Definition, nature and specificity of gangrenous pulpitis
The pulp is a soft epithelium penetrated by capillaries and nerve vessels. There are a lot of nerve cells in the pulp. Therefore, toothache is the most difficult to endure. Consequently, pulpitis is an inflammation of that very soft tissue, the nerve. External irritants cause inflammation:
- infectious diseases;
- decreased immunity;
- jaw injuries;
- caries.
The position of the pulp, when the crown part of the tooth is completely destroyed, as a result of putrefactive decay of hard tissues, under the influence of pathological microflora of the oral cavity is called gangrenous pulpitis.
Gangrenous pulpitis on molars
This is an inflammatory process in the gums. Often a consequence of caries.
- With such a lesion, the tooth initially begins to change color, then an unpleasant odor appears.
- The process is accompanied by aching pain that intensifies after eating.
- The molars of the lower jaw suffer the most from the disease.
- Symptoms depend on the presence of an opening of the dental cavity. If there is no opening, then the fluid has nowhere to go, so pain appears and an exacerbation occurs.
- Most often, there is an opening, and there is an outflow of pus. In this case, the inflammatory process is painless. Instead, there is a pulling sensation that causes discomfort.
- Palpation of the soft tissue is painless; pain occurs only with a more detailed examination of the nerve or when food debris sticks to the carious gap.
The beginning of gangrenous pulpitis - hypertrophy of the pulp
Causes
The appearance of an inflammatory process in a chronic form is the result of the opening of the coronal part of the dental cavity and the beginning of the outflow of fluid into the cavity formed under the influence of caries. If the body shows a low level of reactivity, then the development of the disease occurs in a closed cavity, acting as an independently existing process.
The reason for the formation of this disease will be the low quality of caries treatment, in particular, the use of incorrect dental cavity treatment techniques or incorrect application of the lining.
How to diagnose
The manifestation of the disease can be in several variations. The most common of them are the following:
- pain that gets worse at night;
- echoes of painful sensations are also felt in neighboring teeth;
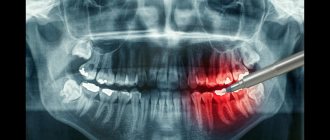
- X-rays clearly show small pathologies in the form of an increase in the gap between the dental crown and the gum, and slight tissue decay - an in-depth
- carious cavity;
- During a clinical examination, an incisor with a different color is detected, inside of which there is pus: touching the disintegrated particles does not cause pain, examination of the orifices causes suffering.
Initially, all the symptoms that the patient describes are studied. Based on the anamnesis and examination data, a diagnosis is made.
Tapping the causative tooth will not cause any pain. However, if gangrene has spread to most of the pulp and there is no outflow of purulent fluid, then mild pain may occur.
With prolonged manifestation of gangrenous pulpitis, a gradual intensification of pain will appear during probing. The tooth will practically not respond to a cold stimulus due to the death of a large fragment of the pulp.
If a chronic form of pulpitis is determined, it is necessary to conduct an additional differential examination. This procedure will help distinguish pulpitis from deep caries or damage to the upper part of the root.
Gangrenous pulpitis on an x-ray image
NeoStom – Dentistry website
1 visit:Complaints of pain in tooth 37 from cold, sweet foods, when food gets into a carious cavity, when the temperature changes. The pain continues for some time after the irritants are removed.
History: The tooth was previously treated for caries, the filling fell out a month ago and pain appeared.
Objectively: There is a deep carious cavity on the chewing surface of tooth 37, the tooth cavity has been opened. Probing the pulp is painful; the reaction to cold is painful and does not go away for a long time; percussion is painless. EDI 35 µA.
Diagnosis: Chronic simple pulpitis of tooth 37 (Pulpitis chronica simplex).
Treatment: Partial preparation of the carious cavity; arsenic paste is applied to the exposed pulp horn on a swab with eugenol under a bandage of dentin paste. Appointment in 2 days.
Student's signature_______________
Assistant's signature___________
2nd visit:
There are no complaints about pain in tooth 37.
History: Two days ago, treatment was started for chronic simple pulpitis of tooth 37, arsenic paste was applied.
Objectively: The bandage is preserved, percussion is painless.
Diagnosis: Chronic simple pulpitis of tooth 37.
Treatment: Removal of the bandage, preparation of the carious cavity, opening of the tooth cavity, amputation of the coronal pulp, expansion of the mouths of the root canals, extirpation of the root pulp (L of the distal canal - 20.8 mm, medial ones are passable at 2/3 of the length). Instrumental and medicinal treatment of the canals with 3% sodium hypochlorite solution and drying were carried out. The distal canal is sealed with eugedent with a gutta-percha pin, a tampon with cresodent is applied to the medial orifices, and a bandage of artificial dentin is applied for three days. X-ray control (description of the image indicating the quality of filling of the distal root canal; possible reasons explaining the obstruction of the medial canals - bending, obliteration, etc.; condition of the periapical tissues).
