cyst formation. The pain in the acute stage of periodontitis is aching, accompanied by discomfort in the gum area. At the same time, eating hot foods becomes significantly painful.
When lying down, the patient feels as if he has an ingrown extra tooth, and the pain increases.
A visual examination of the jaw does not reveal the disease, because it is localized in its internal part.
A dental examination may reveal slight looseness of the tooth. When pressing on it, there is an increase in pain, and the gums also swell slightly.
If the disease is ignored and there is no timely treatment, the disease from the inflammatory process can progress to the stage of purulent formations. In this case, an increase in temperature is observed, the mobility of the dental organ increases, the patient may shiver, the size of the lymph nodes increases, the mucous membrane swells, and pain occurs on palpation.
You can learn more about acute periodontitis here.
Symptoms of granulating periodontitis
Chronic granulating periodontitis is characterized by the following symptoms: aching pain, aggravated by load on the tooth - pressure, chewing, thermal exposure; local swelling and hyperemia of the gingival tissue, gum pastiness; slight tooth mobility is possible; In the projection of the root, an infiltrate can be felt - a fistula with serous or purulent exudate can be formed at this site.
Other, less common symptoms are discoloration of the tooth, enlargement and some pain on palpation of the lymph nodes (submandibular and submental) on the side of the affected tooth. The fistula tract most often opens in the oral cavity from the vestibular side, but can occur on the face and neck, which requires careful differential diagnosis with actinomycosis.
The course of the disease consists of alternating periods of exacerbation and remission; relief most often occurs with the outflow of purulent exudate. The period of remission may be asymptomatic, but there is often slight pain when chewing and exposure to temperature, especially if the affected tooth also has a carious cavity. After a short lull, an exacerbation of granulating periodontitis occurs, followed by the accumulation of pus and an intensification of the inflammatory process.
Chronic periodontitis
This pathology is characterized by the location of granulation tissue near the upper part of the tooth root, surrounded by fibrous capsules. The function of the fibrous capsule is protective, since it does not allow pathological substances to enter the body, leaving pus, toxins, microbes and decay products within its boundaries. Thus, a balance is obtained between purulent inflammation and the entire body. For this reason, the disease does not have pronounced symptoms, whereas it destroys the periosteum and bone tissue.
You can learn more about chronic periodontitis here.
Stages of periodontitis
Healthy gums hold the teeth firmly in the socket. Periodontitis develops in several stages.
- There is bleeding and slight swelling of the gums. Most often, this result is caused by ordinary plaque on the teeth. If it is not removed carefully enough, it turns into tartar and accumulates in the spaces between the teeth. Plaque contains aggressive enzymes and toxins that irritate the gum tissue. Gingivitis begins to appear.
- Dental pockets appear. The cause of their occurrence is hardened plaque on the teeth. The necks of the teeth begin to become exposed at the roots. They become extremely susceptible to any influence of external factors: chemical, physical, mechanical. This is why it is important to see your dentist twice a year. If he detects a stone on your teeth and removes it in a timely manner, this will save you from many diseases.
- If the patient has not received adequate treatment, periodontitis progresses. Bone and connective tissue are severely destroyed. This is a direct path to tooth loss.
Causes
Inflammation of the soft tissues of the dental organ can cause periodontitis. Education is promoted by:
- mechanical damage to the periodontium;
- poor quality dental filling;
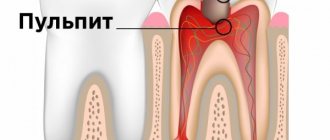
- caries and, as a consequence of its neglect, pulpitis;
- fungus;
- poor-quality treatment of pulp or pathology;
- the presence of endocrine diseases;
- poor absorption of vitamins and minerals;
- bite problems;
- reduced immunity;
- smoking.
In addition, the tooth root can be affected due to the use of certain drugs, as well as allergic reactions with deformation of soft tissues and subsequent infection in the space between the teeth.
In other words, pathogenesis can be provoked by premises in three directions:
- drug complications;
- bacterial damage;
- soft tissue injury.
Causes of granulomatous periodontitis
In most cases, granulomatous periodontitis is part of the structure of pathologies of chronic etiology. The disease in question is a sluggish dental disease that periodically worsens and over time can lead to tooth loss.
