Glossitis is a disease of tongue tissue of inflammatory origin.
The main symptoms of the disease are swelling of the tongue, changes in its color, structure, pain, burning sensation in the mouth. All these sensations significantly affect the patient’s quality of life, as it becomes difficult for him to eat and talk. With complications, abscesses and phlegmon of the neck can form. With chronic glossitis, various growths may form on the tongue.
Glossitis can be caused by viruses or bacteria. Glossitis often appears as one of the manifestations of stomatitis or may accompany it. The disease is usually preceded by glossalgia - a general inflammation of the oral cavity, often of an infectious nature.
Causes of glossitis
Glossitis can appear as an independent disease or as a symptom of certain pathologies.
So, the onset of glossitis symptoms is usually preceded by one of the following situations:
- Mechanical damage to the oral cavity or tongue. For example, the cause of the development of glossitis can be a fish or meat bone, sharp edges of damaged teeth, dentures, and so on;
- Chemical exposure: most often this is the use of aggressive oral hygiene products or substances of other origin;
- A burn of the mucous membrane, which occurs either as a result of a single case of severe intensity, or regular exposure to hot food or drinks. Thus, smokers often suffer from this disease, since hot smoke constantly damages the lining of the oral cavity. At first it is difficult to notice the progress of this process, and over time a person gets used to the high temperatures from smoking each cigarette. Also, lovers of strong alcoholic drinks may sooner or later discover glossitis. Irritation of the mucous membrane can also be caused by too spicy foods. As a result of such aggressive influences, the integrity of tissues is disrupted, which facilitates the easy penetration of various pathogens.
Naturally, rational use of toothpaste and mouth fresheners, eating foods of different tastes (including sour, salty, etc.) and alcoholic drinks in reasonable quantities cannot provoke glossitis. For infection, a necessary condition is not only a constant negative effect on the oral mucosa, but also a general decrease in immunity, in particular against the background of diseases such as hepatitis or herpes.
Classification
There are inflammatory and non-inflammatory glossitis. All kinds of microorganisms are to blame for the occurrence of inflammatory glossitis: fungi, bacteria, viruses. Inflammatory glossitis is divided into superficial and deep.
However, glossitis can develop not only as a result of infectious exposure, but also with systemic diseases, local exposure to aggressive factors on the tongue (injuries, burns, smoking, etc.)
There are the following forms of non-inflammatory glossitis:
- Desquamative;
- Diamond-shaped;
- Hairy;
- folded
- Atrophic;
- Gunterovsky.
Desquamative glossitis
This is an inflammatory-dystrophic disease of the tongue, which is accompanied by specific changes on the back of the tongue and its lateral surfaces. Desquamative glossitis is a fairly common pathology, and this disease affects people of any age.
This pathological condition often develops against the background of existing diseases of the digestive tract, collagenosis, infectious and neuroendocrine diseases.
As a rule, desquamative glossitis is not accompanied by any subjective sensations. A person learns about the disease by chance, either by looking at his tongue in the mirror, or at a dentist’s appointment. It is rare to hear a person with this form of glossitis complain of a burning sensation in the tongue.
Externally, the disease manifests itself as the appearance of red round spots on the tongue. Often the lesions enlarge and merge with each other. The spots form a bizarre pattern on the tongue, like a drawing on a map, which is why the disease is called “geographic tongue.”
Villous glossitis
A very recognizable type of disease in which the papillae in the middle and back of the tongue grow and change color - they can turn brown or even black. Although no particularly painful sensations were noticed. Experts note that men over 40 years of age are more susceptible to villous glossitis.
It develops mainly due to impaired metabolism, stomach diseases, excess or insufficient content of vitamins in the body.
Diamond-shaped glossitis
The diamond-shaped form of glossitis in which the papillae of the tongue atrophy and a diamond-shaped focus forms in its center. Its length is about five centimeters and its width is up to two centimeters. Causes: lack of vitamin C, inflammation of the gastrointestinal tract, smoking, candidiasis (fungal infection).
Diamond-shaped glossitis has several forms:
- In the smooth form, small areas that are pink or red in color are affected. There are no papillae in these areas. A feeling of a foreign body appears on the tongue; upon palpation, lumps are felt. There may be a burning and tingling sensation that gets worse when eating.