Student's signature__________________
Assistant's signature________________
3rd visit:
There are no complaints about pain in tooth 37.
Objectively: The bandage is preserved, percussion is painless.
Diagnosis: Chronic simple pulpitis of tooth 37.
Treatment: Removal of the bandage, filling of the traversed part of the medial canals with cresodent, lining with phosphate cement, filling with silidont.
Student's signature____________
Assistant's signature__________
4th visit: Grinding, polishing of the filling.
We recommend reading:
- Case history of chronic fibrous periodontitis
- Case history of acute apical periodontitis (exudation phase)
- Case history of acute apical periodontitis (intoxication phase)
- Case history of exacerbation of chronic pulpitis
- Case history of chronic gangrenous pulpitis
Related materials:
- Case history of acute purulent pulpitis
- Case history of acute general pulpitis
- Medical history acute partial
- Case history of hard tissue erosion
- Case history of wedge-shaped defect
Next >>
Consequences of chronic gangrenous pulpitis
When manifestations are repeated with some frequency, even after a course of treatment, the disease develops into a protracted form.
Chronic gangrenous pulpitis is differentiated with some serious problems.
- Chronic fibrous. Acute and aching pain for certain periods of time accompanies the problem. There is no pain at night; it appears when the tooth is exposed to an irritant. X-ray shows changes in the periodontal fissure.
- Acute deep caries. Acute pain had not previously been observed. Painful sensations appear, but not for long - the pain stops as soon as the irritant is removed. Changes are not visible on x-ray.
- Acute limited pulpitis. At first the pain appears during the day. A characteristic symptom is acute pain attacks, even at night. X-ray shows no changes.
- Pathological and anatomical examination of fibrous pulpitis reveals an increase in fibrous tissue. The pulp threads are thickened. Traces of hemorrhages that occurred previously appear. The composition of the pulp at the cellular level is dramatically changed.
The danger of gangrenous pulpitis is the death of gum tissue
In chronic hypertrophic pulpitis, a pathological and anatomical study reveals transformations of the pulp in all its constituent elements. Significant changes are noted in the vessels. There is a disruption in the functioning of blood vessels and lymph.
The chronic form of gangrenous pulpitis is a consequence of purulent or chronic fibrous pulpitis. This type of pulpitis is more often than others accompanied by unusual disorders of the apical periodontium. X-ray shows the expansion of the periodontal gap and its deformation.
Characteristic
At the moment when the acute stage of the inflammatory process passes, the immune system is activated in the body, which releases a huge number of leukocytes into the pulp. As a result, the pulp becomes swollen and its area increases rapidly. The formation of ichor occurs, which over time turns into purulent liquid.
Pus is dead white blood cells and bacteria. Thus, the metabolism in the pulp is inhibited, and it begins to die.
- Acute diffuse pulpitis is characterized by complete destruction of the soft tissue inside the tooth. This process causes severe toothaches, which echo in the ears, temples, eyes or back of the head.
- After anatomy of the bottom of the carious cavity, significant relief occurs as the accumulated pus comes out. Then an unpleasant odor appears from the mouth.
- The chronic form of fibrous pulpitis turns into gangrenous, after an exacerbation phase. The outflow of purulent fluid is disrupted and the bottom of the carious cavity becomes clogged with food debris. Then new foci begin to appear in the nervous tissue. Ultimately, this process becomes a chronic form of gangrenous pulpitis.
- When pus enters the pulp chamber, this leads to the disintegration of the nerve itself, and then to the death of the root part of the pulp.
- If there is an unhindered connection between the pulp chamber and the carious cavity, there will be no symptoms at all, only the color of the dental crown will change.
Read also: Tooth root rots, what to do
Possible complications
Flux is one of the possible complications.
Among the factors that provoke complications of the disease are lack of treatment or incorrect doctor’s prescriptions. When transforming into a more complex form, gangrenous pulpitis causes disorders in the body such as the formation of a flux cyst, neuralgia, and periodontitis.
The treatment regimen for each patient is selected individually, taking into account the advanced stage of the process and the presence of other health problems. You cannot delay going to the clinic if characteristic symptoms are detected, otherwise you may lose your tooth.
Treatment process under a microscope:
How to treat
Pulpitis does not always occur in an acute form and with severe pain. When the process has already gone far, heaviness and discomfort are felt.
The main goal of treatment is to eliminate the infection and decomposed dentin particles and lymphatic tissue.
Treatment regimen for gangrenous pulpitis
The main method of treating gangrenous pulpitis is cleaning the dental canals from dead dentin tissue. Vital extirpation in stages:
- anesthesia;
- isolation of the affected dental crown;
- removal of carious cavity, antiseptic treatment;
- opening of dental canals, treatment with antiseptics;
- assessment of the patency of the canals, their expansion, removal of nerve processes and dentin that has had time to decompose, treatment with antiseptic agents;
- a medicinal preparation is placed into the already cleaned and treated root canals, and a temporary filling is applied on top for five to seven days;
- after the allotted period, all temporary materials are removed - the affected areas are once again treated with an antiseptic, then sealed;
- restoration of the tooth crown, if necessary, production of an artificial crown.