The proliferation of granulomatous periodontitis is caused by the presence of pathological changes in the human body, conditionally divided into pathogenetic and external development factors.
Pathogenetic factors:
- Carious lesion.
- Pulpitis.
- Granulating periodontitis.
- Incorrect dosage of medications.
- Abnormal microflora of the oral cavity.
- Immune deficiency.
- Hypovitaminosis.
- Chronic diseases.
- Dysfunction of the endocrine system.
- Allergic reactions to drugs used in dental treatment.
- Weakened immunity due to surgical interventions.
In the pathogenesis of granulomatous periodontitis, in addition to pathogenetic factors and mechanical causes, there are deviations in the development of the dental system:
- orthognathic bite;
- anomalies in the structure of teeth;
- anomalies of the dentition.
Granulomatous periodontitis is diagnosed more often if the above abnormalities are present.
External development factors:
- Facial injuries.
- Smoking and chewing tobacco.
- Poor quality dental treatment.
- Traumatization of the gums.
- Chronic and occupational injuries.
- Use of aggressive chemicals.
- Attempts to chew hard foods or objects.
The main reason for the development of chronic granulomatous periodontitis is constant focal infectious processes in the dental tissues.
Symptoms
Most often, a granuloma grows and forms without showing any symptoms. And the rate of its growth depends on the state of the patient’s immunity and how active the inflammatory process is.
But still, some patients with granulomatous periodontitis experience discomfort in the area of the diseased dental organ when they eat. At the same time, the tooth may also change color or the filling may fall out.
During the period of exacerbation, as well as during the time when the cystic form is already observed, symptoms that accompany acute periodontitis usually appear. If the cyst is not located directly at the root apex, but is slightly shifted to the side, swelling may occur upon palpation.
Symptoms of granulomatous periodontitis
Granulomatous periodontitis often has a latent nature of manifestations. Granuloma forms and grows without clinical manifestations. The symptom complex and complaints of patients arise with the progression or exacerbation of the pathological process.
The manifestations of the pathology in question are similar to the symptom complex of acute periodontitis. The primary symptom of granulomatous periodontitis is discomfort and unpleasant sensations around the tooth, burdened by a pathological deviation.
The main symptoms of periodontitis:
- Radiating toothache.
- Proliferation of infiltrate on the gum.
- Swelling of the cheeks and, in rare cases, lips.
- Tooth mobility.
- Change in the normal size of the submandibular lymph nodes.
- Increase in body temperature to subfebrile levels.
- Sour breath.
- Hypersalivation.
- Formation of fistulas on the gums and facial skin.
- Change in enamel color on a tooth burdened with granulomatous periodontitis.
- Loss of material used to fill the dental cavity after treatment.
Symptoms of granulomatous periodontitis are accompanied by an explicit pain syndrome, since the infectious process involves the tooth and the regional bone tissue of the apex of the tooth root.
There is a slow decay of nerve endings and damage to the ligamentous apparatus. It is necessary to seek qualified help from a dental center.
Diagnostics
Diagnosing a disease can be both simple and difficult at the same time. The difficulty lies in the absence of symptoms, which is why the diseased tooth may not be noticed at all. If there is a change in color, the presence of a significant defect, the absence of pain on probing and the presence of other symptoms of periodontitis in the chronic stage, it is not difficult to recognize the occurrence of a granuloma. But if they are absent, then the development of this disease is unlikely to be suspected. In this case, the inflammation can gradually turn into a cyst.
The disease is often determined only by radiography of the root of the tooth. The image shows that there is destruction of the bone tissue and deformation of the root.
The lesion is usually circular in shape and looks like a cyst. It can touch the root, or form a kind of cap. The edges of the bone tissue are blurred and jagged. The more the disease progressed, the fewer areas there were where there was no bone structure with smooth contours.
To distinguish this disease from other oral diseases, you need to know the following:
- with average caries and chronic pulpitis, no abnormalities will be detected on x-rays;
- fibrous periodontitis is characterized by an enlarged periodontal fissure;
- as with pulp necrosis, the sensitivity of the dental organ affected by granulomatous periodontitis also falls within the range of 100 to 120 μA;
- a root cyst is accompanied by discrepancy of teeth and bulging of the bone wall;
- symptom of “parchment crunch”.