- Lumpy glossitis is characterized by lesions that consist of bumps separated by folds. The bumps can be of different sizes. There are no papillae on the folds and tubercles. The affected areas become red with a bluish tint.
- In the hyperplastic form, papillary formations grow on the tongue, having flat tops and wide bases.
Inflammatory glossitis
When a fungal infection of the mouth occurs, the tongue is also involved in the process. Due to inflammation, the tongue swells and turns red. Fungi actively reproduce, which is why a white coating quickly forms on the surface of the tongue.
Bacterial and viral infections can also cause glossitis. If inflammation is localized only on the mucous membrane, they speak of the development of superficial glossitis. Redness and swelling of the tongue indicate catarrhal glossitis; if ulcers form on the tongue, this is ulcerative glossitis.
When the infection penetrates deeper into the tissue of the tongue, deep glossitis develops with the formation of an abscess. The pathological condition is accompanied by throbbing pain, uneven enlargement of the tongue with swelling in the area of the abscess, slurred speech, and increased salivation.
When the infection spreads to the entire tongue, as well as the lower jaw and neck, they speak of the development of phlegmonous glossitis. The development of this condition is indicated by severe pain in the tongue, difficulty speaking and breathing, enlargement of the mandibular and cervical lymph nodes, weakness, and high temperature. This condition requires emergency treatment.
Folded glossitis
This is a congenital abnormality of the tongue. Clinically manifested by folds on the back of the tongue, with the deepest fold located longitudinally along the midline of the tongue. A folded tongue does not cause discomfort; treatment is required only for a significant number of folds and is carried out for aesthetic purposes.
Interstitial glossitis
It is one of the symptoms of syphilis in the tertiary period. Part of the muscle tissue of the tongue is replaced by interstitial (connective). The tongue looks like a quilted blanket, where areas of muscle tissue are raised and grooves of connective tissue tighten the tongue.
In the absence of antisyphilitic treatment, complete degeneration of muscle tissue into connective tissue occurs. Interstitial glossitis is a precancerous disease and very often the cells become malignant, resulting in cancer of the tongue.
Differential diagnosis of desquamative glossitis
Desquamative glossitis is differentiated:
- with secondary recurrent syphilis . The decisive factor in the diagnosis is the Wasserman reaction, the detection of pale treponema in the lesions, infiltration at the base (papules are covered with a whitish coating), in the center of the papules as a result of trauma and maceration, a deep erosion or ulcer is formed, covered with a purulent-bloody coating;
- with a typical form of lichen planus , which is characterized by small papular rashes of a whitish-pearly color, forming a characteristic lace pattern on the unchanged mucosa, mainly on the lateral surface, in the posterior third of the tongue. The filiform papillae are preserved and there is no desquamation of the epithelium. Lesions on the oral mucosa are combined with damage to the skin. Subjective sensations are either absent or disturbed by dryness and tightness of the oral mucosa;
- with a flat form of leukoplakia . On the unchanged mucosa, limited, non-rising plaques of a grayish-white hue appear; when scraped with a spatula, they are not removed and are painless. Smoothness of the filiform papillae is observed;
- with vitamin B12 deficiency, Addison-Biermer disease . Endogenous factors may include surgical interventions on the stomach, disturbances in absorption conditions, and increased destruction of vitamin B)2 in the intestine. Exogenous forms of B,2-vitaminosis are caused by insufficient supply of vitamin B12 from the outside. Often the initial signs of the disease are pain and burning in the tongue. The classic symptom is Gunter-Miller glossitis - a “varnished” tongue. Atrophy of the filiform papillae occurs; areas of epithelial desquamation can cover the entire surface of the tongue or be located in the form of inclusions, often resembling the Latin letters V or U. Characteristically, there is no plaque. Desquamation of the epithelium can also occur in other areas of the mucous membrane, with the exception of the gingival mucosa. Multiple caries is often found;
- with changes in vitamin B1 deficiency ariboflavinosis . The mucous membrane of the mouth, lips, and eyes is affected. With damage to the lips (vertical cracks), changes in the tongue simultaneously appear - at the beginning of the disease, hyperplasia of the fungiform papillae occurs, hypertrophy of the foliate papillae may occur, dental imprints are visible on the tongue, but later all papillae atrophy, the surface of the tongue becomes smooth, shiny, bright red colors. Often, aphthae-like formations develop on the oral mucosa;