If there is no treatment, complete decomposition occurs. Periodontitis begins to develop.
Treatment of pulpitis by pulp treatment
Ulcerative chronic pulpitis
Chronic ulcerative pulpitis progresses in the context of the development of acute or diffuse pulpitis. It can take from several months to a year or even two to form. It can lead to such consequences as periodontal inflammation and osteomyelitis of the jaw. A characteristic feature of ulcerative pulpitis is the appearance of ulcers on the pulp. In many cases, the pathological condition does not manifest itself at all.
When examining the oral cavity, a deep carious lesion is discovered in the causative tooth; at the bottom of the cavity there is already soft dentin with altered pigment. Probing opens the pulp chamber. Then the ulcer becomes visible, which is covered with necrotic plaque. With further probing, bleeding and pain appear.
The main goal during the treatment of ulcerative pulpitis is the elimination of all decomposed particles from the canals, elimination of infection, and further filling of the root canals with a filling substance.
Manifestation of the disease
Very often, this type of pulpitis does not have pronounced symptoms, so the patient does not immediately consult a doctor. However, there are also the following manifestations:
- a feeling of heaviness in the affected tooth;
- slight pain reaction when exposed to irritants;
- unpleasant (purulent) odor from the mouth;
- the presence of a carious cavity with soft dentin.
From time to time, the patient experiences spontaneous “shooting” pain, which intensifies in the evening and at night, and also spreads throughout the jaw.
Fibrous pulpitis can be accidentally discovered by a dentist during a routine examination of the oral cavity or on an x-ray.
Difference between gangrenous pulpitis
Gangrenous pulpitis is the final stage of development of the chronic manifestation of the disease. All this leads to complete destruction of the nerve. The crown above the causative site becomes dark in color, and a putrid odor appears from the oral cavity. X-ray shows deformation of the upper opening of the root system.
The form of gangrenous pulpitis for the most part has consequences - in the form of complications.
In children, chronic inflammation is asymptomatic. There may be two reasons.
- The structure of temporary teeth allows infections to easily penetrate from the pulp into the periodontium, and in the reverse order. This is due to the presence of a wide pulp chamber, as well as the lack of a formed root system of non-permanent teeth.
- The young body's susceptibility to colds. Most of them are caused by pathogenic microbes streptococci, which can cause inflammation of the periodontium, gums, and nerve endings.
Gangrenous pulpitis causes severe pain
The most common manifestations:
- increased sensitivity to temperature changes;
- however, warmer food causes pain, while cold food does not cause any sensation.
Ulcerative pulpitis can result from an acute form of pulpitis. When an abscess forms in the pulp.
Inflammation of the pulp in children
In children, chronic inflammation of the pulp can develop, bypassing the acute stage. This happens for two reasons.
- Features of the structure of children's teeth. They are distinguished by a wide pulp chamber, the absence of formed roots and a wide apical foramen through which infection easily penetrates from the periodontium into the tooth, and vice versa.
- The child's tendency to catch colds. Some of them are caused by pathogenic microorganisms - for example, streptococci, which can infect the periodontium, periodontal tissues, and with them the nervous system.
In such cases, infection of the neurovascular bundle occurs after another cold or tooth injury. The infection can spread to the crowns of adjacent baby teeth, as well as affect the rudiments of permanent teeth, which threatens the development of multiple caries.
Therefore, if you notice that your child has begun to react to cold and hot, complaining of aching pain and heaviness in the tooth, it’s time to take him to a pediatric dentist.
Prevention as an opportunity to prevent a problem
The most important factor is regular visits to the dental office. This needs to be done at least once a year. If you notice any symptoms, you should immediately consult a doctor. It is important to remember that advanced gangrenous pulpitis provokes the development of bone inflammation.
- It is necessary to treat caries in time in both children and adults. Caries tends to appear on one tooth and spread to adjacent tooth crowns.
- If you already have fillings in your mouth, then visits to the dentist should be made more than once a year. Filling materials also have their own expiration date. They can be destroyed by exposure to the oral environment and over time. Often microorganisms seep into the cracks between the tooth wall and the filling.
- Prevention of pulpitis is a computer examination of the oral cavity. Modern equipment will help identify violations in the most inaccessible places.
- If an injury to the jaw area occurs, you need to come for an examination, as microtraumas can lead to the appearance of caries. Damage to the enamel and chips can also lead to consequences such as pulpitis.
- An important factor is the preference for healthy food. Be sure to eat solid vegetables and fruits, such as carrots and apples.
- Careful and proper oral hygiene is the main preventive measure for any disease of the teeth and gums.
