Occurring most often as a result of the development of caries, periodontitis in children is, unfortunately, very common. It is no exaggeration that inflammation of periodontal tissue occurs in almost every third child. Caries is not the only reason that leads to periodontitis, but it can be called one of the most common. It is strictly not recommended to delay a visit to the dentist, since the consequences of this disease in children can be much more serious than in the case of adult patients.
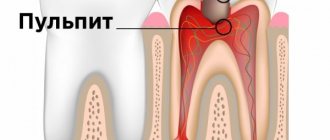
What is periodontitis?
Periodontitis is a severe inflammation of the soft tissues adjacent to the tooth root. This fact alone explains the need for an early visit to the dentist, because the source of inflammation turns out to be located dangerously close to the human brain and his respiratory tract. Periodontitis in children is distinguished by the presence of its rather specific features, in particular, children's teeth are still at the stage of their development, molars are still forming and are in their rudimentary state. As a result, periodontitis begins to develop rapidly, flowing, among other things, into a purulent form; in addition, the process of its treatment becomes more and more complex and difficult over time.
Symptoms of acute periodontitis in children may include lymphadenitis, abscesses and phlegmon, occurring against the background of the appearance of an inflammatory process in the soft tissues and the occurrence of swelling. The consequence is a deterioration in the child’s health; he experiences an increase in temperature and the number of leukocytes in the blood, as well as sedimentation of red blood cells in it. Periodontitis in children in its purulent form can provoke acute sepsis and osteomyelitis; moreover, it is worth remembering that the chronic stage of this disease is fraught, although this happens quite rarely, not only with granulomatosis, but also with the threat of fibrosis of adjacent tissues. The worst thing is that the inflammation is not limited to a certain framework; it very quickly begins to cover adjacent areas of soft tissue, negatively affecting the future molar of a person.
Acute periodontitis of milk teeth
The treatment plan is selected individually by the doctor. If there is a suspicion that there is a risk of inflammation of the permanent tooth germ, then the baby tooth can be removed. The same is done when the tooth root is destroyed by 2/3 or more, when periodontitis of permanent teeth is treated.
The desire to minimize the number of visits to the dentist and to carry out treatment at one time is a normal desire of both parents and young patients themselves. This is entirely possible under certain circumstances. In this case, modern anesthetic drugs are used to ensure painless treatment, without causing discomfort to the child and reducing stress from the procedures.
Treatment in one day can be divided into 3 stages:
- Preparation of a diseased tooth.
- Removal of affected tissues from the cavity of the coronal part of the tooth and canals.
- Filling.
If it is impossible to treat periodontitis in one visit, after opening and cleaning the tooth, a course of drug treatment is prescribed. Medications are prescribed for a certain period of time, determined by the doctor. Afterwards they are removed and the tooth is filled.
All details, as well as the need for subsequent treatment, are determined by the doctor.
The periodontium in children is loose, and the connective tissue that forms it is not as dense as in adults. It contains many blood vessels, which makes the tooth structure susceptible to pathogenic bacteria. Periodontal instability is associated with subsequent resorption of dental ligaments due to the replacement of milk teeth with permanent ones. The main factors for the development of periodontitis in children are:
- injury to dental structures;
- improper treatment of caries or pulpitis;
- some medications used for treatment;
- decreased immunity due to persistent viral infections (influenza, acute respiratory viral infections, chronic inflammatory processes of the ENT organs).
Most often, inflammation is caused by microorganisms such as streptococci, staphylococci, lactobacilli, yeast-like fungi, and actinomycetes.
How does periodontitis manifest in a child?
The disease occurs in acute and chronic forms. Symptoms:
- hyperthermia (up to 38-39 degrees);
- general deterioration of the condition – lethargy, unnatural drowsiness, moodiness;
- sleep disturbance;
- loss of appetite or refusal to eat due to severe tooth pain;
- throbbing pain in the affected tissues;
- swelling and swelling of the gums;
- swollen lymph nodes;
- unpleasant smell.
