Traumatic stomatitis is a disease of the mucous membranes of the oral cavity caused by mechanical or chemical influence. This leads to the development of integrity of epithelial tissues and cells. Long-healing wounds, erosions and ulcers appear on the affected area. Treatment of such a pathology usually takes a long time, and if the provoking factors persist, constant relapses are possible. In the article we will look at why the disease occurs, effective methods and methods of treating traumatic stomatitis.
Definition of disease
In dentistry, traumatic stomatitis is understood as a single or regular impact of various nature on the mucous membranes of the oral cavity, which leads to the appearance of wounds, ulcers and erosions. Pain in the affected area, minor bleeding and increased tissue sensitivity are noted.
As the pathology develops, the injured area becomes covered with a white or gray coating.
Due to the violation of the integrity of the tissue structures of the oral cavity, the risk of infection with infectious diseases of various nature (viral, bacterial and fungal) increases. Bacteria actively accumulate in affected areas, which leads to halitosis - bad breath.
With a single damage to the mucous membranes, no symptoms of the disease are observed - the tissues are restored naturally. The most dangerous thing is regular mechanical or chemical exposure.
Etiology
Several reasons contribute to the occurrence of traumatic stomatitis. In general, they can all be divided into three types:
- chemical;
- mechanical;
- physical.
In childhood, the development of stomatitis is caused by damage to the tooth or tissue that occurs as a result of a blow or an unsuccessful fall during outdoor games. In newborn children, the disease occurs when the gums are damaged by an encroaching tooth.
In an adult, the factor that triggers the onset of the disease is a burn from drinking hot tea. In the case of constant consumption of hot food and drinks, the burn and, consequently, stomatitis become chronic. You can get this kind of injury not only from hot food.
The causes of traumatic stomatitis can be:
- medications that were not used in accordance with the instructions;
- chemicals;
- acids;
- fire;
- alkaline substances;
- electricity.
On this topic
- Stomatitis
Find out how long it takes for stomatitis to go away
- Maria Konstantinovna Tevs
- July 26, 2020
In addition, pathology can develop as a result of frostbite.
Mechanical factors include:
- poorly selected braces and dentures;
- hard plaque that was not removed in time.
Mechanical mucosal injuries also occur when:
- frequent consumption of unpeeled seeds ;
- the habit of putting sharp objects - cloves, needles and others;
- hasty eating , when the likelihood of biting the mucous membrane increases.
Another reason contributing to the development of the disease is the presence of a bad habit of biting the lips and the inside of the cheeks, which causes damage to the mucous membrane.
The above factors not only can permanently injure soft tissues, but they also lead to swelling, inflammation and the formation of ulcers.
Causes
The following causes of traumatic stomatitis are identified:
- friction of the mucous membrane on the sharp edge of the tooth , poor-quality braces or dentures;
- chemical or thermal burn (excessively cold or hot drinks, prolonged use of medications, work in hazardous working conditions);
- In children and some athletes, stomatitis occurs due to trauma to the oral cavity during play, for example, when being hit by a ball or landing on a hard object during play;
- In infants, the problem appears due to teething.
Some researchers separately consider bad habits that provoke the development of pathology. This includes frequent eating of sunflower seeds, biting the tongue and cheeks while working, and holding sharp objects in the mouth.
How to eat when the disease develops
To cure stomatitis of the traumatic variety, using only medicines or folk remedies is not enough. You will have to give up smoking and drinking alcohol, and also eat right.
First of all, it is necessary to exclude from the diet food and drinks with pronounced tastes: nothing spicy, salty, sour. Also, you should not eat too cold or hot foods, drinks, or solid foods. Food should not only be warm and soft, but also rich in vitamins, micro and macroelements.
If you have useful tips on a given topic, please share your experience with our readers in the comments.
Please like and share the article with your friends.
Kinds
To assess the pathology and choose a treatment method, it is important to determine the type of stomatitis. There are several classifications depending on certain factors. The form of the disease is determined by diagnostic procedures.