- with changes in the tongue in systemic scleroderma - changes in the tongue area are observed in all patients without exception. This is mainly desquamative glossitis (migratory form), which is considered as a particular manifestation of a general pathological process with damage to the microvasculature, leading to generalized disorganization of connective tissue and secondary changes in various organs and tissues. Patients with systemic scleroderma complain of a white coating on the tongue, especially in the morning, dullness and distortion of taste sensitivity and a burning sensation that intensifies when eating. Areas of desquamation are paler, their migration proceeds more slowly against the background of compacted (sclerosed) muscle tissue and is accompanied by dry mouth. In the chronic course of the disease, the lesions are of a fixed nature. The mobility of the tongue, its removal from the oral cavity and movement to the sides are limited and difficult. With repeated maximum elevation of the tongue, a characteristic diagnostic symptom is observed - whitening of the tip of the tongue, which characterizes vasomotor ischemic disorders that lie in the pathogenesis of changes in the tongue in systemic scleroderma;
- with changes in the language in diseases of the gastrointestinal tract :
a) in patients suffering from chronic colitis and enterocolitis , constant symptoms: glossitis, aphthous stomatitis and seizures occur against the background of a significant deficiency of vitamins PP and B2 [Saidakbarova H.I., 1967]. M.A. Malygina [1966], when examining children suffering from dysentery, noted the development of desquamative glossitis on days 7–14 of the disease;
b) with chronic gastritis, desquamative glossitis is observed with atrophy and smoothness of the papillae of the tongue, which occurs with secretory insufficiency of the stomach. With exacerbation of the disease, a fixed form of desquamative glossitis is more often observed. Subjective complaints include a burning sensation, pain, especially when eating irritating foods. The duration of existence of such foci of desquamation varies from 3-5 days to 2-3 weeks;
c) with gastric ulcer - a migratory form of desquamative glossitis. On the dorsal surface you can see foci of desquamation of the epithelium from small pinpoints to 0.5-1.5 cm. Their localization is constantly changing, there is a movement of foci along the surface of the tongue, which causes the migration of pain. Spontaneous disappearance of foci is possible, which distinguishes this form of desquamative glossitis from the “geographical” tongue; d) in diseases of the liver and gall bladder, cirrhosis of the liver, epidemic or viral hepatitis (Botkin's disease), desquamation of the epithelium of the tongue on its dorsal surface and atrophy of the fungiform papillae are noted;
— with changes in the oral cavity in diseases of the cardiovascular system . Desquamation of filiform papillae is noted. The tongue becomes smooth and shiny (“polished tongue”). Patients complain of a burning sensation. With myocardial infarction, especially in the first days of the disease, the greatest changes in the tongue, desquamal glossitis, and deep seizures in the corners of the mouth are noted. An important diagnostic sign for heart disease is hemorrhages in the papillae and interpapillary structures of the tongue. Extravasation noted on the back of the tongue is a consequence of hemodynamic disturbances in the capillary bed;
- with pathological phenomena in the language of persons exposed to ionizing radiation . Atrophic and desquamative glossitis is observed in 68% of patients with atrophic gastritis exposed to ionizing radiation. The most radiosensitive areas of the oral mucosa are the lateral surface and tip of the tongue, floor of the mouth, soft palate, cheeks, gingival margin and gingival papillae. Inflammatory processes on the mucous membrane are areactive (pallor, swelling, severe pastiness), and dystrophic processes in the periodontium are characterized by progressive resorption of bone tissue.
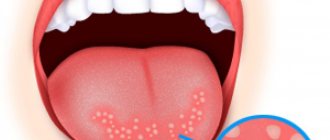
Symptoms of glossitis
Early symptoms of glossitis (see photo) are a burning sensation and discomfort in the mouth. There is also a feeling of the presence of a foreign body in the mouth. After some time, the tongue acquires a burgundy and bright red tint and swells a little. As the swelling of the tongue increases, salivation also increases. The sense of taste becomes dull or often completely lost, or a distortion of taste sensations occurs. The process of eating does not bring pleasure, causing only unpleasant sensations. As a result of swelling and soreness of the tongue, the speech of patients becomes slurred, since the tongue practically does not participate in the formation of sounds to reduce pain.
