Pathogenesis (origin and development)
Odontogenic periostitis is usually classified according to the phase of the disease, as well as the nature of the pathological process. The possible types are clearly demonstrated by the international classification of the ICD, where each disease is assigned a specific code.
It is quite possible to identify the moment of onset of periostitis, as well as to trace further development (pathogenesis). This will be done using progressive methods used in modern dentistry.
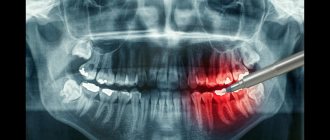
Along with external examination and palpation, the attending physician often prescribes an x-ray examination. Using the resulting image, the specialist assesses the condition of the roots and periapical area. The only drawback of this method is the inability to identify the fact of periosteal thickening in the first three days from the onset of the disease.
How can you not treat periostitis?
Periostitis is a dangerous disease that can lead to serious illness and can be considered a threat to health and even life. Any delay, even the slightest, can be fatal.
Self-medication and “folk” remedies are something you should not do under any circumstances. The scope of “home” treatment includes:
- self-prescription of antibiotics. It is possible that acute inflammation can be stopped, but without further treatment, the “flux” will make itself felt again, and with even more pronounced symptoms;
- lack of treatment can cause inflammation to spread and develop into complications: abscesses and phlegmon of the head and neck. Let us recall that acute purulent processes and, especially, the accumulation of pus in the maxillofacial area, a place that is abundantly supplied with blood vessels, are dangerous for the spread of infection to the brain area;
- It is strictly forbidden to apply heat or use compresses. Such actions only accelerate the process of spreading pus, and the consequences will not be long in coming;
- taking aspirin. Taking this drug can also provoke the rapid development of complications.
Types and classification of periostitis
There is a detailed classification based on a number of key criteria. A brief essence and description of the latter will be given below.
So, for example, based on the degree of participation of pathogenic bacteria in the progression of inflammation, periostitis occurs:
- purulent,
- aseptic.
Depending on the severity of the process, there are such varieties of the disease in question as:
- acute purulent periostitis,
- chronic periostitis.
If we take the nature of exudative discharge as a basis, periostitis can occur in two types:
- exudative,
- proliferative.
According to the form of the disease, periostitis is:
- simple,
- fibrous,
- serous,
- purulent,
- ossifying.
In addition, there is a classification, the main criterion of which is the path by which the infection penetrates the periosteal tissue. According to this gradation, the following problems are identified:
- acute odontogenic periostitis of the jaws (the main cause is a diseased tooth);
- hematogenous (infection entered through the blood);
- lymphogenous (the pathological process spreads throughout the lymph system);
- traumatic (formed by injuries to the periosteum).
Causes of purulent periostitis
Periostitis rarely occurs as a separate disease; it usually acts as a complication of various diseases of the oral cavity and larynx. In most cases, the cause is chronic periodontitis in an advanced form, as well as periodontitis, inflammation of wisdom teeth, alveolitis, and jaw cyst. Prerequisites for suppuration of the periosteum can be bacterial infections against the background of tonsillitis, influenza, otitis, acute viral disease, measles, scarlet fever.
Acute development of periostitis may also be associated with other conditions:
- difficult tooth extraction;
- surgical interventions in the oral cavity;
- mechanical injuries of the jaw with the formation of wounds;
- inflammatory processes in facial tissues;
- overheating, hypothermia, heavy physical exertion;
- eruption of the baby's first teeth;
- improper treatment of dental diseases;
- reduced immunity.
The cause of purulent periostitis can be clearly expressed and understandable, but sometimes it is difficult to diagnose if visible pathological conditions have not been observed before. Inflammation can occur against the background of several favorable factors. For example, after treated caries, a wound has formed near the root of the tooth, which, against the background of poor immunity, becomes infected from the outside with bacteria (staphylococci, streptococci). This is how suppuration occurs and the development of acute purulent periostitis. It is important to clarify all possible factors that could influence the appearance of gumboil during a consultation with a dentist. Then the treatment will be targeted and comprehensive.
Causes of occurrence (Etiology)
The etiology and pathogenesis of periostitis in modern dentistry have been studied quite well, due to which the effectiveness of the treatment processes is high. The most common factors that cause periostitis of the lower jaw are trauma or infection. According to statistics, this problem occurs in 5.4% of patients with inflammation in the facial and jaw areas. At the same time, the acute form is present in about 95% of patients, and the chronic form is present in only 5%.