Depending on the nature of the lesion
This classification is based on the cause of the disease. The following types of traumatic stomatitis are distinguished:
- mechanical. Formed as a result of mechanical trauma. Everyone belongs to this type
Thermal damage is the most painful.damage to the mucosa due to poor quality prosthetics;
- chemical _ Damage occurs due to a chemical burn. Most often found in people working in hazardous production conditions, active smokers;
- thermal _ Stomatitis appears after a burn. Often occurs with regular consumption of excessively cold or hot drinks.
This classification is considered the main one for determining subsequent treatment, since thermal or chemical stomatitis require a different approach to the choice of remedies.
According to the nature of the flow
Depending on the degree and duration of the lesion, the following types are distinguished:
- Chronic . Occurs with regular traumatic effects on the mucous membrane. Difficult to treat.
- Subacute . At this stage, the wounds and ulcers are not yet fully formed, and the active process of infection begins.
- Spicy . Patients experience pain, redness and swelling of the mucous membrane. Possible increase in body temperature. More information about the treatment of chronic stomatitis here.
Traumatic stomatitis is characterized by a transition from one form to another in the absence of proper treatment.
Any stage of the disease is dangerous, so if characteristic signs are detected, you should consult a doctor promptly.
By localization
Depending on the severity of damage to the mucous membrane, diffuse traumatic stomatitis is distinguished - there are small ulcers, erosions or scars over the entire surface, as well as focal - the damage is represented by single wounds (stomatitis on the cheek, gums, lips). A long-term disease can turn into a necrotic form, when the death of cells and tissues begins; this is considered a serious complication, since the patient experiences intoxication of the body.
Prosthetic
It forms on the oral mucosa in those places where the prosthesis has a constant mechanical effect on the tissue. Pathology is observed when prosthetics are performed poorly or when care rules for removable structures are not followed.
Prevention plays an important role, since prosthetic stomatitis can be avoided by regularly applying special compounds and consulting a doctor if discomfort occurs.
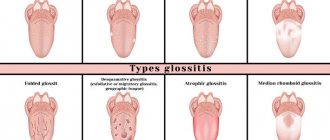
Types of disease
Traumatic stomatitis is classified according to a number of characteristics. According to the form of manifestation, the following varieties are distinguished:
- Hyperplastic type. In appearance, it is a plaque in the mouth in the form of a hardened yellowish crust. When it is removed, bleeding, hyperemic tissue is revealed. With the development of this pathology, dryness and burning are felt in the oral cavity.
- Catarrhal type. In this case, swelling and redness of the mucous membrane are noticeable, but ulcerations are not detected. When eating and talking, pain and unpleasant discomfort appear.
- Erosive stomatitis. It is characterized by the formation of an erythematous spot that is not covered with a film or plaque. Erosion has clear boundaries, but under the influence of various reasons they can grow and merge with each other.
- Ulcerative stomatitis. Its main feature is the appearance of single or multiple ulcerations. The ulcers may bleed and become covered with plaque.
- With frequent traumatic lesions, there is a risk of developing necrotizing stomatitis, in which epithelial cells die. In this case, the ulcers become covered with a yellow coating, and the mouth feels dry and burning.
- Separately, prosthetic stomatitis is distinguished, which develops as a result of damage to the mucous membrane by inserted elements.
According to the nature of the course of the disease, acute, subacute and chronic forms are distinguished. According to the degree of prevalence, the pathology can be focal (damage to certain areas of the oral cavity) or diffuse (spread to almost the entire surface).
Symptoms
With traumatic stomatitis, a small wound appears in the mouth, which causes severe discomfort and inconvenience to the person during conversation, while eating and in the morning. If the immune system is strong, the cells are restored naturally. With chronic exposure, the following symptoms appear:
- swelling and swelling of the mucous membrane at the site of the lesion;
- the wound turns red, burning and itching appears;
- sharp pain appears while eating or talking;
- articulation is impaired;
- a characteristic white or gray coating appears at the site of damage;
- in acute form, body temperature rises;
- salivation increases;
- There is an unpleasant smell of acid from the mouth.
Most stomatitis has similar symptoms, so one of the doctor’s main tasks is to correctly determine the type and source of the problem.