In some cases, a fistula may form on the gum, through which pus comes out. In the chronic course of periodontitis in children, stable moderate hyperthermia (up to 37.5 degrees), mild pain, and a consistently increased level of leukocytes in the blood are observed. In some cases, if there is no exacerbation, periodontitis does not have pronounced symptoms.
In a child, chronic granulating periodontitis develops only when the roots are fully formed in children. If baby teeth or roots are not fully formed, granulating periodontitis may develop, which, if not treated urgently, can lead to:
- Rapid resorption of rhizomes of baby teeth;
- Complete tooth death is still in its infancy;
- Development of extensive inflammation
- The occurrence of follicular cysts, periostitis, osteomyelitis against the background of tissue necrosis;
- Premature eruption of baby teeth;
- Development of rheumatoid arthritis, endocardium with the addition of sepsis against the background of periodontal inflammation.
The most common causes are infection coming from the pulp cavity and root canals, trauma and medications (arsenic, phenol, formalin) used in the treatment of pulpitis. Acute periodontitis of primary teeth is rare. They develop as a result of pulpitis, accompanying acute general serous and purulent pulpitis.
The clinical picture is characterized by the rapid spread of inflammatory phenomena, the transition of serous exudate to purulent and the onset of intoxication of the body. With acute periodontitis, children complain of weakness, headache, and increased body temperature. Acute periodontitis is often accompanied by soft tissue swelling, acute serous periostitis, and enlarged submandibular lymph nodes.
However, along with this, purulent exudate in most cases spreads along the periodontal fissure and exits under the gum, forming a subgingival abscess. There are no changes on the x-ray. If the described clinical picture reveals changes in the periodontium, the disease should be considered as an exacerbation of chronic periodontitis.
Treatment depends on the nature and extent of the inflammatory process and the general condition of the child’s body. In case of severe intoxication of the body or the threat of spread of the inflammatory process to adjacent milk teeth (the beginnings of permanent teeth), the diseased tooth must be removed at any age.
In cases of purulent periostitis or subgingival abscess, an incision or blunt detachment of the gums is recommended. The released purulent exudate indicates the possibility of further outflow and eliminates the need to resort to a drill during the same visit to remove the filling or open the pulp cavity.
We suggest you read: At what age do children have their teeth brushed?
In cases where the inflammatory process is localized within the periodontium, opening the pulp cavity and removing the root pulp from all canals, ensuring the outflow of exudate through the root canals of the tooth, is indicated. The tooth is left open for 7-10 days, after which chronic periodontitis is treated.
If acute periodontitis accompanies general pulpitis of a baby tooth, then first of all the inflammation of the pulp should be eliminated. It is contraindicated to resort to pulp devitalization with arsenic preparations during the same visit. Inflammation can be eliminated with camphor-phenol and anesthesin. The child is prescribed analgin, 6-10% calcium chloride in a teaspoon or tablespoon 2 times a day, white streptocide 0.1-0.5 g 2-3 times a day, chlortetracycline (biomycin) 100,000 units 2 times a day.
https://www.youtube.com/watch?v=r0pTGF-R5Ys
The main reasons are the same as in adults. The process can develop from acute inflammation and primarily. Very often, chronic periodontitis is found in the area of teeth treated for pulpitis. The same forms of chronic inflammation occur as in permanent teeth, but chronic granulating periodontitis predominates.
The anatomical proximity of the roots of primary teeth to the rudiments of permanent teeth makes it possible for the pathological process to spread to permanent teeth. As a result, the full formation of the tissues of the crowns of a permanent tooth may be disrupted; formation of follicular cysts; displacement of the rudiments of permanent teeth followed by abnormal eruption of the latter; premature eruption of permanent teeth, etc.
Chronic periodontitis is often asymptomatic. The most common sign of chronic granulating periodontitis is a fistulous tract, which is also found with filled teeth. In untreated teeth, there may be no visible connection between the carious cavity and the pulp. If the tooth was once treated, but the treatment was not completed and the pulp cavity remained open, then granulation tissue may be found in the cavity, growing from the periodontium through the root canals or through perforation in the area of root bifurcation.