If this disease is not treated, it becomes chronic. With chronic glossitis, the tongue swells strongly and tightly, and its very structure changes. In advanced forms of glossitis, mushroom-shaped growths grow on the tongue.
With glossitis, which is caused by pathogenic microflora, symptoms of acute inflammation appear, namely hyperemia, severe swelling, pain, and local high temperature. With viral glossitis, the entire surface of the tongue becomes covered with blisters, which burst and leave wounds in the form of erosion. If glossitis does not promptly seek medical help, the disease can spread to the oral mucosa, especially with reduced immunity. With candidal glossitis, the tongue becomes covered with a white coating, becoming loose and dense. You can also notice hyperplastic changes in the tongue.
With an advanced form of glossitis, an abscess is possible. The onset of this process may be indicated by the presence of local acute throbbing pain. The patient's speech becomes very unintelligible, the tongue greatly increases in size, and the area of the abscess itself is characterized by more severe swelling and pain. Salivation constantly increases as the abscess develops.
If glossitis is complicated by phlegmon, then swelling of the tongue and suppuration become more pronounced and spread to the bottom of the mouth and neck. The pain syndrome intensifies, the process of eating becomes more complicated until the patient completely refuses to eat. Speech and breathing become difficult, and attacks of suffocation are possible. General signs of intoxication with glossitis complicated by phlegmon become more pronounced: regional lymph nodes enlarge, temperature rises, and weakness appears.
Treatment
How to treat glossitis is determined by the doctor depending on the type of disease.
General principles of therapy:
- First of all, medical procedures are carried out to improve the health of the oral cavity.
- Antiseptics are prescribed for rinsing the mouth. Nystatin is suitable for adults and children.
For most types of glossitis, therapy with Miramistin, Chlorhexidine, Laripront, Furacilin is prescribed. - If an infectious form of the pathology is detected, the patient is prescribed antibiotics (for example, Amoxicillin, Doxycycline).
- The preparations Vinizol, Kamistad, Solcoseryl, Malavit are used to apply ointment compresses to the tongue.
These drugs have powerful analgesic and wound healing effects. - After completing drug therapy, it is recommended to treat the problem area with sea buckthorn oil. This will restore healthy microflora in the oral cavity.
If glossitis is a consequence of a lack of vitamins, reduced immunity or an infectious disease, complex therapy is carried out with the obligatory elimination of the root cause.
Glossitis is a disease that is not only unpleasant, but also dangerous, capable of causing serious complications and consequences.
The patient can expect serious breathing problems, the formation of papillomas on the tongue, and the spread of the inflammatory process to other organs and systems. To prevent them, you need to take care of your health and regularly visit the dentist's office.
Diagnosis of glossitis
At the initial stage, glossitis of the tongue will probably not be noticeable, and may not be diagnosed. The detection of changes in the oral cavity can be determined by a doctor during a medical examination or when visiting for another ailment of the body. Diagnosis begins with collecting complaints. They clarify: what is troubling, when it appeared, the sequence, duration of the illness, what the patient used to alleviate the condition (especially the emphasis on antibiotics, glucocorticosteroids, cytostatics - as a factor in the development of glossitis of the tongue). The general well-being of the patient and the occurrence of health risk conditions are assessed. The somatic pathology is clarified, and if necessary, an appointment with a specialist is issued. Pregnancy and lactation, the presence of TORCH infections (herpes, cytomegalovirus, toxoplasmosis) are emphasized. Factors contributing to chronic traumatization of the tongue are identified: preference for junk food, diseases of the nervous system, overestimation of fillings, defective orthopedic devices. The phenomenon of dysbiosis (change in the composition of microflora), bad habits, and what hygiene products the patient uses are clarified.
