A radicular cyst of the upper jaw is a cavity formation in the area of the apex of the tooth root, lined from the inside with epithelial tissue and filled with a special cystic fluid. Represents the end of periapical chronic inflammation. A person with a radicular cyst of the jaw (ICD 10 K09) sometimes does not feel anything, does not complain about anything, inconvenience occurs when it grows into the maxillary sinus or when the contents suppurate. The prolonged existence of a cyst causes deformation of the bone tissue and increases the likelihood of a jaw fracture. Treatment is carried out mainly surgically.
Description of the disease
A radicular or radicular cyst of the upper jaw is a liquid formation with fibrous walls that forms in the apical region of the dental root and limits the focus of inflammation from healthy periodontal tissues. This is the most common type of cystic jaw pathology - it occurs in 95% of patients. Cysts of the dental roots of the upper jaw are more common when compared with the lower jaw. Both women and men are equally susceptible to the appearance of formations, usually between the ages of twenty and forty-five years. Radicular cysts of the upper jaw can be more than five centimeters in diameter. A root cyst is formed from epithelial cells under the influence of inflammation in periodontal tissues. It has thin fibrous surfaces, is lined on the inside with flat stratified epithelium, and is filled with a clear yellow liquid with cholesterol crystals. The formation appears either directly on the upper part of the dental root (the so-called apical cyst), or on the lateral root surface and is then referred to as a periodontal lateral cyst.
Why does a cyst form? Causes
The main reason for the formation of a radicular cyst of the upper jaw is the presence of an inflammation process, as a result of which a connective tissue capsule appears in the body, isolating the infectious focus. Mostly cysts are formed in people with long-term caries, periodontitis, pulpitis, or as a result of incompetent dental intervention. Among the most common precursor diseases of cysts is granulomatous periodontitis - an inflammatory chronic periodontal pathology with the formation of specific connective tissue granulomas, which gradually grow and turn into cysts. The cause of an infectious lesion is often a dental injury, an infectious disease suffered by a person: sinusitis, otitis media or tonsillitis, or deterioration of the immune system. Also, the cystic process can be accompanied by an incorrect bite and difficult teething of figure eights.
Possible complications
If acute inflammation does not stop in time, the capsule melts with pus breaking into the surrounding fibers. In this case, a reverse process is observed, called adenophlegmon. Localization in the cervical region is accompanied by a rapid course with rapid spread of pus through the interphase spaces. Breakthrough of exudate into other anatomical areas (organs, cavities) leads to the formation of fistulas, abscesses and mediastinitis. The infection can reach the venous vessels (thrombophlebitis) or enter the bloodstream with the development of septicopyemia.
Symptoms
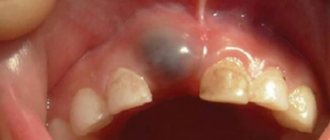
A radicular cyst of the maxilla (ICD 10 K09) can occur completely without symptoms for a long time or be accompanied by signs that are insignificant for the patient, and therefore they are often simply ignored. During the examination, the dentist will notice darkening of the tooth (the inflamed tooth may be under the crown, in which case it is much lighter than the tooth itself) or a carious process in an advanced state. Probing the root canals does not cause pain and is accompanied by the release of a yellowish fluid. As a rule, percussion does not often cause discomfort. If the cyst is large, there may be displacement of adjacent teeth, deformation of the alveolar process; palpation in this area is accompanied by the sign of “parchment crunching” and a feeling of pliability of the surface under the dentist’s fingers. Facial deformation of people with a radicular cyst is observed in 36.4 percent of cases. Due to the growth of the formation, bone tissue is destroyed, as a result, the likelihood of a jaw fracture increases.
Symptoms are much more pronounced if there is cystic suppuration. This phenomenon can be triggered by a blow to the tooth or maxillofacial trauma, sinusitis, unsuccessful dental intervention, etc. Inflammation begins from the cystic wall, the infected contents transform into pus. There are complaints of pain in the area of the causative tooth, signs of intoxication (chills, malaise, fever). An objective examination reveals swelling of adjacent tissues and hyperemia.
The lack of competent medical care in this case leads to significant complications, for example, soft tissue phlegmon, fistula, and maxillary osteomyelitis. The infectious process can spread to the paranasal sinuses and inner ear, which results in the formation of inflammatory pathologies of the ENT organs. Also in dentistry, the phenomenon of cystic growth into the maxillary sinus is encountered. Because of this, the walls are seriously deformed, the spongy bone substance atrophies, and the patient develops sinusitis.
The main sources of infection in the buccal area
- Odontogenic – from focal damage to the dentition, inflammatory gum disease, the formation of an abscess after extraction of elements.