Single-rooted primary teeth with granulations that have grown into the canal are treated in one visit. The granulations are burned with phenol and anesthesin and, despite bleeding from the canal, they are filled with eugenol paste (it is not recommended to add thymol to the paste), Genis paste, etc. In multi-rooted teeth, chronic periodontitis, accompanied by the germination of granulation tissue into the root canals, is treated using mummifying agents .
On the first visit, the carious and pulp cavities are opened, a phenol-formalin mixture (1 drop of 40% formalin solution and 2 drops of phenol) is left over the orifices, and a bandage is applied. On the second visit, the contents are removed from the canals, the formalin-resorcinol method is used, and a bandage is applied. On the third visit, the accessible part of the canals is filled with formalin-resorcinol paste and the tooth is filled.
Chronic periodontitis with the presence of decay and purulent contents in the root canals is treated with the use of proteolytic enzymes. On the first visit, the pulp cavity is opened, decay is removed if possible, a tampon with a solution of proteolytic enzymes and antibiotics is left over the orifices, and a bandage is applied;
Causes
Infectious lesions that occur when affected by caries and its complex forms become one of the most common causes of childhood periodontitis. The peculiarity of the structure of a child’s tissues, which consists in their loose structure, allows infectious processes to develop at a high speed due to the large number of vessels. Childhood periodontitis can also be caused by other reasons, for example, trauma, this is especially true of teeth located in the front. Injuries received as a result of falls or sports provoke the death of the pulp and contribute to the transition of the disease to a chronic condition.
It is advisable to note other reasons contributing to this disease:
- the child taking strong medications;
- damage to the body by viral infections;
- carrying out the treatment procedure at a low quality level;
- a consequence of a cold;
- the general level of the child’s body condition.
Reasons for development
Surely every parent who is concerned about the health of their child is interested in the question of what can cause the disease, what preventive actions will help avoid the development of periodontitis.
The main advice that can be given is do not forget to visit the dentist in a timely manner, and at the first signs of caries, do not delay, start treatment. It is untimely or incompletely cured caries that leads to the occurrence of periodontitis. This is due to the structural features of periodontal tissue in children. They are loose, with a large number of blood vessels, and these are very favorable conditions for the rapid spread of infection.
Treatment of pulpitis should not be taken lightly. When treating this disease in children, it is important that the doctor takes into account the patient’s age and correctly selects medications and their dosage. An allergic reaction is unacceptable.
You should pay attention to the baby's daily life. It must be taken into account that young teeth cannot yet withstand large mechanical loads. Therefore, the use of solid foods in a child’s diet must be approached with caution.
You also need to immediately wean your little person from the habit of gnawing hard objects (nuts, pencils, pens, etc.). It is necessary to prevent injuries to the maxillofacial area. Young teeth must be protected.
Another piece of advice is to be attentive to viral diseases, even those that, at first glance, have nothing to do with the oral cavity. Periodontitis in a child can be a consequence of previous infections.
The disease develops as a complication (exacerbation) of caries in the absence of timely treatment, leading to infectious damage to part of the periodontium. But the reasons for the development of the chronic form can be not only in the lack of timely sanitation of the oral cavity and oral hygiene, but also in:
- Incorrect approach of the doctor to the treatment of caries;
- Pathological changes in the root that can lead to the development of inflammation;
- Incorrect selection of medications by the dentist when treating caries in children;
- Failure of women to consult a doctor in a timely manner during pregnancy for treatment of carious teeth;
- Taking certain toxic substances that lead to inflammation of the tissue;
- Treating the canals with chemical compounds that eventually corrode the internal cavity;
- Excessive sensitivity of fragile primary teeth in children to antibiotics, antiseptics or sulfonamides applied by a doctor during the treatment of caries;
- Accidental injury to the canals of baby teeth in the event of mechanical processing or grinding with a drill;
- A case of surgical or dental intervention by a doctor to correct a bite;
- Inaccurate, poor-quality placement of a temporary filling due to excessive mechanical pressure on the tooth;
- A case of jaw injury due to strong mechanical impact, leading to damage to the tooth root.