Recommendations after treatment
The only way to avoid relapse is to maintain proper oral hygiene and visit the dentist regularly. The appearance of pain in a tooth at rest or while eating is a good reason to visit a specialist, as this reflects an inflammatory process in the pulp. Professional cleaning of the oral cavity and visiting the dentist 2 times a year will help you prevent the recurrence of chronic pulpitis. If, after treatment from a specialist, you notice an acute reaction to cold and hot food, experience pain when pressing on your gums and teeth, or notice swelling and discoloration of the enamel, be sure to make an appointment with your doctor.
In the dental department of the CELT clinic, treatment of chronic forms of pulpitis is carried out using modern diagnostic equipment and high-quality filling materials.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
What happens to a tooth during acute pulpitis and why is it so dangerous to delay treatment?
Acute dental pulpitis is an inflammatory process in the soft tissues (pulp) of the tooth, characterized by acute pain.
This disease can occur in two forms: focal and diffuse. The disease in its focal form is also called serous due to the presence of serous exudate - a pathological fluid of inflammatory origin.
Acute pulpitis –
Signs of acute pulpitis are reduced to the appearance of acute, paroxysmal pain, spontaneous in nature (i.e., occurring spontaneously, without any irritants). As inflammation transitions from serous-focal to purulent-diffuse, the pain acquires a pulsating, shooting, tearing character, and pain-free intervals disappear until they disappear completely.
According to Platonov’s classification, acute pulpitis should be divided into focal and diffuse forms (Fig. 1-2). Acute focal pulpitis is characteristic of the very beginning of inflammation, when inflammatory changes are present only, for example, in the area of one pulp horn. The rest of the pulp is not yet engulfed in inflammation. Acute diffuse pulpitis - in this case, inflammation covers the entire pulp, both in the coronal part of the tooth and in the root canals (Fig. 2).
Focal and diffuse forms of acute pulpitis –
However, it should be noted here that this division does not have great clinical significance, and it is much more important to subdivide the acute form - not into focal and diffuse, but into acute serous and acute purulent forms. By the way, this is precisely the division proposed by the classification developed by WHO (World Health Organization) specialists.
Clinic, ICD 10 and classification of acute pulpitis
Code according to the international classification of diseases ICD-10: K04.0 Pulpitis
Important! The causative agents of the disease are various bacteria, including streptococci and staphylococci, which enter the soft tissue of the pulp through the carious cavity.
Symptoms, complaints, nature of pain
Acute tooth pulpitis has two forms of progression, which are characterized by pronounced symptoms.
Serous form
At the beginning of development, with the serous form of pulpitis, the patient complains of paroxysmal pulsating pain, which occurs both with and without impact on the tooth.
The attacks last for 10-30 minutes, the pain is localized clearly at the site of inflammation. This form of the disease lasts 1-2 days.
Diffuse form
With diffuse pulpitis, attacks intensify and become longer, the time interval between them is reduced. Pain occurs without affecting the source of inflammation. With further development of the disease, pain appears in the entire jaw, as well as in the head. The patient cannot independently determine the location of the inflammation.
Objective symptoms
- Caries on a diseased tooth has jagged edges that do not connect to the pulp chamber.
- On probing, pain appears at the point of localization of inflammation.
- When tapping there is no pain or electrical excitability .
Subjective symptoms
- Spontaneous, throbbing pain that gets worse at night.
- Often the pain is radiating and its source is difficult to determine without the help of a doctor. When the upper teeth , the pain radiates to the temples, teeth of the lower jaw, as well as to the cheekbones and brow ridges. When the lower teeth , the pain radiates to the back of the head, teeth of the upper jaw, ears, and the area under the jaw.
- A diseased tooth is characterized by increased sensitivity - pain occurs when touching cold or hot food.
- The patient experiences sleep disturbances, decreased appetite, and often increased body temperature.
Reference. Pain of a pulsating nature is caused by the pushing of exudate into the carious cavity.
Read also: Is it painful to treat?
Diagnostics
The initial form of pulpitis can be diagnosed with the help of a qualified specialist.
Photo 1. Patient at a dentist appointment. In case of acute toothache, it is necessary to visit a specialist to make a correct diagnosis.
At the slightest suspicion of the occurrence of this disease, the dentist is obliged to:
- Interview the patient. The specialist determines the nature and frequency of pain, the time of its occurrence, duration and radiation.
- Examine the oral cavity. The presence of caries, fillings, damage to teeth, and periodontal swelling is determined.
- Apply instrumental examination methods. The level of tooth destruction, the degree of caries development, and the condition of the pulp are determined.
- Apply radiography and electroodontodiagnostic methods. The image will help determine the condition of the pulp, and electroodontodiagnostics (EDD) will help determine the depth of the inflammation.
Differential diagnosis
If it was not possible to diagnose pulpitis using standard studies, you should turn to differential diagnostic methods, for example, laser Doppler flowmetry.