Characteristic symptoms
Unfortunately, the traumatic type of stomatitis manifests itself with the same symptoms that are inherent in other types of inflammatory ulcerative manifestations that develop in the oral cavity. Therefore, without knowing about the background of the pathology, making an accurate diagnosis is not so easy. Among the characteristic symptoms are the following:
- swelling appears precisely at the site of injury;
- the skin around the wound becomes bright red;
- painful sensations gradually increase;
- At the site of injury, both small ulcers and other types of erosive manifestations can form.
If the above symptoms manifest themselves, you should rush to the nearest dentist as quickly as possible. After all, only an experienced doctor can find out exactly what type of stomatitis is developing in a patient after a thorough examination of the patient and obtaining the results of the necessary tests. Next, the doctor will prescribe a comprehensive treatment therapy, individually selected for the patient, which will help avoid complications and prevent the development of relapses.
Treatment
When traumatic stomatitis is detected, complex treatment is prescribed, aimed at eliminating the provoking factor, strengthening immunity and cell regeneration. The choice of medication or health procedures should only be made by a doctor based on the diagnostic results.
The method and method of treatment directly depends on the form and stage of the disease. The optimal medications are selected, the cause and factors that caused the disease are eliminated. Below we present possible treatment strategies for traumatic stomatitis.
Elimination of the traumatic factor
It is the first priority during the treatment of the disease. A provoking or directly traumatic factor can cause complications, lead to relapse and development of the disease. The cause is determined during the collection of anamnesis, using laboratory and hardware diagnostics. Depending on the type, individual recommendations are selected and a recovery plan is developed.
Sometimes it is not possible to accurately determine the nature of stomatitis in a particular case. In such a situation, they can continue to undergo inpatient treatment in order to find out the main cause of the illness in a hospital setting.
Correction of orthodontic devices
Necessary if stomatitis was caused by poor-quality prosthesis or braces. It is necessary to remove the orthodontic device and its further correction.
Keep in mind that after the mucous membrane is restored, the braces will have to be put on again.
The most difficult situation is with braces, which are not always possible to remove. It is recommended to completely remove the braces until the mucous membrane is restored.
Anesthesia and neutralizer treatment
Procedures are necessary only in acute form or stomatitis was caused by a chemical substance. For example, in case of a burn with alkali, a weak acid solution is used as a neutralizer. The effect must be very rapid, since some compounds destroy mucosal tissue very quickly . Painkillers are used only when the patient has acute pain that cannot be tolerated, and also when surgical intervention is necessary.
Removing soft and hard deposits on teeth
If stomatitis was caused by dental diseases or a violation of their anatomical integrity, it is extremely important to eliminate the traumatic element, as well as to carry out complete sanitation of the oral cavity. For this purpose, both special grinding machines and chemicals are used.
Treatment of traumatic stomatitis
Treatment of this pathology must begin at the first warning signs. Drug therapy should be prescribed by a specialist after examining the patient. There are some distinctive features in the treatment of stomatitis in children and adults.
In any case, in case of chemical damage, before starting treatment, it is necessary to treat the affected area with a neutralizer. Otherwise, you can only worsen traumatic stomatitis. The neutralizer must be opposite to the irritant.
Dental procedures
If the cause of the damage is a tooth fragment, it must be treated. The specifics of treatment depend on the amount of damage, the condition of the tooth and root. In some cases, the tooth needs to be removed followed by prosthetics. For minor damage, sanding the chip is sufficient.
In case of traumatic stomatitis caused by tartar, it is necessary to have professional teeth cleaning to remove deposits.
If the damage is caused by new dentures, then you need to contact the specialist who installed them. He must adjust the shape and size of the structures. If the injury is associated with wear and tear of previously installed prostheses, then they need to be replaced.
General recommendations
Traumatic stomatitis can be cured only by eliminating its causes. It is also important to minimize irritation of the damaged area. To do this, you must follow the following recommendations:
- Eat food at an optimal comfortable temperature. You need to avoid food that is too hot or cold.
- Eliminate spicy, sour and salty foods from your diet. Avoid spices, garlic and raw onions.
- Eat soft food or pre-soften it.
- Avoid alcohol completely.
- Stop smoking.
- Take special care to maintain oral hygiene.
- Gently brush your teeth without touching the injured area.
- Taking vitamins. The bulk of them should come from food. Additionally, as prescribed by your doctor, you can take a multivitamin complex. This measure is necessary to increase resistance to infection.