It should also be noted that localization of periostitis on the lower jaw occurs 1.5-2 times more often. At the same time, the clinical picture (both local and general) is distinguished by a certain originality.
The success of treatment directly depends on its timeliness. If the disease is detected at a very early stage, the treatment process proceeds quite quickly and without any serious consequences. As for situations where the problem has already demonstrated some progress, elimination will require significantly more effort, time and money (in this situation, the price of the corresponding dental services usually increases significantly). Plus, the likelihood of purulent complications occurring is very high.
For what reason does the disease in question occur? There are several of these. The main sources invariably include complicated caries, when pathogenic microflora penetrates through microchannels into the dental cavity, after which it spreads to the tissues surrounding the root.
It is also not uncommon for the cause of this disease to be chronic apical periodontitis. Here there is a gradual movement of pathogenic microorganisms through the channels further and further. In the absence of proper treatment, the soft tissues are affected first, and then the periosteum.
Additionally, you should know that staphylococcus constantly lives in the oral cavity. With the weakening of the natural immune defense, the population of the latter shows significant growth, and the periosteum, in turn, becomes inflamed.
The cause of the lymphogenous and hematogenous form is often ARVI, ENT diseases, as well as scarlet fever and measles, which are classified as infectious diseases. As for traumatic periostitis, its occurrence is a consequence of the removal or injury of units of the dentition, surgical intervention, infection of wounds on the facial surface, jaw fractures, etc.
The appearance of periostitis in a number of patients is due to previous overheating or hypothermia. Overloads of a physical and emotional nature are also among the sources of the problem.
In rare cases, periostitis is caused by tuberculosis, as well as other diseases that cause serious complications on the jaw periosteum.
Possible complications of periostitis
Any form of periostitis should be treated by a qualified specialist. Self-medication and the use of traditional methods for this pathology are not advisable. Moreover, attempts to unauthorizedly open an abscess, clean it, rinse with improvised means and uncontrolled use of antibiotics will never cure the disease. Such independent measures will only complicate an already severe pathology.
Lack of adequate treatment, including surgical opening of the flux, can lead to the development of osteomyelitis - purulent-necrotic destruction of bones and tissues. Pathology can develop directly on the affected jaw, and also spread to nearby areas. This disease can only be treated in a hospital setting using a whole range of complex therapeutic measures.
Another common consequence of untreated purulent periostitis is the transition of the disease to a chronic form. This outcome of events leads to gradual degradation of facial tissue, ossification, and serious physiological and aesthetic problems.
Purulent processes tend to spread quickly. If suppuration is not stopped locally, it spreads to nearby human organs and systems. The abscess can spread to the neck, face, head and cause cellulitis or sepsis. These two conditions require immediate attention, otherwise they can be fatal.
Symptoms and signs of periostitis
Symptoms of periostitis of the jaw in acute form are determined by the existing form of the disease. The current state of immunity, as well as other concomitant diseases, also have a significant impact. At the same time, there are also characteristic signs that make it possible to make an accurate diagnosis.
Note that periostitis is a disease with gradual development. First of all, the gums swell slightly, and when pressing on a unit of the dentition, painful sensations appear. If you notice such seemingly insignificant symptoms, you should contact a specialist immediately. Preferably on the same day or, in extreme cases, the next. True, here it should be understood that by the morning of the next day there is a high probability of significant swelling of the cheek.
If we talk about the form of the disease with serous infiltrate, the list of typical signs looks like this:
- redness of the mucous membrane,
- quite bearable pain,
- the formation of a painful swelling in the fold between the cheek and gum,
- probable increase in body temperature to 37°C,
- acquisition of asymmetrical proportions by a person,
- enlargement of the postauricular and submandibular lymph nodes (lymphadenitis).
When a purulent infection is present, a significant deterioration in the patient’s condition is observed:
- the appearance of obvious signs of intoxication,
- general soreness,
- temperature rise to 38°C,
- noticeable swelling of the cheek,
- irritation of pain along the trigeminal nerve,
- a clear sensation of pulsation in the swollen area,
- there is a possibility of fistula formation,
- palpability of fluid vibrations when pressing on the area between the gum and cheek.