Active cell proliferation
Lack of treatment leads to the formation of cystogranuloma, the size of which varies from five to eight millimeters to a centimeter.
The cells of the upper layer of periodontium are similar in structure to the upper layer of the mucous membrane. Their active reproduction leads to the formation of a mucous lining inside the granuloma, turning it into cystogranuloma. These changes increase the level of acidity at the site of inflammation. The higher the acidic environment, the slower the formation and the faster the destruction of bone tissue.
Treatment
The main task of treating granulating periodontitis is to eliminate the source of chronic infection. In this case, endodontic treatment is carried out. And only if it does not produce results, you can resort to one of the surgical methods: resection of the apex of the tooth root, its hemisection or coronary-radicular separation. The doctor decides how the treatment will be carried out regarding the structure and size of the granuloma, the patency of the tooth canals, the age of the patient, the presence of other diseases and the state of immunity.
To cure a small granuloma with a small amount of epithelium and good patency of the canals, conservative therapeutic treatment is used. It is as follows:
- Introduction into the enlarged and treated dental canals of a drug that leads to the death of pathogenic bacteria due to its high acidity, which contributes to the resumption of osteoblast activity.
- With the help of calcium hydroxide, the bone structure is restored and strengthened.
- Iodoform increases the bactericidal properties of the drug.
If the granuloma is large, it will most likely be necessary to resect the apex of the tooth root. But at the same time, almost half of the apex will be removed, and it happens that it would be more advisable to remove the entire tooth.
Let us consider the procedure for resection of the root apex step by step:
- Infiltration anesthesia.
- An incision is made in the projection of the apical zone, the gingival flap is folded back and held with sutures or an instrument so that the entire surgical field is visible.
- Sawing out a bone window relative to the area of destruction using a cutter.
- Cutting down the protruding part of the root and placing filling material in the distal part of the canal, if necessary.
- Scraping the bone cavity and filling it with a material that accelerates the regeneration of bone tissue.
This method of treatment gives good results, but it is used only in cases where conservative treatment is ineffective.
When treating this disease in the acute stage, the symptoms of acute inflammation are first relieved by ensuring the drainage of pus and prescribing antibacterial therapy, and then treatment is carried out according to a standard template.
Treatment methods
Granulating periodontitis is treated surgically (operative) or therapeutically (endodontic) by:
- Chronic stage. Therapeutic measures consist of the following actions: removing exudate from the inflamed area; elimination of the infected inflamed part - the canal is cleared of infected dentin and decayed pulp; destruction of pathogenic flora with anti-inflammatory and antimicrobial pastes, which are placed in the tooth root, antiseptics; if necessary, use broad-spectrum antibiotics, sulfonamides, ultrasound (physiotherapy); carry out measures that ensure the restoration of periapical tissues and bone structures; canal filling. If necessary, surgical intervention is performed.
- Remission. Anti-inflammatory local agents of complex action and physiotherapy are used. Vitamins (mainly groups B and C), as well as biogenic stimulants, are prescribed.
- Exacerbation of chronic granulating periodontitis. Pain is relieved and treated as for a chronic disease.
- Surgery. The teeth are removed with severe destruction of part of the crown; with great mobility (stages 3-4); if the canal cannot be opened due to curvature, obstruction of the lumen or narrowing. Preference is given to operations that allow the patient to save the tooth. These include: amputation - the affected root is removed before it becomes the crown; cystotomy – the cyst is partially removed; hemisection – the root of a multi-rooted tooth is cut off along with the crown; cystectomy – complete removal of the cyst; resection of the root apex – removal of the area of inflammation and infection.
Treatment through surgery
Surgical intervention, that is, removal of a dental organ, can be performed if conservative therapy is ineffective.
The following factors contribute to removal:
- mobility of the third, fourth and fifth degrees;
- severe destruction of the tooth crown and the inability to regenerate it;
- the presence of severe educational pathologies or the patient’s mentally unstable condition.
After the tooth is removed, its hole is well treated with antiseptics and antibacterial drugs, and the patient is also prescribed antibiotics that will completely destroy the infection.