Differential diagnostic methods can identify acute pulpitis from papillitis, deep caries, acute diffuse and chronic pulpitis, periodontitis and neuritis of the ternary nerve.
Conservative treatment is used only at the initial stage of the disease and is aimed at preserving the integrity of the pulp.
In this case, the specialist removes necrotic dentin, the cavity of the affected tooth is opened, and treated with an antiseptic.
After this, the dentist applies a dentin-forming substance. After a few days , the tooth is filled, and the patient is recommended to undergo physiotherapeutic procedures.
Surgical treatment is used only when there is a high probability of infection of nearby tissues, as well as deep damage to the teeth and the transition of the acute focal form of the disease to purulent or diffuse. Surgical intervention involves the use of one or more methods of surgical resolution of the disease, including devital and vital amputation, pulpectomy and devital extirpation.
Treatment of fibrous pulpitis
As already mentioned, treatment of chronic fibrous pulpitis is carried out using surgical methods. It is aimed at eliminating the source of inflammation, preventing the spread of the disease and restoring the appearance and functionality of the tooth.
One of the methods of treating chronic fibrous pulpitis is vital extirpation, which is performed under local anesthesia. The procedure consists of several stages:
- removal of carious cavity tissues;
- carrying out treatment using antiseptic drugs;
- removal of pulp first from the coronal and then from the root part of the tooth;
- root canal filling;
- tooth filling.
All these manipulations require one visit to the dentist and are considered gentle and physiological. But if the patient has allergic reactions to local anesthetics or root canal obstruction, devital extirpation is required. It is carried out in two steps, in the first of which the pulp is opened and a special paste is applied to it, followed by the installation of a temporary filling. The second measures are carried out after 1–10 days and consist of removing dead pulp, filling canals and teeth. Experienced dentists at the CELT clinic treat fibrous pulpitis, achieving excellent results.
Exacerbation: chronic ulcerative pulpitis of the tooth
With untimely and poor quality treatment, acute pulpitis develops into chronic ulcerative pulpitis. In this case, a focus of necrosis forms in the pulp, which leads to partial or complete disintegration of the pulp.
With chronic ulcerative pulpitis, there are no spontaneous pain sensations; as a rule, they occur in response to the influence of one of the irritants.
The irritant can be hot or cold food, a sudden change in room temperature. The patient complains of bad breath, in the past - severe headaches, which suddenly decreased or completely disappeared.
Upon examination, the dentist observes a carious cavity with gray pulp. The pulp has an unpleasant, putrid odor, electrical excitability is reduced, and probing is quite painful.
Treatment of chronic ulcerative pulpitis is possible only after appropriate diagnosis. The main method of treating an ulcerative process is to completely remove the affected pulp, followed by cleaning the canals and then filling them with filling substances.
Clinical picture
Complaints
• Bad breath;
• Slowly increasing aching pain from hot heat that does not stop after the action of the irritant, a feeling of fullness in the tooth;
• May be asymptomatic;
• For discoloration (change in tooth color)
Anamnesis
Previously, spontaneous pain may be observed, which then decreased or completely disappeared.
Objectively:
Tooth color – enamel has a gray tint.
The condition of the gum mucosa is unchanged.
Probing reveals
• Deep carious cavity, with a wide open tooth cavity;
• Large amount of softened dentin;
• Painfully deep probing at the mouths of the canal (depending on the degree of development of the process).
Thermal diagnostics - pain occurs from hot heat, does not go away for a long time, pain slowly increases and gradually fades away.
X-ray shows a deep carious cavity, widely communicating with the tooth cavity. there may be changes in the periapical tissues in the form of widening of the periodontal fissure or even the formation of a focus of bone tissue destruction in the area of the root apex.
Prevention measures
Acute pulpitis is a serious disease that can lead not only to damage to the dentition and nearby tissues, but also to death. Pathogenic bacteria that develop during the acute form of the disease multiply in the affected tissues and spread through the blood throughout the body. The odontogenic infection that develops in this case often leads to death.
To exclude such diseases, you should adhere to preventive measures:
- Visit the dentist periodically (at least twice a year).
- Treat all dental pathological processes in a timely manner.
- Maintain oral hygiene.
- Regularly carry out professional teeth cleaning (removing tartar, strengthening enamel, etc.).
At the slightest suspicion of acute pulpitis, you should immediately contact a dental clinic for further treatment.
Gangrenous pulpitis
Gangrenous pulpitis is necrotization of the nerve endings of the tooth. This process is preceded by inflammation of the pulp, which manifests itself as a result of reactions to external stimuli. Most often, the disease is provoked by pathogenic bacteria that live in the oral cavity and the toxins produced by them. Pathogenic microflora first causes caries, and after perforation of the affected cavity, pulpitis develops. Less commonly, the infection develops as a secondary lesion, that is, bacteria enter the nerve endings of the tooth through periodontal pockets due to the presence of chronic diseases.