Symptoms of periostitis
Manifestations of periostitis differ depending on the patient’s age, stage and form of the disease, and individual characteristics of the body. However, in most cases there are a number of obvious signs indicating the disease:
- toothache – can “radiate” to the ear, eye socket and/or temple, sometimes the pain does not allow you to open your mouth normally and limits jaw movements;
- pathological tooth mobility;
- swelling of the gums, lips - in some cases, swelling distorts the face;
- hyperemia of the oral mucosa (overflow of blood vessels);
- the appearance of an abscess - a purulent tumor, which is popularly called gumboil;
- enlargement and thickening of lymph nodes in the face and neck;
- feeling unwell – body temperature within 38 degrees, weakness, headache, etc.
Sometimes a fistula tract forms in the flux, through which pus enters the oral cavity. Painful symptoms when such a course appears become less pronounced.
Unlike pulpitis and periodontitis, which are also accompanied by pain, with periostitis there is always a distortion of the contours of the face. Mildly expressed or very noticeable deformations are always present.
Doctors note that in most patients the disease makes itself felt after physical or emotional stress, hypothermia or overheating.
Periostitis of the upper jaw
Diseases similar to periostitis
In practice, there are diseases whose symptoms are quite similar to periostitis:
- adenophlegmon (a purulent infiltrate forms in the soft tissues of the oral cavity; there is no inflammatory reaction of the periosteum),
- gum abscess (the area of suppuration is sharply limited, external damage to the skin is clearly visible),
- pulpitis of the lower molar (there is constant aching pain, which intensifies at night; there is no swelling of the oral mucosa),
- osteomyelitis of the lower jaw, identified using panoramic radiography (there are severe symptoms of general intoxication, as well as radiological signs of existing bone tissue damage).
The above list is not complete. There are other diseases that look very similar to the symptoms of periostitis. For example, syphilitic manifestations. In view of the difficult situation described, only the attending physician can make an accurate diagnosis.
Symptoms
While the inflammatory process is in its initial stage, parents may not notice its dangerous development. The child is bothered by moderate pain in the oral cavity, which is why he refuses to eat. The gums swell slightly, the baby is capricious.
ATTENTION! Periostitis in children develops quickly; if the initial symptoms of the disease are not noticed, the inflammation will progress. The child requires emergency help from a pediatric dentist, as the pathology is fraught with serious consequences - an abscess, phlegmon, and sepsis may occur.
The following symptoms indicate the spread of the disease:
- aching pain in the tooth becomes constant, throbbing, intensifying when eating or pressing on the affected area;
- the gum swells, turns red, and an abscess appears on it;
- swelling of the soft tissues of the face is observed - if periostitis affects the upper jaw, not only the cheek, but also the area near the ear and eye swells. Flux localized on the lower jaw causes swelling of the cervical area;
- inflammation may spread to the lymph nodes;
- the child’s temperature rises, he becomes lethargic, weak, and is often capricious;
- there is an unpleasant odor from the mouth.
Periostitis in children. Photo.
Diagnostics
During diagnostic measures, the specialist determines the existing similarities and differences between chronic and acute forms of periostitis, as well as other diseases of the oral cavity. It is possible to clearly differentiate the disease in question from those that have similar symptoms (cellulitis, apical periodontitis, abscess, osteomyelitis, inflammation of the salivary gland) using x-rays.
Generally speaking, a number of techniques help modern doctors to identify the problem in a timely manner, which will be discussed further.
Inspection
During a visual examination, it is possible to detect a tooth that is affected by caries to such an extent that the coronal part is destroyed by 50% or more. Such a dental unit has a clearly defined carious cavity. In this case, the infected canals are filled with pulp decay products, i.e. neurovascular tissue. A painful reaction of such teeth to percussion (tapping) is observed in 85% of cases.
X-ray
Using a radiograph, a number of other concomitant diseases and processes can be diagnosed in a patient with periostitis. The latter include:
- periodontitis (when tissue inflammation is present between the jaw bone and the root),
- impacted (i.e. unerupted) dental units,
- cyst,
- newly formed bone tissue.
Blood analysis
Through a blood test, it is possible to detect a slight increase in the level of leukocytes. In addition, a slight increase in ESR can be identified: this indicator does not exceed 12-15 mm/h.