As a result, an inflammatory process develops in the periodontal area as a complication. The photos provided clearly show what the disease of primary and permanent teeth looks like in the acute stage or when an exacerbation occurs.
Indications for removal of baby teeth
Each case of potential removal of a baby tooth should be considered individually, but there are several indications for mandatory removal, since this is associated with a danger to the child’s health. These include the following:
- zero effect of treatment of the disease and continued deterioration of health;
- baby teeth play the role of a provoking cause of sepsis;
- there is a danger of losing the permanent tooth germ as a consequence of ongoing inflammation;
- dental damage due to chronic inflammation that cannot be treated;
- loose teeth;
- eruption of a permanent tooth against the background of still existing milk teeth;
- chronic periodontitis, which has led to damage to temporary teeth, until the replacement of which there is no more than 18 months.
How to treat
Treatment tactics are selected by the doctor taking into account the classification, degree, severity of damage to the periodontal area, some characteristics of the child’s body, and the type of teeth (baby or permanent).
Granulating acute periodontitis must be urgently eliminated and treated to avoid the development of serious complications. It is possible to carry out complex therapy to eliminate periodontitis with antibiotics with additional vitamins to maintain children's weak immunity.
The process is not complete without the dentist’s manipulations, usually carried out under anesthesia for the purpose of pain relief to provide free access to the tooth, high-quality and complete sanitation of the inflamed area, treatment with antiseptics and antibiotics, and then installation of a temporary filling.
Milk teeth are removed only in extreme cases, when:
- An incorrect bite led to protrusion (crawlout) of a molar beyond the boundaries of the jaw arch;
- The root of a temporary tooth is very loose, excessively mobile and cannot be restored.
- Treatment of permanent teeth directly depends on the degree of root maturity. If there are several roots on one tooth, each root is examined and treated by a doctor separately.
- Treatment of periodontitis in children, both temporary (baby) and permanent teeth, consists of:
- Steaming the pulp cavity;
- Treating areas of inflammation with antiseptics;
- Removal of affected periodontal tissues;
- Eradication of purulent contents from the root canals if granulating periodontitis develops;
- Sealing, placing a temporary filling by placing antibiotics, enzymatic preparations into the cavity;
- Placing a filling in the presence of permanent teeth, for which you need to contact the doctor again at the appointed time.
For a chronic disease, the doctor selects treatment tactics on an individual basis. When treating chronic periodontitis, each case is considered separately. Alternative treatment options are possible, taking into account the child’s age, readiness (unreadiness) for the procedure, the presence of other internal diseases, and the wishes of the parents.
Surgical intervention cannot be avoided in case of complications, infection spreading deep into the tooth canal, development of osteomyelitis, sepsis. It is possible that conservative treatment has already been carried out previously, but did not lead to positive results. The tooth has become very loose since eruption and cannot be preserved.
We suggest you read: Dark plaque on a child’s front teeth
Periodontitis in children - classification
There are several variations in the classification of periodontitis in children, so, according to the causes of the disease, it can be divided into:
- Infectious. It occurs as a result of tooth damage by caries and the penetration of pathogenic bacteria into the periodontium.
- Medication. Becomes a consequence of exceeding the dose of medications.
- Traumatic. Occurs as a result of injury to a tooth or bone tissue.
There is another approach to this issue, based on the type of inflammatory process:
- acute form of the disease, characterized by a high rate of development;
- a chronic form of the disease, during which periodontitis in children can overflow granulation or fibrous tissue, and also degenerate into granulomatous tissue with the concomitant formation of a purulent radicular cyst.
If we focus on the place where the inflammatory focus is located, then the disease can be classified as:
- marginal periodontitis, when the area of its occurrence becomes the area near the neck of the tooth affected by the disease;
- apical periodontitis, when the area of the apex of the tooth root becomes the focus.
