After a tooth is pulled out, an inflammatory process may begin in its socket, which often spreads to the gum tissue.
Alveolitis be treated immediately after it manifests itself, otherwise serious complications will arise.
A similar disease occurs in approximately forty percent of patients in dental clinics.
What kind of disease is this
Each tooth has roots that are located in a cavity (alveolus). It fixes the bone formation in the jaw.
microorganisms that transmit infection
can enter this hole When blood becomes infected, it does not protect the wound and the healing process stops. Due to saliva and food debris, rotting begins and the infection progresses. There are several types of alveolitis:
- Serous. A small clot of blood fluid, saliva and food residues remain in the cavity of the extracted tooth. The serous type of pathology develops after about seventy-two hours and after a week turns into a purulent form.
- Purulent. Upon examination, the specialist sees swelling and traces of blood, a gray coating and a rotten smell.
- Hypertrophic. The symptoms of purulent alveolitis gradually subside, and the person’s well-being improves. When examining the oral cavity, soft tissue tumors with pathological changes in cells are detected. There are areas of dead structures.
Alveolitis is a serious disease that is very painful. If it is neglected, it will be difficult to cure the pathology.
Therefore, it is important to contact a specialist at the first manifestations of the pathological process. Otherwise, osteomyelitis, abscess, phlegmon or periostitis may develop.
Topographic classification
This is a gradation that distinguishes types of caries according to the degree of damage to the canals. It is as common in determining the diagnosis as the classification of caries according to ICD 10. The following stages of damage are determined:
- Spot formation. The initial stage, excluding the destruction of enamel. At this stage, a light or dark spot appears on the surface of the tooth. There is no damage to the enamel structure - it remains smooth, pain does not bother you. At this time, it is easiest to cure caries, since it occurs with minimal intervention in the tooth tissue - the stain is removed from the surface, and the enamel is remineralized.
- Superficial caries. This stage involves damage, the focus of which is concentrated no deeper than the area of the tooth enamel. Characterized by periodic pain and reaction to hot and cold. Treatment follows the same scheme as at the initial stage.
- Average caries. The process has gone beyond the boundaries of the enamel and progresses in the area of superficial dentin, pain appears more intensely and more often. The treatment process involves cleaning the carious cavity and installing a filling.
- Deep caries. The tissue damage is very severe, the pulp is protected only by a thin layer of preserved dentin, and the patient experiences severe pain. If the filling is not installed in time, the disease can affect the pulp, and tooth extraction cannot be avoided.
Causes
Infection of the dental cavity can occur for the following reasons:
- Damage to the walls of the recess. Careless handling by a specialist leads to microtrauma. Remains of bone tissue enter the wound, causing infection.
- Failure to follow the dentist's recommendations. Blood clots are removed with solid food and constant rinsing.
- The slow transition of blood from a liquid state to a clot. The blood in the cavity coagulates, forming a protective layer. If the patient has problems with its clotting, the wound will not be protected.
- Weakened immunity. This condition increases the risk of developing inflammation. The immune system of a healthy patient easily copes with harmful bacteria. Therefore, surgery cannot be performed if a person is sick.
- Infection through instruments. Pathogenic microorganisms can enter an open wound from the outside.
Alveolitis in an advanced stage (photo)
The risk of developing infection is higher in people who have the following problems:
- gingivitis;
- periodontitis;
- caries;
- cyst;
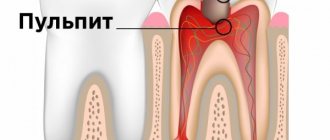
- pulpitis;
- inflammation of the tooth root (periodontitis);
- ARVI;
- flu;
- angina.
More often, inflammation of the cavity occurs in elderly patients and people with HIV infection and diseases of the endocrine system.
Sometimes the cause is a complicated operation, for example, after the removal of a wisdom tooth. It was revealed that the disease is more often observed in the lower jaw (in the area of the molars). This is explained by its special structure, which creates certain problems during tooth extraction.
General information
Doctors have repeatedly made attempts to create a single, universal system of classifications of human diseases.
As a result, in the 20th century the “International Classification - ICD” was developed. Since the creation of the unified system (in 1948), it has been constantly revised and supplemented with new information.
The final, 10th revision was carried out in 1989 (hence the name ICD-10). Already in 1994, the International Classification began to be used in countries that are members of the World Health Organization.
In the system, all diseases are divided into sections and marked with a special code. Diseases of the oral cavity, salivary glands and jaws K00-K14 belong to the section of diseases of the digestive system K00-K93. It describes all dental pathologies, not just caries.
K00-K14 includes the following list of pathologies related to dental lesions:
- Item K00. Problems with development and teething. Adentia, the presence of extra teeth, abnormalities in the appearance of teeth, mottling (fluorosis and other darkening of the enamel), disturbances in the formation of teeth, hereditary underdevelopment of teeth, problems with teething.