When diagnosing, one of the key skills is the specialist’s ability to distinguish periostitis from osteomyelitis of the jaw, as well as manifestations of specific inflammatory processes (tuberculosis, syphilis). In the first case, no acute and sharp pain, as well as swelling, is observed. In the second, the image will show obvious bone destruction, which is completely uncharacteristic for periostitis.
Reasons for appearance
Depending on the factors causing periostitis, there are 2 types:
- odontogenic – divided into acute and chronic forms;
- traumatic.
Children aged 3-6 years old, when the body's protective functions are not fully formed, are more likely to suffer from gumboil than others. The appearance of inflammation of the periosteum is associated not only with caries:
- Improper oral hygiene – rotting food particles provoke the appearance of bacteria and microorganisms.
- Trauma to teeth or gums.
- Unskilled dental treatment - during the procedure, infection is introduced into the soft tissues through medical devices.
- Chronic or infectious disease - the virus enters the gums through the lymphatic system.
Inflammation of the periosteum can be either infectious or aseptic in nature (without the participation of pathogenic microorganisms).
The main causes of periostitis are:
- traumatic damage to the periosteum due to a bone fracture or injury to nearby soft tissues;
- aseptic inflammation of the periosteum from excessive load on the tendons of adjacent muscles;
- spread of the inflammatory process from nearby structures;
- chronic mechanical irritation of the periosteum;
- hematogenous metastasis of purulent infection during sepsis;
- pathological proliferation of subperiosteal tissue;
- infectious and inflammatory diseases (tuberculosis, syphilis, osteomyelitis, etc.).
Periostitis is always a complication of caries. The carious process gradually moves through the tissues of the tooth - enamel, dentin and reaches the neurovascular bundle (pulp), so caries turns into pulpitis. With further spread of infection along the root canal, pulpitis turns into periodontitis. And in the future, microbial inflammation, which often takes on a purulent character, can continue to spread along several paths, but most often turns into periostitis or gumboil.
It is necessary to remember some predisposing factors. As practice shows, periostitis is most often registered in children in the age group of 6–8 years, namely on chewing milk teeth, and extremely rarely on newly erupted permanent teeth.
Considering the characteristics of the child’s body - imperfect immune defense, structural features of the teeth - it is easier for infections to spread through baby teeth. The situation is complicated by resorption of the roots of baby teeth - resorption. The only thing standing in the way of infection is the crown, and then it goes into the thickness of the jaw. The periosteum almost immediately reacts to infection, and a localized focus of inflammation is formed.
Symptoms of flux, depending on the age of the child and the degree of resorption of the roots of baby teeth, can be recorded already with periodontitis.
Treatment of periostitis
How to treat gumboil and other manifestations characteristic of this disease? For this purpose, modern dentistry uses both local and general methods.
A simple rule applies here: the sooner treatment procedures begin, the faster the positive result will be. According to statistics, the minimum period from the start of therapy to complete recovery is one week. Obviously, such an indicator is valid only for those situations where the disease was detected at a very early stage.
During drug therapy, which is often the second treatment stage after surgery, the surface of the resulting wound is washed with specialized antiseptic compounds, as well as the application of sterile dressings soaked in a special ointment or disinfectant solution. To avoid complications and relapses, the attending physician also prescribes antibiotics.
In addition, if necessary, the treatment program may include nitrofurans, painkillers, sulfonamides, antihistamines and vitamins. In the postoperative period, the patient must also follow the recommended gentle diet, as well as perform regular rinses with antiseptics.
Antibiotics
As part of antimicrobial therapy, which is often in addition to physiotherapy in the presence of purulent processes, the doctor usually prescribes a combination of Metronidazole and Clindamycin. These drugs demonstrate high efficiency in eliminating protozoa, a variety of anaerobic bacteria, as well as gram-positive cocci, which constitute the same pathogenic flora that in the vast majority of cases is present in infected tissues.
In addition to the above, the dentist may well prescribe other antibiotics with a wide spectrum of action. These, in particular, include Tsifran St, Summed, Amoxiclav.
Drug therapy
Antihistamines
The prescription of antihistamines in the treatment of periostitis occurs along with antibacterial drugs. Thanks to the former, the body’s resistance to various infections increases, and intoxication is relieved, which was caused by the emergence and spread of purulent masses.