Surgical intervention is also possible when the integrity of the tooth is preserved. These may be the following procedures:
- removal of the upper part of the tooth root;
- removal of part of the tooth root that is affected;
- partial root amputation;
- implantation of the missing area of the tooth;
- transplantation.
Disease prevention
If conservative therapy was carried out correctly, a transition from granulomatous periodontitis to fibrous periodontitis occurs. After this, treatment is no longer required. At first, the patient may feel pressure and discomfort in the gums, which is a completely adequate reaction of the body and will soon pass.
If surgery has been performed, pain may persist for the first time at the incision sites. If sharp pain appears, it is important to see a dentist immediately, as it may indicate that the operation was performed incorrectly.
Important to know: After surgery, it is important for the patient to avoid alcohol, nicotine, hot and spicy foods. Chewing food must be done so that the edges of the wound are not touched.
After six months, it is important to see the dentist again, who will take a control x-ray.
If the disease is not treated, it can lead to unpleasant consequences. The granuloma will develop into a large cyst that can envelop the roots of nearby teeth. The bone tissue will gradually deteriorate. These consequences will lead to the need to remove the dental organ.
If treatment is started in time, then when the granuloma suppurates, the acute inflammatory process will be stopped and conservative or surgical treatment will be carried out.
In order to detect the disease in time, it is important to visit the dentist once every six months, take a picture of the jaw bones and, if necessary, treat all inflammations of the oral cavity.
It is also important to carry out high-quality oral hygiene and be attentive to all changes in the sensitivity of the dental organs and prevent damage to soft tissues. If teeth are damaged by caries, it also needs to be treated immediately.
If you follow all of the above recommendations, granulomatous periodontitis will be prevented.
Treatment of the disease
Treatment of periodontitis, be it acute or chronic, is always carried out in a complex manner. But in the second case, the therapy is longer.
To treat chronic periodontitis, innovative clinics use a dental microscope, which provides clear visualization of the anatomy of the root canals. The device allows you to perform tooth-preserving surgery at a high level and relieve the patient from the need to remove a neglected tooth. Thanks to the microscope, it is possible to avoid the risks that usually arise during the treatment of periodontitis: removal of material beyond the apex of the tooth root, underfilling of the canals, incomplete removal of affected tissue, perforation of the root walls.
Outflow of pus
The doctor opens the dental canals to ensure unhindered drainage of purulent discharge. There are situations when root canals have a curved shape. Then the doctor makes an incision on the side, from the gum side, installing a drainage - a thin tube through which the pus comes out. The same manipulations are carried out if pus is in the periosteal space. Such therapy takes from a day to several days.
Outflow of pus
Laying the medicine
Afterwards, the channels are thoroughly washed with an antiseptic. A drug is placed inside the tooth cavity or under the gum, the action of which is aimed at suppressing pathogenic microflora and restoring damaged tissue. A temporary filling is installed. The duration of this stage is 3 or more days. If necessary, the drug can be replaced several times.
Laying the medicine
Drug therapy
It is carried out simultaneously with other procedures, from the very first stage of treatment. Antibiotics and antihistamines are prescribed, which prevent the proliferation of bacteria and eliminate them, stopping inflammatory processes.
Antibiotics
Gum curettage
This procedure, which is aimed at peeling the gums and removing plaque and stone from the surface of the tooth roots, is required if the cause of periodontitis is deep deposits.
Gum curettage
Video of closed gum curettage
Final filling
The completion is the filling of the canals and the outer part of the tooth, and, if necessary, the installation of a crown. But only after an x-ray is taken, the image will show whether the inflammatory process has completely stopped.
Treatment of periodontitis
If treatment of aggravated chronic periodontitis is started on time and carried out efficiently, there is a possibility that this disease will no longer remind of itself. But it is worth remembering that if tooth mobility and bone resorption around the root have appeared, the tooth cannot always be saved - it is easier to remove it and replace it with a dental implant than to carry out long-term and expensive treatment, which may be completely ineffective.
Notice
: Undefined variable: post_id in
/home/c/ch75405/public_html/wp-content/themes/UltraSmile/single-item.php
on line
45 Notice
: Undefined variable: full in
/home/c/ch75405/public_html/wp-content /themes/UltraSmile/single-item.php
on line
46
Rate this article:
periodontitis