Gangrenous pulpitis is preceded by pathology in an acute form - diffuse or fibrous pulpitis. The disease in the acute stage is accompanied by more vivid symptoms than in the chronic form of the course. A person may experience severe throbbing pain, swelling of the soft tissues of the mouth, and inflammation of the lymph nodes.
The main reason for the development of the problem is the entry of pathogenic flora into the pulp chamber. This condition can be provoked by illiterate dental treatment. for example, if the doctor did not clean the canals well or did not install the filling material tightly. Another factor provoking pathology is increased abrasion of enamel. In the absence of timely action, destruction spreads to the dentin and then to the pulp.
A common cause of gangrenous pulpitis is too deep periodontal pockets. The disease occurs as a complication of periodontitis. Other causes of the problem include:
- Injury to enamel as a result of an accident or consumption of too hard foods (nuts, crackers). During accidents, not only the crown, but also the root of the tooth can be injured, including damage to its nerve endings.
- Infectious diseases of ENT organs. With these types of disease, the infection quickly spreads throughout the oral cavity. A factor favorable to the growth of bacteria in this case is the lack of oral care. Sinusitis, otitis, and tonsillitis can become the primary source of gangrenous pulpitis.
- Osteomyelitis or inflammation of the bone structures of the jaw. In this case, damage to several row elements on the upper or lower jaw is observed.
The pathology occurs in children much less frequently than in adults, but its treatment is a complex process. It is difficult for a child to sit quietly in a chair while the bur machine is running. Dental treatment for children is almost always accompanied by fear and tears.
Also, children cannot always describe the nature of the pain in the tooth. Advanced acute pulpitis causes the disease to progress to the chronic stage. As a result, the crown of the tooth is completely destroyed, and the baby’s body becomes vulnerable to pathogenic flora. Acute pulpitis is not always accompanied by severe pain; it all depends on the individual characteristics and sensitivity of the body. When examining small patients, significant carious cavities with partially or completely dead nerve endings may be detected. When probing the canals, the child usually experiences discomfort. In such cases, devital surgery is indicated.
Risk factors for the development of a chronic form of pathology:
- mechanical damage to the crown of the tooth, accompanied by a fracture or dislocation of its root;
- opening of the tooth chamber by the dentist during caries treatment;
- chronic diseases of the dental-jaw system;
- the presence of chronic infectious diseases of internal organs;
- periodontitis of neighboring elements.
Symptoms of the disease largely depend on the duration of pulpitis and the presence of anastomosis with the soft tissues of the mouth. Gangrenous pulpitis is visible to the dentist with the naked eye. In the chronic form of the pathology, patients experience moderate discomfort when biting off food. The tooth reacts sharply to temperature stimuli - cold and hot foods. When exposed to heat, pain can persist for a long period of time.
On palpation there is no pain in the tooth. Discomfort appears only with deep probing. If the root of the unit is also involved in the pathological process, then swelling and inflammation of the gums are noted, and a fistulous tract is also detected. If the disease lasts long enough, it may be accompanied by enlargement of the submandibular lymph nodes.
Read also: What is a pulped tooth?
Why is pulpitis accompanied by different symptoms in each patient? This is also due to the fact that not the same pathogenic bacteria are capable of causing caries. In addition, the patient’s immune status plays a role in the development of the disease. The stronger the body’s defenses, the more resistant it is to various pathological processes, including caries.
How does chronic pulpitis develop?
There are 5 possible “scenarios” for the development of this disease in its chronic form:
Fibrous
In this variant, the cells of the nerve and vascular bundles thicken and begin to degenerate. Patients feel heaviness in the jaw in the area of the tooth affected by pulpitis, and aching pain when the ambient temperature changes. As happens when leaving a warm room into the cold, or after taking a drink or food that is too cold or too hot.
Fibrous pulpitis is reversible. If medical care is sought on time, the neurovascular bundle can be restored.
At one time, dentist Gofung, giving a classification of chronic pulpitis, called it fibrous “simple”. This is something that practicing dentists around the world have been disagreeing with for decades. For such a name does not in any way reflect the essence of those painful changes occurring in the neurovascular bundle that passes through the pulp canals.
Ulcerative
Characterized by the formation of deep carious cavities penetrating deep into the tooth down to the pulp; an unpleasant aftertaste, which is associated with the active proliferation of pyogenic bacteria in the internal parts of the tooth. When you try to suck out leftover food from a tooth, an aching or shooting pain appears in its depths. Mycoulcers with a putrefactive coating appear on the part of the pulp that reaches the crowns.
Concrete
Develops in people over 45 years of age or in people with reduced strength of tooth enamel. Among the features of these forms of pulpitis, the presence of calcification salts is noted, forming microgrowths of irregular shape, serving as irritants to the bundle of vessels with nerves and causing their inflammation.