The most common practice is to prescribe antihistamines such as Diazolin, Erius, Tavegil, Suprastin, Fenkarol, Peritol. As a result of their intake, the body's resistance increases, and the likelihood of allergic reactions while taking antibiotics is eliminated.
Immunomodulators
The intended purpose of immunomodulatory agents is to strengthen the body's defenses, which nature has endowed humans with. When treating chronic periostitis, an effective solution to this strengthening task is of key importance.
Currently, the pharmaceutical market offers a wide range of such drugs, which makes it quite difficult to independently select the most suitable ones. For this reason, you should purchase and take only those medications that have been individually prescribed by your doctor.
Nonsteroidal anti-inflammatory drugs
In order to relieve pain, modern medicine uses special non-steroidal anti-inflammatory drugs. These, in particular, include Analgin, Ibuprofen and Paracetamol, which are recommended for use for a wide range of different diseases.
If we talk specifically about the dental field, then a drug called Ketorolac, which is capable of inhibiting COX mainly in peripheral tissues, has become widely used. As a result, the synthesis of pain sensitivity modulators and prostaglandins is significantly inhibited.
Ointments and gels
Ointment gels offered on the modern pharmaceutical market are intended for topical use. With their help, the abscess is treated, pain and swelling are relieved, and the vital activity of harmful pathogenic microorganisms is suppressed.
For periostitis, the most recommended drugs are Levomekol ointment, Metrogyl Denta, Vishnevsky ointment.
Rinsing
Mouth rinsing for the disease in question is effective in the following cases:
- at the initial stage of the disease,
- at a subsiding stage,
- in parallel with antibiotic treatment,
- if there is pain (there is a way to relieve it),
- if it is impossible to urgently visit a doctor,
- with chronic flux.
For rinsing during periostitis, medicinal herbs (sage, chamomile, gorichnik, calendula) in the form of tinctures and decoctions are used. At the same time, such herbs can be brewed either individually or as a collection.
Salt, soda, and oak bark are also suitable for relieving pain and disinfecting. And propolis tincture also has a healing effect.
Purely pharmaceutical preparations of similar action also exist. Among these, Chlorhexidine is the most popular.
Hemostatics
The use of such drugs is allowed strictly as prescribed by a doctor and only in cases where there are clear signs of bleeding. For these purposes, in the vast majority of cases, drugs such as Etamzilat and Vikasol are prescribed.
Physiotherapy
Physiotherapy is prescribed the very next day after surgery has been performed. In order to relieve inflammation of the periosteum of the tooth in any form of the disease, a specialist prescribes about 5-7 appropriate sessions.
Widely used physiotherapeutic methods include:
- fluctuarization (therapeutic effects on tissues are carried out through weak alternating current),
- UHF (tissues with good blood supply are exposed to a magnetic field),
- electrophoresis with lidase (the medicine is injected into the diseased area through current),
- laser therapy (irradiation with laser light is carried out, which leads to an additional improvement in the effect of drug therapy),
- ultrasonic influence.
To relieve pain during such treatment, we can take analgesics: Ketanov, Nimesil, Nurofen and the like.
Surgical intervention
While conservative therapy is often sufficient for serous inflammation, the purulent form, on the contrary, requires the immediate intervention of a surgeon to eliminate dental flux. During the operation, the submucosal or subperiosteal abscess is opened.
If we talk about a baby tooth that caused periostitis, such a unit must be removed. Permanent teeth that have a significant degree of destruction are also subject to urgent removal. As for the dental units that are still suitable for performing their direct functions, they need to be treated. Moreover, immediately!
Video of surgical flux removal
Principles of treatment of acute purulent periostitis
Treatment of periostitis requires an integrated approach. At the first signs of the onset of an inflammatory process in the jaw, you should consult a dentist. He will conduct a visual examination of the teeth and pharynx, which will show the location and nature of the problem. To clarify the diagnosis, laboratory blood tests may be needed. With a purulent process, leukocytes and ESR will be increased.
The most informative is thermography - a diagnostic method based on the use of infrared radiation. Thanks to it, the exact localization of inflammation and its boundaries are determined. Additionally, an x-ray of the affected teeth is taken to check for concomitant pathologies.