How to cure traumatic stomatitis with medications
Therapy for traumatic stomatitis should be comprehensive. One of its components is rinsing. They are necessary for disinfecting the oral cavity. The following preparations can be used for rinsing:
- Chlorhexidine (0.05-1%);
- Furacilin (solution from tablets according to instructions);
- hydrogen peroxide (1 tbsp. 3% product in half a glass of water).
For rinsing, you can use herbal preparations such as Chlorophyllipt, Malavita, Rotokan, calendula tincture, propolis.
Treatment must include agents that eliminate the inflammatory process and prevent the spread of infection. For these purposes, they resort to the following means:
- Inhalipt (aerosol);
- Iodinol (solution);
- Lugol (solution);
- Miramistin (solution);
- Fukoricin (solution);
- Cholisal (gel).
Traumatic stomatitis is usually accompanied by painful sensations. Their intensity depends on the degree of damage, the patient’s susceptibility, and compliance with the doctor’s recommendations. In case of severe discomfort, resort to painkillers. This could be Kamistad or Lidochlor.
It is possible to use non-steroidal anti-inflammatory drugs. More often they resort to Ibuprofen and Nimesulide.
With the development of general toxic syndrome, antibiotics are required. To select a drug, it is necessary to determine the sensitivity of the pathogen.
You can speed up the healing of the affected area with the help of applications. For them, use sea buckthorn oil or an oil solution of vitamin A.
Medicines for children
The principles of treatment of traumatic stomatitis in children are similar to therapy in adults, but the list of possible medications is limited. In childhood, only local use of drugs is allowed. The following remedies are appropriate for children:
- Inhalipt;
- Miramistin;
- Lugol (from 5 years old);
- Fukortsin;
- Holisal.
The choice of drug is carried out individually. For young children who do not know how to rinse their mouths, only products in the form of aerosols, gels and solutions for irrigating the oral cavity are suitable.
To rinse traumatic stomatitis, you can use Furacilin, Chlorophyllipt, Rotokan, Malavit. The use of Chlorhexidine in young children should be avoided.
Children are allowed to take painkillers. Kamistad is allowed from 3 months, Lidochlor from one year.
For application you can use sea buckthorn oil.
On this resource you will find an article about the most effective medications for stomatitis.
Medication
This treatment is considered the most effective, since the drug can be selected depending on the severity of the case, age and condition of the patient’s oral cavity. Often several medications are used at once.
Painkillers
Taking them is necessary to eliminate painful sensations in the mouth, relieve itching and burning sensation. The painkiller is usually taken in the form of a spray, which is conveniently applied to the affected area. The most popular remedies are Lidocaine Asept, Hexoral-Tabs, Kamistad.
Antiseptics and antibiotics
Antiseptic agents are necessary for disinfecting wounds (hydrogen peroxide, Furacilin, Chlorhexidine for stomatitis). Antibiotics are needed to eliminate the inflammatory process caused by the activity of pathogenic bacteria. These are complex agents that have a broad effect (Amoxiclav, Tetracycline, Amosin and others).
Anti-inflammatory therapy
Taking these medications is necessary to relieve swelling, burning and redness caused by the inflammatory process. These are dental products for external use - Lugol, Cholisal for stomatitis, Rotokan, Hexalize.
Wound healing
A group of medications that are prescribed to speed up the healing process of tissue in the oral cavity. They often contain natural ingredients that have a mild effect.
The best healing drugs are Propolis spray, Solcoseryl, Karotolin, Olazol.
Disinfection and relief of inflammation
The next task of treatment is to disinfect the affected area of the oral mucosa. For this purpose, antiseptic drugs are prescribed: Miramistin, Triclosan, Chlorhexidine, Furacilin. At the mild stage of the disease, they are enough to suppress the infection.
Solution "Chlorhexdin"
If antiseptics do not cope with inflammation, anti-inflammatory drugs are additionally used: Dentinox, Metrogyl Denta, Sebidin, Tantum Verde, Cholisal.
If there are fungi in the oral cavity, it is necessary to take antifungal agents: “Candide”, “Pimafucin”, “Mikozon”.