During examination, the symmetry of the face, skin, lymph nodes, and mouth opening are assessed. Visualization of the oral cavity establishes the condition of the mucous membrane and organs. There is a change in color, plaque, erythema, aphthae, erosions, rashes, pustules, plaques. The phenomenon of bleeding gums and subsequent removal of plaque from the tongue. A change in the volume and shape of the tongue, swelling or foreign inclusions are visualized. Trauma factors are determined by imprints on the mucous membrane (over-inflated fillings, defective orthopedic devices). Diseases of teeth and periodontal tissues as carriers of microflora are identified. In correlation with the scale of penetration, glossitis of the tongue is differentiated into superficial (damage to the mucous capsule of the tongue), catarrhal (damage to the mucous membrane, the occurrence of edema), deep (the occurrence of abscesses), ulcerative (presence of a mucosal defect covered with plaque, when removing the wound bleeds), phlegmanous (defeat the entire tongue, with distribution on the tissues of the oral cavity and neck, with the appearance of many purulent foci in the tongue).
These transformations actively manifest themselves in inflammatory glossitis, the source of infection of which is the microflora of the oral cavity. In case of non-inflammatory glossitis, the primary changes are not formed in the oral cavity and the examination should be carried out by a doctor corresponding to the damage to the somatic system. In the case of an infectious cause of development, the doctor selects additional methods of medical examination: bacteriological examination of a smear, histological examination of tissues, general blood test, biochemical medical examination of blood, blood examination for HIV, syphilis and TORCH infections, stool analysis (for helminths - exclude helminthic infestation and dysbiosis). Refer to related specialists: ENT doctor (the phenomenon of inflammation of the upper respiratory tract), gastroenterologist (symptoms of the digestive organs), immunologist-allergist (history of allergies, regular colds, immunogram: for desquamative and contact catarrhal glossitis), hematologist (change in color of the mucous membrane, atrophy , varnished surface), therapist and rheumatologists (for collagenosis), infectious disease specialist and dermatologist (skin rashes).
How to treat glossitis?
At the beginning of treatment, special attention should be paid to proper oral hygiene: brush your teeth at least 2 times a day, rinse your mouth after eating, and do not neglect preventive dental examinations. It must be remembered that spicy and excessively hot foods worsen the course of glossitis. Therefore, such foods should be excluded from the diet during treatment.
Various purees and pureed soups, viscous porridges are recommended. During the day, you should rinse your mouth with a weak solution of potassium permanganate, a solution of furatsilin or chlorhexidine. Painkillers (a solution of Anestezin in glycerin, a solution of chloral hydrate, trimecaine or lidocaine) and restorative agents for the mucous membrane (rosehip oil, retinol solution, peach oil, Solcoseryl, vinylin) are used locally. For the purpose of disinfection, you can rinse the oral cavity with a solution of Rotokan, Romazulan.
- Purulent-phlegmonous (deep) glossitis. Excision (removal) of the abscess or pus of phlegmon is performed surgically. In the postoperative period, a course of antibacterial therapy is prescribed.
- Desquamative glossitis. To cure desquamative glossitis, it is necessary to treat the disease that led to inflammation of the tongue.
- Diamond-shaped glossitis. Most often, this type of glossitis does not require special treatment. But with the progression of the disease and the development of papillomatous (hyperplastic form) glossitis, surgical removal of the affected area is performed in order to prevent the development of precancerous and cancerous diseases of the tongue.
- Gunter's glossitis. Since Gunter's glossitis is not an independent disease, but refers to the symptoms of B12-folate deficiency anemia, treatment is aimed at eliminating the cause of anemia. Thus, treatment consists of compensating for the deficiency of vitamin B12 and folic acid, as well as normalizing the functioning of the gastrointestinal tract.
- Villous glossitis. The changed papillae are removed using tweezers. After the procedure, the surface of the tongue is treated with a 3% solution of copper sulfate, resorcinol, and salicylic alcohol.
- Candidal glossitis. Antifungal drugs are used to treat candidal glossitis.
Treatment of folded (scrotal) tongue
The anomaly usually does not bother its owners, however, sometimes they complain about its appearance: cracks.
A folded (scrotal) tongue requires especially careful care. Because food residues may be trapped in the folds. Because of this, bad breath occurs, as well as accompanying unpleasant symptoms: burning and inflammation.
In addition, the grooves may bother people who have suffered acute infections or surgical interventions. The reasons in this case are also clear: the overall tissue reaction in the body decreases, and the sensitivity of the surface of the folded tongue increases significantly. Therefore, it reacts painfully to chemical irritants and drugs.