- Item K01. Impacted (sunk) teeth, i.e. changed position during eruption, in the presence or absence of an obstacle.
- Item K02. All types of caries. Enamel, dentin, cement. Suspended caries. Pulp exposure. Odontoclasia. Other types.
- Item K03. Various lesions of hard dental tissues. Abrasion, enamel grinding, erosion, granuloma, cement hyperplasia.
- Item K04. Damage to the pulp and periapical tissues. Pulpitis, pulp degeneration and gangrene, secondary dentin, periodontitis (acute and chronic apical), periapical abscess with and without cavity, various cysts.
- Item K06. Pathologies of the gums and the edge of the alveolar ridge. Recession and hypertrophy, trauma to the alveolar margin and gums, epulis, atrophic ridge, various granulomas.
- Item K07. Changes in bite and various jaw anomalies. Hyperplasia and hypopalsia, macrognathia and micrognathia of the upper and lower jaws, asymmetry, prognathia, retrognathia, all types of malocclusion, torsion, diastema, trema, displacement and rotation of teeth, transposition.
Incorrect jaw closure and acquired malocclusions. Diseases of the temporomandibular joint: looseness, clicking when opening the mouth, painful dysfunction of the TMJ.
- Item K08. Functional problems with the supporting apparatus and changes in the number of teeth due to exposure to external factors. Loss of teeth due to injury, extraction or disease. Atrophy of the alveolar ridge due to long-term absence of a tooth. Pathologies of the alveolar ridge.
Symptoms
In the first two days, the alveolitis of the tooth socket is almost invisible. Then he starts to progress.
The main symptoms of the pathology include:
- pain that gets worse when eating;
- swelling;
- redness of the gums;
- general malaise of the body;
- discharge of pus from the cavity;
- the presence of gray plaque in the alveoli.
Advanced pathology causes weakness and fatigue. The thermometer can show temperatures up to 38 degrees. The patient develops a bad odor from the oral cavity, the lymph nodes become inflamed sensitivity increases . Pain may radiate to the ear or temple. They intensify over time and shoot sharply into the cavity itself and gums.
Treatment
Treatment for alveolitis should begin at the first sign of infection. It is unacceptable to self-medicate.
Before seeing a doctor, you can reduce pain with the following medications:
- Ibuprofen;
- Ketonol;
- Nise;
- Tempalgin
- Sedalgin.
Before prescribing therapy, the doctor usually sends you for an x-ray . In the image you can see foreign elements or dental fragments.
Sometimes curettage of the cavity is performed to identify the root cause of inflammation.
Then the dentist performs anesthesia and performs the following manipulations:
- cleans the socket of the extracted tooth and washes out the pus using special solutions;
- applies local applications with antimicrobial drugs;
- rinses the mouth with antiseptics and washes out food particles using a syringe and needle;
- Remains of food or tooth root are removed with a surgical spoon;
- re-rinses the cavity;
- dries it using a sterile cotton swab;
- powdered with anesthetic powder;
- applies a gauze bandage with an antiseptic.
In the future, it is recommended to take baths with potassium permanganate and take vitamin complexes.
The doctor may prescribe drugs from the following groups:
- Antibiotics (Sumamed, Azitral, Amikacin, Norfloxacin).
- Anti-inflammatory (Voltaren, Ibuprofen, Nurofen, Ketorol).
- Antiseptics (solutions of Miramistin, Furacilin).
- Anesthetics (Lidocaine, Trimecaine).
Treatment with antibiotics and other types of drugs should be carried out only on the recommendation of a doctor. It is unacceptable to prescribe medications on your own.
The following methods are used as physiotherapy:
- microwave therapy;
- laser exposure;
- use of alternating current;
- UV irradiation.
Proper treatment can stop inflammation within a week. The wound is covered with a protective layer, and relief comes. After this, the patient must visit a specialist and follow all his recommendations.
Within a week and a half, the cavity is overgrown with granulation tissue, complete healing occurs after fourteen days, and the inflammation finally subsides.
To prevent alveolitis, doctors advise:
- do not squeeze or suck out blood clots;
- do not pick the damaged hole;
- do not chew food on the side where the operation was performed;
- give up cigarettes and alcohol immediately after the procedure;
- warn the doctor before surgery about poor blood clotting, taking aspirin and anticoagulants;
- Do not feel the area of the extracted tooth with your fingers.
On the day of the procedure, you should not be overcooled, and after it you should avoid contact with various types of infections. The surgeon can prevent the development of the pathological process if he performs the operation in accordance with all the rules, using antiseptic solutions.
Patients with diabetes mellitus and cancer should undergo treatment to prevent infection of the socket before removing a tooth.
It is possible to eliminate the manifestations of the inflammatory process at home only for a short time. on your own . Therefore, you will still have to contact a specialist who knows how to treat alveolitis after tooth extraction. Otherwise, it may lead to blood poisoning.