If the disease is too advanced and has become severe with severe pain and large or multiple defects in the oral mucosa, the doctor prescribes courses of antibiotics. In the article “Use of Antibiotics for Stomatitis” we looked at the most effective drugs.
Home Remedies
Used for mild lesions. Traditional medicine is suitable for accelerating healing or enhancing the effect of traditional drugs. The following substances are used for this purpose:
- sea buckthorn oil for stomatitis . Rub the affected area with oil, the product enhances the healing process and reduces the risk of infection;
- propolis . It is best used as part of a rinse solution. Take 1 tbsp. spoon of propolis and fill it with 400 ml of warm water. The procedure is carried out for 3 days every 2-3 hours;
- Oak bark . Used as part of a medicinal decoction for rinsing the mouth. 2 teaspoons of bark need to be poured into 400 ml of water and boiled over low heat for 20 minutes, after which the product is filtered and cooled. The procedure must be carried out 4 times a day for 5 days. More information on how to rinse your mouth for stomatitis here.
Many doctors are against folk remedies because they are ineffective and can cause complications, such as allergies. You need to choose your prescription carefully; if side effects occur, you should completely abandon the drug.
Medical therapy
Therapeutic therapy for traumatic stomatitis depends on the cause that caused the development of the pathology:
- If the source of the pathology is a sharp object in the mouth, for example, a tooth fragment or tartar, the doctor will simply remove it.
- Children's therapeutic therapy is based on treating wounds with harmless antiseptic compounds, for example:
- infusion of regular chamomile or calendula;
- using furatsilin or hydrogen peroxide;
- using a decoction of plantain leaves for lotions.
- If the wounds in the oral cavity are more serious, the doctor will supplement the treatment with both antimicrobial and anti-inflammatory drugs:
- Hexaliz tablets are prescribed to children over 6 years of age;
- Rotokan for medicinal lotions and mouth rinses;
- Miramistin for spraying the medicinal composition over the entire surface of the oral cavity.
No less effectively, as indicated by reviews from numerous users, sea buckthorn infusion and rosehip oil help fight traumatic stomatitis.
In order to prevent serious complications, you should never put off visiting a dental clinic, because any disease, including traumatic stomatitis, is much easier to cure at the initial stage of development.
Possible complications
Traumatic stomatitis in children and adults can lead to serious complications if treatment is not started in time. Bacteria multiply at the site of the lesion, resulting in the development of chronic infectious diseases (Vincent's ulcerative necrotizing stomatitis, bacterial infection). The mucous membrane may become keratinized, erosions and severe ulcers appear on the inner surface of the cheeks and tongue.
The most severe consequence is tissue anesthesia due to prolonged traumatic exposure. It leads not only to the gradual death of tissues, but also to intoxication of the body.
Inaction as a cause of complications
If the traumatic type of stomatitis is not treated, the disease risks taking on a purulent form, which can lead to poisoning of the body. Or cause inflammation of neighboring tissues: gums, jaw bones, nasal mucosa, throat.
The longer the disease is left untreated, the weaker the immune system and the more active the pathogenic bacteria, microbes, and fungi. Gradually, these microorganisms and their metabolic products - toxins, begin to penetrate the circulatory system. Thus, they spread throughout the body, causing dangerous pathologies. The end result may be death.
Allergic stomatitis
According to a number of researchers, lesions of the oral mucosa in allergic diseases (see) occur in approximately 20% of cases. To the dentist. In practice, drug allergies are the most common, and the cut is characterized by a nonspecific allergic reaction to a given drug. The peculiarity of allergic S. is the variety of forms and variants of its clinical course.
Allergic S. can manifest itself in the form of catarrhal, hemorrhagic, vesicular-erosive, necrotic, as well as combined lesions localized in a limited area or on the entire oral mucosa. With allergies caused by various drugs, catarrhal and catarrhal hemorrhagic lesions more often occur. In this case, patients complain of a burning sensation, itching, dry mouth, and pain when eating. The mucous membrane of the mouth is swollen, hyperemic (color Fig. 16), atrophy of the papillae of the tongue may occur (the so-called varnished tongue). In the vesicular-erosive form of damage to the mucous membrane, blisters appear against the background of pronounced edema and hyperemia, after opening they form erosions covered with fibrinous plaque (print. Fig. 17).