At the end of treatment
Timely, high-quality treatment allows you to quickly cope with the disease, return the condition of the teeth to normal, and improve the overall health of the little patient. To prevent recurrence of the disease, you should teach your child how to properly perform oral hygiene procedures and explain the need for a responsible approach to this.
Proper lifestyle is also important: nutrition, physical activity, fresh air, sleep, etc. It is imperative to regularly show the child to the doctor for a preventive examination. At the first complaint of pain or discomfort, you should also not delay visiting the dentist.
Symptoms
The symptoms of the disease will largely depend on the form of its course, for example, purulent periodontitis is characterized by:
- Manifestation of acute pain in the initial period of the disease. Painful sensations are characterized by increasing strength, are constant and tend to intensify, which manifests itself when pressing on the tooth, chewing on the problem side or tapping on it.
- The appearance of swelling of the gums around the diseased baby tooth. The child experiences an increase in temperature, the urge to vomit, and general lethargy. In the blood, ESR accelerates and leukocytosis is determined.
- Enlarged lymph nodes, their pain.
In the chronic form of the disease, without an exacerbating form, symptoms may not manifest themselves, pain may occur upon contact with cold or hot food, and may be intermittent. When a mechanical effect is applied to the tooth, the pain intensifies, but the gums do not undergo changes. Periodically, exacerbations similar to the acute form of the disease may occur, as well as symptoms such as drowsiness, lethargy, increased fatigue and general weakness.
Prevention
The key to success will be regular visits to the dentist for preventive examinations. If caries is detected during such an examination, the treatment will be timely and effective. Parents should be concerned about combating bad habits, as well as protecting the child from injury; in case of any injury to the oral cavity, they must immediately visit a dentist to conduct an examination and determine the consequences. Regarding specialists, it should be noted that on their part, disease prevention is based on a competent procedure for treating caries using medications in the correct dosage and optimally selected methods to combat it.
Diagnostics
Diagnosis of periodontitis in children compared to adult patients is complicated by the fact that a child can rarely accurately explain the symptoms of the disease. Meanwhile, correct diagnosis is the key to successful treatment, therefore, this issue needs to be given increased attention. If there is any doubt about the accuracy of the preliminary diagnosis, an x-ray examination should be performed to obtain the most reliable information.
Rules for diagnosis and treatment in children
When diagnosing periodontitis in a child, the dentist often faces certain difficulties. A child cannot always correctly and accurately describe his feelings, and communication with a dentist is not easy for many children, as they are simply afraid of him.
When examining a small patient, an X-ray examination of a baby tooth and probing may be prescribed. These techniques help the doctor differentiate the development of periodontitis in children from pulpitis and caries in order to develop the correct treatment strategy (we recommend reading: caries in children under 3 years of age: causes and methods of treatment).
READ ALSO: tooth pulpitis: what is it, how is it treated in children?
Treatment of baby teeth
When treating periodontitis in primary teeth, the doctor must first assess how justified the attempts to save the tooth will be, how severely the inflammatory process has affected the tissue, and what risks will arise during extraction.
The dentist always tries to choose the least traumatic method of treating a small patient, however, there are situations when conservative treatment of periodontitis in primary teeth seems impossible. This therapy is not practiced in the following cases:
- the temporary tooth has become very mobile,
- reduced immunity of the child, including due to chronic illness,
- the affected element is the focus of sepsis,
- perforation of the bottom of the cavity of a baby tooth,
- significant resorption of the baby tooth root,
- several periods of exacerbation in the treatment of chronic periodontitis,
- diseases of internal organs, chronic infectious diseases, a history of allergies in a child,
- no more than 18 months before replacing a temporary tooth with a permanent one.
Methods for eliminating periodontitis in permanent teeth
When treating periodontitis in permanent teeth, the dentist tries to avoid unnecessary extractions. The tooth will be removed if therapeutic methods of treatment do not give the required result, and the source of inflammation progresses, and there is a risk of developing serious complications. There are effective surgical treatment methods. The dentist will select the appropriate method of therapy after diagnosis.