Hypertrophic
It mainly affects people under 30 years of age. Hypertrophy of the nerve conduction and vascular bundle, caused by inflammation in the acute stage, causes increased cell division of this bundle, which subsequently results in the formation of a polyp in the form of a growth inside the dental cavity.
Such a growth is detected during examination as grayish-pink tissue of the dental cavity. To avoid confusion between this polyp and a similar growth of the gingival papilla, it is necessary to carry out EDI (electroodontodiagnosis), that is, measure the level of resistance of the internal tissues of the tooth using microcurrents.
Gangrenous chronic pulpitis
The extreme, most unpleasant and even health-threatening stage of chronic pulpitis. There is complete destruction of the neurovascular bundle in the dental cavity, with darkening of dental tissues, visible even through the remaining intact enamel, and the smell of decomposed tissues from the mouth.
Radiography at this stage reveals plastic deformation of the apical opening of the root.
The gangrenous form is always fraught with complications such as:
- Acute periodontitis
- The appearance of a granuloma at the base of the tooth root.
Diagnostics
If you suspect pulpitis, you should immediately contact a specialist. You will not be able to cope with the disease on your own. The doctor must carry out differential diagnosis, which makes it possible to distinguish the gangrenous form of the disease from others. This study includes:
- Visual examination of the oral cavity. During the examination, the dentist reveals the depth of damage to the tooth, the size of the cavity and changes in the color of the enamel of the element.
- Percussion or tapping on the problematic element. The method is used to assess the sensitivity of a tooth to external stimuli. Sometimes during the examination, expansion of the periodontal fissure and destruction of the root of the unit are revealed.
- Thermometry. The procedure is carried out using a dental probe without the use of hot water. The base of the instrument is heated using a heating pad. The doctor touches not only the pulp, but also the tooth surface. If pain increases slowly, then we are talking about pulpitis in a chronic form. After the procedure, discomfort disappears for a long time, which indicates the accumulation of purulent exudate in the affected area. When the tooth is diseased, it usually does not respond to cold water and food.
- Electroodontodiagnostics. Using the method, the sensitivity of the pulp in its various states is determined. An electric current of varying intensity is supplied to the nerve endings of the tooth. Sensitivity in a healthy tooth appears when exposed to a current of up to 6 µA. With gangrenous pulpitis, the sensitivity of the pulp decreases to 60-90 μA.
- X-ray. Using the technique, the doctor reveals additional information about the affected element: an increase in the periodontal gap, the condition of the root system, alteration of the tooth tissue.
Diagnosis of chronic fibrous pulpitis
It is impossible to diagnose chronic fibrous pulpitis unless a set of certain research measures is carried out. The key feature of pulpitis in its chronic fibrous version can be considered the formation of a carious cavity filled with soft dentin affected by infection. This cavity has a direct connection with the pulp chamber and to identify it, the dentist uses probing using a sharp curved instrument. An indicator of such a message will be pulp bleeding and pain.
Another diagnostic method for determining pulpitis is thermometry, that is, exposure of the tooth to cold and hot irritants. In particular, the technique of applying cold water to the tooth using a syringe and a blunt needle is used. In this case, the pain is felt quite strongly and does not go away for a long time even after the irritating factor ceases.
However, the most reliable and certainly the most informative way to detect chronic pulpitis is electroodontodiagnosis. A healthy pulp demonstrates a response to minor current impacts, approximately 2-6 μA; any deviations indicate the presence of inflammation. Thus, fibrous pulpitis will be indicated by the response excitation of the pulp when exposed to a current of 35-50 μA. X-rays will also help identify the chronic form of pulpitis, thanks to which it is easy to detect a cavity affected by caries that communicates with the pulp chamber.
It is important to know: It is very easy to confuse the chronic form with the acute form, but it is still possible to identify the differences, first of all, through a careful study of the patient’s medical history. The fact is that he will have no complaints of acute pain, as well as pain radiating to the head, in the chronic form. The patient can tell the doctor that they once felt these pains, but over time they passed and only aching pain of a long-lasting nature remained.
Features of treatment
Treatment of gangrenous pulpitis is carried out by removing the nerve endings of the tooth. Otherwise, the pathological process may spread to healthy areas of the oral cavity and cause multiple loss of elements of the series.
The operation begins with the injection of an anesthetic drug into the soft tissue of the gums. The problem area is chipped from several sides. An adult is given about 3 injections to completely lose the sensitivity of the operation in that area. The dosage of the anesthetic is calculated individually, based on the patient’s body weight and state of health.
The patient waits about 15-25 minutes until the painkiller takes effect. In order for the medicine to act quickly and effectively, patients are asked to press the inside of the cheek and the area to be injected with their fist. After this, the patient should tilt his head back and take a comfortable position. The doctor asks the patient to open his mouth as wide as possible to provide better access to the problem area.
The dentist carries out the necessary manipulations in several stages:
- Using a drill and other instruments, the doctor opens the affected carious cavity. Dead tissue is completely removed, otherwise the pathology will appear again. Using the procedure, the specialist provides access to the soft tissues of the pulp.