The diagnosis is made on the basis of anamnesis and cytol data. research (detection of acantholytic or multinucleated cells). Blistering erosive lesions of the oral mucosa are differentiated from pemphigus (see), herpetic S., exudative erythema multiforme (see Erythema exudative multiforme). Ulcerative-necrotic lesions in case of drug intolerance are differentiated from ulcerative lesions in blood diseases (leukemia, agranulocytosis), Vincent's ulcerative-necrotic stomatitis.
Treatment involves eliminating the cause that caused the allergic condition and prescribing oral hyposensitizing and antihistamine drugs. In severe cases, sodium thiosulfate solution is administered intravenously; in a hospital setting, drip infusions of hemodez, polyglucone, isotonic sodium chloride solution, as well as corticosteroids are prescribed.
The prognosis depends on the timely elimination of the causes of the allergy.
Chronic recurrent aphthous stomatitis is an inflammatory disease believed to be of an infectious-allergic nature. It is characterized by the appearance of single painful aphthae (see) on the oral mucosa (tsvetn. Fig. 18), which heal after 7-10 days. Recurrent aphthae may be one of the symptoms of generalized aphthosis (see Behçet's disease). Relapses are more often observed in the spring-autumn period. Over time, the severity of the disease increases: the number of aphthae increases, and their healing period lengthens to 2-4 weeks, and relapses become more frequent. Sometimes there are no remissions at all.
The diagnosis is made on the basis of a characteristic wedge picture.
Treatment must be comprehensive and strictly individual. Specific (bacterial allergens) or nonspecific hyposensitizing therapy, sanitation of the oral cavity (particular attention is paid to the elimination of odontogenic foci of infection), local therapy (analgesic, antiseptic, epithelializing) are indicated.
The prognosis for systematic treatment is favorable.
Infectious stomatitis
To the most common information. diseases in which the oral mucosa is involved in the process include viral infections - lichen simplex, causing acute herpetic S., herpes zoster (see Herpes), influenza (see) and influenza-like diseases (for example, vesicular S.) , infectious mononucleosis (see Infectious mononucleosis), measles (see), foot and mouth disease (see), etc.; Vincent's ulcerative necrotizing stomatitis; bacterial infections - hyoid diseases, diphtheria (see), tuberculosis (see), leprosy (see); mycoses, for example, actinomycosis (see), candidiasis (see); sexually transmitted diseases, for example, gonorrhea (see), syphilis (see). If the lesion of the oral mucosa dominates in the wedge, the picture inf. illness, special treatment is required.
Acute herpetic stomatitis occurs mainly in children. Its occurrence is considered as a manifestation of primary infection of the oral cavity with the herpes simplex virus. There are mild, moderate and severe forms. The last two are accompanied by a pronounced disturbance in the patient’s condition, an increase in body temperature to 38-40°, acceleration of ROE to 20 mm/hour, and leukopenia. The mucous membrane of the mouth is swollen, hyperemic, with a large number of small vesicles, quickly turning into erosions covered with plaque (tsvetn. Fig. 14). Erosion is localized mainly on the mucous membrane of the palate, tongue, cheeks, lips, and in transitional folds. Diffuse gum disease is characterized by acute catarrhal gingivitis. Other mucous membranes may also be affected, primarily yellowish-kish. tract.
Differential diagnosis is carried out with other viral diseases (vesicular S., foot and mouth disease, etc.) using virusol. research methods (virus isolation, increase in titer of specific antibodies). Acute herpetic S. is also differentiated from allergic S.
When treating to strengthen the body's defenses, prodigiosan and lysozyme are administered intramuscularly; the oral cavity is treated with antiseptic solutions, proteolytic enzymes, and UV therapy is prescribed.
The prognosis is favorable. Prevention consists of carrying out anti-epidemic measures (isolation of sick people, monitoring the staff of children's institutions in order to identify patients with relapses of herpetic S.).
Vesicular stomatitis is caused by a virus from the family. Rhabdoviridae, which is transmitted to humans from domestic animals sick with this acute infection. illness. Infectious agents are transmitted through nutritional means, and in laboratory conditions - aerogenically.