The main stages of eliminating periodontitis without surgery:
- cleaning and antiseptication of root canals,
- removal of dead tissue,
- antibacterial treatment,
- restoration of damaged periodontal tissue (in chronic disease),
- sometimes magnetic therapy, UHF, laser therapy are used,
- local use of antibiotics (for deep periodontal pockets),
- filling root canals with filling material.
What to do during an exacerbation?
Chronic granulating periodontitis in children becomes possible in the process of complete formation of tooth roots. The danger here lies in the fact that if urgent treatment is not carried out, the consequences of such inaction will be:
- resorption of the rhizome of a baby tooth;
- death of a tooth at the stage of its formation;
- development of a general inflammatory process;
- the occurrence of complications in the form of follicular cysts, periostitis and osteomyelitis against the background of tissue necrosis;
- eruption of baby teeth ahead of schedule;
- against the background of periodontal inflammation, the development of endocardium and rheumatoid arthritis.
Classification and types
The classification of periodontitis includes several types with distinctive features depending on:
- places of localization of the source of inflammation: in the root apex, cervical canal or in periodontal fibers;
- forms of inflammation: acute and chronic. The acute form begins with pronounced clinical symptoms in the child, although changes in the periodontal part usually do not occur. All types of periodontitis (classification) can be seen in the photo.
Chronic periodontitis, as a rule, passes from an acute form due to untreated pulpitis or caries. Clinically, the picture of the chronic form of the disease in a child is blurred. Symptoms are minor or absent altogether. One thing is obvious - advanced, deep caries, requiring urgent treatment. If the disease is not treated, exacerbation of a chronic illness is inevitable.
Classification by flow includes:
- Granulomatous;
- Granulating periodontitis in the case of rapid spread of the inflammatory process, damage to nearby healthy areas up to the cerebral cortex.
Granulating periodontitis does not present any particular difficulties in diagnosing for doctors. The dental canal is inflamed, painful on palpation, the lymph nodes are clearly enlarged, a blood test shows rapid sedimentation of erythrocytes. The symptoms are obvious, so doctors quickly make the correct diagnosis. The most difficult to recognize are blurred signs with a sluggish course, so chronic granulating periodontitis in a child is diagnosed only by X-ray, or when an exacerbation occurs.
Treatment of the disease
In order to confirm the results of the examination carried out by a specialist and to finally determine the seriousness and extent of the disease, it is necessary to perform an x-ray examination. When the degree of damage to a baby tooth becomes clear, a decision is made about its safety and the advisability of fighting for it. If a child has tooth root damage, severe tooth loosening, or is approaching the time of replacing primary molars with permanent teeth, the dentist may recommend an extraction procedure.
The treatment process is directly related to the scale of inflammation and the general condition of the child; if intoxication is observed, especially in acute form, removal should be carried out immediately, without paying attention to the age of the child.
If a decision is made to leave a tooth, then the issue of correct selection of filling material becomes relevant. Considering that we are talking about a child, the best option would be to use a special paste, which will subsequently dissolve without any harm to him. If it concerns a molar, then you can use resorcinol-formalin paste, the distinctive ability of which is to penetrate into all the curvatures of the dental canals.
The treatment process for childhood periodontitis in acute form is no different from that in adult patients, but it is necessary to take into account the factor of using your own medications and products during the procedure. If we are talking about purulent periostitis, then the primary task is to ensure the outflow of harmful secretions, which will require cutting the gum and leaving the tooth in this condition for up to ten days. If swelling of the facial tissues is detected, a Dubrovin bandage is applied. Therapy involves keeping the child in bed and taking medications in pediatric dosages. If there is no improvement, the question is raised about the need to remove the tooth.
If the therapeutic treatment brings results, then the subsequent procedures are similar to the chronic form of the disease, in particular, it will be necessary to remove decay products from the problem area, perform appropriate antiseptic treatment and perform filling.