- Cotton swabs are placed around the tooth and gums. Actions are necessary to ensure that saliva and blood do not interfere with dental work.
- Damaged nerve endings are removed using the pultoectomy method. The dentist uses special needles to remove nerve endings and clean out decay products. The patient needs to periodically spit out the saliva that has accumulated in the mouth. In complex cases, gangrenous pulpitis can be treated in several visits to the dentist.
- The cavity formed in the tooth is covered with a preparation that does not contain arsenic. A temporary filling is placed on top.
A repeat visit to the doctor is required after 2-3 days. At this stage of the intervention, anesthesia is not used, since the tooth is deprived of sensitivity. The remains of the nerve endings die under the filling under the influence of the drug.
The specialist removes the temporary material and re-cleanses the canals. He places a permanent filling deep into the canals, leaving no empty spaces.
After this, the therapy is completed. The dentist gives the patient recommendations regarding behavior in the postoperative period. After treatment, it is forbidden to eat for 2-3 hours. It is not recommended to consume coloring foods and drinks for 2-3 weeks.
Chronic gangrenous disease in the acute stage is treated according to the above scheme. Dental pulp removal is contraindicated in patients suffering from sudden increases in blood pressure, tuberculosis and hemophilia.
Treatment of illness in children
Chronic gangrenous pulpitis in children is treated in the same way as in adults. Doctors perform a complete cleaning of the carious cavity, disinfect the canals with special preparations, and fill the tooth. Adjustments may be made to the treatment regimen due to the structural features of the elements in children.
For children, drugs containing arsenic are usually used, which quickly kill nerve endings. It is difficult for children to calmly tolerate the injection of anesthetics into problem areas. The doctor chooses the appropriate method of therapy depending on the age and behavior of the child, the structural features of the problem unit and the level of equipment of the clinic.
Therapy for gangrenous pulpitis is carried out in two ways - using devital and vital amputation. In the first case, the gangrenous cavity is completely cleaned out using anesthetic drugs. In the second case, mummification of the affected nerve endings occurs after they are killed.
The product contains all the necessary components for mummification of the nerve endings of the tooth. This method allows you to preserve the milk element until it is replaced by a permanent tooth. In addition, dental paste prevents relapse of exacerbation of gangrenous pulpitis.
Treatment of fibrous form of pulpitis in children
Fibrous pulpitis, unfortunately, can occur even on baby teeth in the youngest patients. Treatment in this case depends on three factors:
- experience and qualifications of a pediatric dentist;
- clinical picture of a particular case;
- capabilities of the dental clinic.
To treat pulpitis on baby teeth with fully formed roots, dentists use a medical approach similar to that used in adults. However, children are very timid and cannot always ensure complete immobility during treatment, therefore, as a rule, preliminary devitalization of the dental nerve is used. The prepared pulp is removed at the next visit.
Attention! In the practice of pediatric dentists, arsenic-free paste, for example Devit-S, is most often used for devitalization. This is a potent drug based on paraformaldehyde, which has an effect on the pulp comparable to arsenic.
Before applying the paste, the dentist opens access to the pulp chamber. The paste is placed into the chamber in a small amount, about 2 mm of substance. In some cases, on multi-rooted teeth, the amount of paste used can be increased. The exposure time of the drug on pulp tissue is usually from 3 to 7 days.
Devitalization - used in dentistry for partial removal of dental pulp, can be mechanical or chemical. During chemical devitalization, the tooth pulp is dissolved as a result of the use of a specialized paste, which allows root canal treatment to begin.
Unfortunately, some pediatric dentists tend to choose treatment methods that are more convenient for them, without thinking about the patient's future prospects. Treatment of pulpitis in a child is complicated by the characteristics of child behavior. It is difficult for children to sit in the dentist's chair and endure unpleasant sensations motionless, obediently following the doctor's commands. Therefore, some dentists use devital amputation methods, in which, after killing the nerve, the coronal pulp is removed and the root part is left intact. The dead part of the nerve becomes mummified and remains in the tooth. This manipulation speeds up the treatment process and makes it less labor-intensive for the dentist. However, a dead nerve often becomes a source of chronic inflammation in dental tissues, leading to the formation of gingival fistulas and tooth root cysts. These processes can have a negative impact on the rudiments of the child’s future permanent teeth.
Prognosis for recovery
The success of recovery from pathology largely depends on the competent actions of the doctor. If the dentist performed poor-quality cleaning of the canals or left particles of inflamed nerve endings, the tooth will have to be removed in the future. Much depends on the patient’s actions in the postoperative period and his ability to follow the doctor’s recommendations.
Treatment will be successful if gangrenous ulcerative pulpitis is detected in time. For this reason, you need to undergo a routine examination with a dentist at least 2 times a year. For problematic units, the time interval is reduced to 1 time per trimester.