In humans, vesicular S. occurs in the form of a flu-like infection and is accompanied by the appearance of vesicles on the oral mucosa. The incubation period is 1-5 days. Against the background of a sudden rise in temperature, symptoms of general intoxication develop (pain in joints, muscles, neuralgia, headache). After 2-3 days, vesicular rashes appear on the mucous membrane of the mouth and facial skin (cheeks, wings of the nose, upper lip), which persist for 10-12 days. At the same time, regional lymphadenitis develops.
Lab. Diagnosis is carried out by isolating the virus from nasopharyngeal swabs and the contents of vesicles. To make a retrospective diagnosis, serological methods are used. Differential diagnosis is carried out with foot and mouth disease (see), herpetic, aphthous S., as well as stomatitis that develops as a result of taking medications.
Treatment is symptomatic. Prevention of vesicular stomatitis consists of observing hygienic rules applied to prevent intestinal infections.
The prognosis is usually favorable.
Vincent's ulcerative-necrotic stomatitis (ulcerative stomatitis, ulcerative-membranous stomatitis, fusospirochetous stomatitis, ulcerative gangrenous stomatitis, Plaut-Vincent stomatitis, trench stomatitis) causes a symbiosis of a spindle-shaped bacterium (see) and a common spirochete of the oral cavity (fusospirochetosis). The occurrence of the disease is facilitated by a decrease in the overall resistance of the body, hypovitaminosis, etc. The disease usually affects young people. At the onset of the disease, body temperature rises to 37.5-38°, soreness and bleeding of the gums are noted, increased salivation and putrid breath appear. Catarrhal manifestations on the oral mucosa turn into an ulcerative process (gangrenous stomatitis), which most often begins from the gingival margin (print. Fig. 15) and spreads to other areas of the oral mucosa. When pathogens spread to the palatine tonsils, Simanovsky-Plaut-Vincent angina occurs (see Angina).
The diagnosis is established on the basis of anamnesis, wedge, manifestations, blood picture (slight leukocytosis, shift to the left, moderate acceleration of ROE), cytol results. examination of scrapings from the surface of ulcers (an abundance of spindle-shaped bacteria, spirochetes, destroyed leukocytes, structureless masses, erythrocytes). Differential diagnosis is often carried out with damage to the oral mucosa in leukemia (see).
In treatment, local effects are crucial: careful removal of dental plaque, treatment of the oral mucosa with antiseptic solutions, as well as oral administration of multivitamins.
The prognosis with timely treatment is favorable. Prevention involves maintaining oral hygiene.
Prevention
People with a predisposition to stomatitis should avoid any traumatic effects on the mucous membrane, including hot, hard or spicy foods. Do not use irritating mixtures or aggressive chemicals. If an injury has already occurred, it is necessary to prevent the spread of infection and the progression of inflammation. The damaged area should be treated with an antiseptic or suitable antibacterial agent.
Even under normal conditions, opportunistic microorganisms are present in the human mouth, which, when the immune system is weakened, begin to actively multiply and colonize the mucous membrane. The accumulation of pathogenic microflora can also occur due to poor personal hygiene. It is recommended to clean the oral cavity using all hygiene products: toothbrush, toothpaste, floss, mouthwash.
Forms
Any form of this disease is dangerous, since there is a risk of transition from one stage of the disease to another.
Depending on the duration of the course and the degree of damage, the following forms are distinguished:
- Spicy. The main sign of the acute form of the disease is the patient’s absence of symptoms of this disease in the past. The disease develops rapidly and passes in a short time. The main signs are redness of the oral mucosa, swelling, pain, and fever. After an acute illness, there is a risk of re-development of the disease. If you follow the specialist’s recommendations, treatment lasts no more than 2-10 days.
- Chronic. It is observed in people with weakened immune systems, as well as in the absence of treatment for acute stomatitis, which is difficult to treat. The pathology is accompanied by the following symptoms: redness of the mucous membrane, swelling of the soft tissues, pain, general weakness, fever, loss of appetite. The chronic form is very difficult to treat. To get rid of unpleasant symptoms, it is necessary to eliminate the cause of the disease.
- Subacute. This form is characterized by the formation of ulcers and the beginning of the infection process. In this case, there is a possibility that the disease will not develop into an acute form. This stage is accompanied by severe pain.