If the patient does not properly care for the diseased organ, then the inflammatory processes can drag on, and this is a very favorable place for the development of fungal infections.
The dentist treats this pathology. It is he who will select oral care.
Sometimes a folded tongue requires surgery. This happens in cases where the organ is too enlarged and interferes with the patient. The operation involves excision of part of it.
So, in general, drugs are used to eliminate related problems:
- Fungal and bacterial diseases: anti-inflammatory, antifungal drugs, immunocorrectors, antiseptic treatment.
- Candidiasis: clotrimazole cream, shading with aniline dyes, 10% sodium borate solution in glycerin.
- Painful sensations: antiseptic rinses, mouth baths with citral solution, application of medications with anesthesin.
Folk remedies
Folk remedies include anti-inflammatory decoctions with the addition of herbs such as chamomile, sage and calendula. Also, for glossitis, it is recommended to rinse your mouth with water with the addition of a small amount of soda.
- Steam 15 grams of dried crushed chamomile flowers with boiled water - 300 milliliters. Leave the mixture to sit for several hours. Rinse your mouth with the strained infusion after each meal and before going to bed.
- Tea tree oil - the product must be mixed with sea buckthorn oils or regular vegetable oil in equal quantities. Several times a day, this mixture should be kept in the mouth on the damaged area of the tongue. Tea tree oil has an antibacterial effect.
- Hydrogen peroxide - to prepare, add 2 teaspoons of a weak solution of hydrogen peroxide to a glass of boiled warm water, rinse your mouth several times a day after meals. The product has a strong antibacterial effect.
- Take a few medium-sized potatoes, peel them and chop them finely. Wrap the resulting pieces in cheesecloth and squeeze out the juice. It is worth noting that when treating glossitis with potatoes, do not crush the potatoes with a press. Rinse your mouth with juice after every meal. After the procedure, wait 30 minutes. interval, and then start rinsing again.
- Sage has a powerful disinfectant effect. Brew 10 grams of dried crushed leaves of the plant in boiled water - 200 milliliters. It is preferable to infuse the composition in a thermos for at least two hours. Strain the mixture and use to rinse the mouth three times a day.
How is the treatment carried out?
After confirming the diagnosis of diamond-shaped glossitis, the oral cavity is sanitation (treatment of caries and removal of tartar).
For the entire period of the treatment process, the patient must avoid spicy, salty and spicy foods. The food is not hot, it should have a soft consistency (exclude hard foods).
When treating this pathology, the following is used:
- medications;
- recipes for traditional medicine;
- method of surgical therapy.
Tongue care
Along with the use of medications, it is necessary to perform hygiene procedures that will reduce the likelihood of the proliferation of pathogenic microflora.
Therefore, you should adhere to the following recommendations:
- Perform oral hygiene procedures at least 2 times a day. At the same time, avoid mechanical impact on the affected area.
- Rinse with antiseptics after each meal.
- The resulting plaque cannot be removed with your fingers. Before this, use cotton swabs pre-moistened in antiseptic.
- It is allowed to use pharmaceutical rosehip or peach oil.
- To eliminate pain, tingling or burning sensations, it is best to use applications with local anesthetics.
Medicines
Comprehensive treatment of median rhomboid glossitis is important, during which drugs of different effects are used.
Main choice medications:
- Vinizol accelerates the healing of the atrophic area of the surface of the tongue (spray).
- Solcoseryl in gel form improves trophic processes, which ensures rapid tissue regeneration.
- Chlorhexidine solution eliminates the effect of pathogenic microflora.
Drugs that inhibit the growth of candida fungus. Both local dosage forms and medications in tablet form are used. Complex therapy includes:
- glycerin-based borax solution (10%);
- boric acid for rinsing (2%);
- tablets Nystatin, Lamisil or Terbinafine.
Medicinal forms that relieve inflammation and pain:
- Tantum Verde;
- Holisal;
- Ketoprofen;
- Hexasprey or Metrogyl Denta.
Drugs that reduce the production of histamine can reduce swelling of the mucous epithelium: Claritin, Zyrtec, Loratadine.