Acute purulent periostitis is treated with surgical intervention. A purulent abscess must be opened and cleaned of contents. To do this, a small incision is made on the gum, the affected tissue is removed, and drainage is installed to drain the pus. The surgical site must be anesthetized with lidocaine and trimecaine. In mild cases, gum irrigation is used, in more severe cases, a local injection of an anesthetic medication is used. Opening the flux yourself is prohibited; it can seriously aggravate the situation.
- If you consult a doctor in a timely manner, the tooth can be saved. It is treated and filled. Advanced inflammation often requires tooth extraction. The entire complex of treatment measures may take several sessions. Sometimes, due to the severity of the patient’s condition, the abscess is initially treated, and only then the doctor begins to treat the tooth itself. The duration of the measures also depends on the area and depth of the pathological lesion.
- The second stage of treatment is drug therapy aimed at healing the affected areas. Antiseptic and cleansing rinses are prescribed with a warm solution of soda or potassium permanganate, as well as pharmaceutical preparations. In most cases, antibiotic therapy is prescribed to stop the bacterial infection. For severe pain, analgesics are taken. The doctor may also prescribe anti-inflammatory drugs, antihistamines, vitamins, and calcium.
- At the recovery stage, physiotherapeutic methods are used - UHF, Sollux, neon irradiation, laser therapy, ultrasound. Physical therapy may be needed to restore the shape of the facial muscles.
Timely treatment of acute periostitis lasts 3-5 days, including the operation itself and postoperative therapy. If you follow all the doctor’s recommendations and instructions, complete recovery occurs. Advanced cases require longer and more painful treatment. The transition of the disease to a chronic form leads to irreversible changes in the tissues of the periosteum and constant relapses. In this case, it is impossible to do without constant monitoring by a doctor and periodic dental procedures.
There is no need to be afraid to go to the dentist. Cured acute periostitis will relieve you of health problems and large financial expenses. Self-treatment of the disease and late visit to the dentist can lead to very serious complications.
Prevention
The main principle of effective prevention is permanent control of the condition of the oral cavity. The following regular activities are recommended:
- maintain daily hygiene of gums and teeth,
- visit the dentist at least twice a year,
- undergo professional hygienic procedures (in particular, to remove tartar),
- promptly treat caries and other pathologies in a modern clinic,
- systematically undergo treatment from a periodontist (only if there are problems with gum health).
Another important recommendation is an annual x-ray examination. It will prevent periosteum disease.
Periostitis - what is it?
Despite the fact that the disease looks like a gum abscess, in reality it is an inflammation of the periosteum or periosteum. The disease affects the thin layer of connective tissue over the jaw bone. There are other types of the disease: periostitis of the tibia, calcaneus and other bones. If treatment is not started on time, the layer of connective tissue gradually becomes thicker and begins to peel off, which causes even more problems.
The essence of the disease is that serous fluid or pus begins to collect in the cavity between the jaw bone and the periosteum. The onset of the disease is accompanied by symptoms such as severe pain, which initially appears only when chewing food, gradually developing into continuous acute pain. Just as no inflammation goes away without an increase in temperature, so in acute jaw periostitis it can reach low-grade levels.
Periosteum disease occurs in people of all ages, less often in young children. The first sign of gumboil is severe swelling of the cheek. Many patients mistakenly believe that warming the sore spot has a positive effect, but the inflammatory process is activated, the pain becomes unbearable and complications in treatment appear.
READ ALSO: how to quickly remove swelling from the cheek due to gumboil at home?
Forecast
A favorable prognosis and, accordingly, a positive history of the disease can only be counted on with timely and adequate treatment. All other situations (in particular, a complication in the form of chronic hyperplastic osteomyelitis) have a number of limitations and difficulties, which are often difficult to overcome.
To successfully prevent chronic periostitis, two key rules should be followed:
- timely sanitation of the oral cavity,
- systematic correction of immunity.
Differential diagnosis
In medicine, there is such a thing as differential diagnosis. Many diseases may have similar symptoms, but the causes, and even more so the treatment, differ significantly. Therefore, it is extremely important to distinguish one disease from another.
In the case of periostitis, the differential diagnosis is made between acute periodontitis, the formation of abscesses, phlegmon, acute osteomyelitis, and sialadenitis.
In addition to the general symptoms that are characteristic of all these diseases, you can find those that will prompt the correct diagnosis. The main thing is to notice them in time. In many ways, patients themselves help in the process of differential diagnosis.