A group of corticosteroids is prescribed in case of severe atrophic processes (Prednisolone or Hydrocortisone).
Immunomodulators allow you to restore the body’s immune status (Cycloferon, Laferon or Viferon). For the same purpose, multivitamin complexes with a high content of B vitamins are used.
Traditional methods
Traditional recipes are allowed to be used only after prior consultation with a doctor. They are used as an addition to complex therapy. On their own, they will not be able to relieve the severity of the inflammation process and relieve signs of atrophy.
Most often, medicinal infusions are prescribed using the following medicinal compounds:
- Chamomile or calendula inflorescences, brewed at the rate of one tablespoon per 200 ml of boiling water, have an antiseptic effect. They are used to rinse the mouth (up to 6 times a day).
- Sage tincture is used in a similar way.
- An infusion of oak bark has a good effect. To prepare it, use two tablespoons of dry matter, which are boiled in a water bath with the addition of 200 ml of water. The rinsing procedure is performed at regular intervals (7 times during the day).
- Add 20 drops of rosehip, sea buckthorn or eucalyptus oil to a glass of water and rinse three times a day.
Operative therapy
The lumpy and hyperplastic form sometimes does not respond to conservative treatment methods. In this case, surgical treatment is used by excision of tissue within the affected area.
In addition, papillomatous formations can be removed using the cryodestruction method (a jet of liquid nitrogen is applied to the surface). This causes them to be rejected.
Nutrition and diet
Food for glossitis should be gentle on the oral mucosa.
Characteristics of diet for tongue lesions:
- food must be natural, freshly prepared, thermally processed,
- the temperature of food and liquid should be warm, within 36-40C,
- food should be soft, preferably ground, homogeneous,
- do not drink carbonated and sour drinks,
- refrain from coffee and strong tea,
- exclude injuries from bones from fish and poultry,
- do not eat spicy, hot, salty and sour foods (spices, vinegar dressings, all types of peppers, mustard, etc.),
- refrain from sweets (especially lollipops, chemical sweets), since glucose is a good food for many microorganisms,
- do not drink alcohol, refrain from smoking,
- refrain from eating sour fruits (especially citrus fruits) and berries,
- do not consume canned foods, pickles,
- exclude smoking from the diet.
If there are concomitant diseases that cause glossitis, appropriate therapeutic diets are followed:
- Table No. 1, No. 2, No. 3, No. 4 – for diseases of the gastrointestinal tract,
- Table No. 5 – for diseases of the liver and biliary tract,
- Table No. 12 – for diseases of the nervous system,
- Table No. 13 – for acute infectious diseases and so on.
Possible causes of pathology
The exact causes of the anomaly are unknown. But there are a number of factors that can provoke the appearance of pathology:
- chronic diseases of the liver, stomach, duodenum;
- skin diseases;
- pathologies of the nervous system;
- pathologies of the endocrine system;
- bone marrow diseases;
- acute infections;
- violation of the mucous membrane of the tongue and its trophic function;
- lack of vitamins and essential microelements in the body;
- collagenosis;
- human reaction to vaccination;
- hormonal changes (pregnancy, menopause, lactation).
Prevention
To prevent glossitis, you must adhere to the following rules:
- visiting the dentist's office at least 2 times a year;
- regular oral hygiene;
- removing plaque and tartar from the surface of teeth;
- treatment of diseases that lead to glossitis;
- exclusion of spicy and salty foods from the diet;
- strengthening the immune system;
- rejection of bad habits.
Regular prevention of glossitis should be performed by people who are at risk. We are talking about patients who smoke, abuse alcohol, prefer spicy or salty foods, and regularly use mouth rinses and mouth fresheners. All people who neglect visits to the dentist are at risk for glossitis and any other disease of the teeth, gums or tongue.
Forecast
Glossitis is a serious disease that, in the absence of comprehensive treatment, can lead to abscess, cancer and death. With timely treatment, the prognosis is favorable. Therapy should be prescribed strictly by an experienced and professional dentist. To exclude complex consequences, consultations with a gastroenterologist, urologist, gynecologist, infectious disease specialist, or oncologist may be necessary.
Oral candidiasis Stomatitis in children: photos, symptoms and treatment Pancreatitis Gastritis Chronic pharyngitis Cheilitis