- Non-odontogenic, associated with injuries to the mucous membranes of the oral cavity, cheeks or damage to the facial skin by external factors.
Dental pathology includes:
- cheilitis;
- periodontitis;
- carious lesions of varying severity;
- gingivitis;
- an abscess after the removal of a wisdom tooth on the cheek often occurs due to the high risk of damage to the mucous membrane due to the difficult-to-reach location of the elements;
- periodontal disease;
- failure to comply with daily hygiene rules;
- stomatitis;
- eruption of fangs outwards.
READ ALSO: What to do to make the flux break through faster: tips and recipes
Non-dental reasons for the development of an abscess localized on the cheek:
- injury to the gums with a sharp object - fork, knife, toothpick;
- scratches, deep cuts to the face;
- formations with hematogenous or lymphogenous spread; when the abscess is located in the jaw area, local inflammation of the nearby tissue of the cheeks is possible;
- disease of the ENT organs of bacterial etiology - tonsillitis, otitis media, adenoiditis;
- retropharyngeal boil;
- formation may occur when an abscess of the tongue appears with a history of strong immunosuppression;
- osteomyelitis provokes the spread of infected exudate, an abscess forms on the inside of the cheek;
An examination to find the cause, diagnosis, differential diagnosis, and prescription of a treatment regimen is carried out by a dentist, otolaryngologist, or maxillofacial surgeon.
Diagnostic methods
Dental radiography is becoming the most reliable diagnostic method. A radicular cyst is often discovered accidentally during treatment of other teeth. Such a formation appears on an x-ray as an oval or round shadow with clearly visible boundaries, located at the apex of the tooth root or near the lateral root wall. The bone structure of the periodontal fissure is not visualized on the image because it is destroyed. The roots of adjacent teeth are displaced. Sometimes a cyst cannot be identified even with the help of an x-ray, since the root of the diseased tooth is not sufficiently visible. To clarify the diagnosis, the method of electroodontometry is used. In the causative tooth, the excitability threshold varies within 100-120 μA, that is, it indicates pulp necrosis.
To determine whether the cystic formation is malignant, a puncture is made with a thick needle. The contents of a radicular non-festering cyst are yellow liquid containing cholesterol grains. To exclude the growth of the formation into the cavity of the nasal paranasal sinuses, it is necessary to additionally perform radiography of the latter. Radiological symptoms of a cyst are deformation of the bottom of the sinus bone and a dome-shaped protrusion. In doubtful situations, it is advisable to perform a computed tomography or contrast radiography of the upper jaw bone.
Differential diagnosis of this type of cyst is carried out with other jaw cystic formations and tumors (osteoblastoclastoma and ameloblastoma). In the case of a follicular cyst, there is no connection between the disease and the process of inflammation in the causative tooth; radiography reveals the crown of the permanent tooth in the cystic cavity. The examination of the dental arch reflects the absence of a permanent tooth or the presence of a baby tooth in its place. Follicular cysts are most often found in children and young people. Incisor canal cysts form exactly in the midline area of the hard palate, behind the central upper incisors. In the area of the nasolabial beard under the base of the nasal wing there are nasolabial cysts, in the space between the maxillary canine and the lateral incisor there are globulomaxillary cysts.
Ameloblastoma is typically located in the area of the body and angle of the lower jaw; its development is not associated with inflammatory periodontal pathologies. On X-ray analysis, the tumor looks like a polycystic formation with an unerupted figure eight inside or a single-chamber cyst. To clarify the diagnosis, a puncture is required, as well as a cytological analysis of the obtained material. The difference between osteoblastoclastoma and radicular cyst is the less clear boundaries and cellular structure on the x-ray. The roots of the teeth, getting into the tumor area, are most often resorbed. If a puncture is performed, a little brown liquid without cholesterol impurities is obtained.
Forms
Depending on the course, acute and chronic periostitis of the lower jaw is distinguished.
According to the type of exudate, the first option can be serous and purulent.
The chronic form is divided into:
- simple;
- ossifying;
- fibrous.
The acute form is characterized by:
- fast development;
- clear clinical picture;
- copious exudation.
In this course, inflammation progresses in a short period of time, fluid secretion increases, that is, a serous effusion is formed. If the process develops further, then dead cells accumulate in it. The protein level rises and the exudate becomes purulent.
Acute odontogenic purulent periostitis
A simple form of chronicity occurs when treatment of acute periostitis was started late. The process becomes moderate, and clinical manifestations subside.
With ossifying chronic inflammation, the periosteum thickens and hardens, and bone formations form under it. Due to this, the thickness of the lower jaw in the area of inflammation increases, which leads to its deformation. Fibrous periostitis is characterized by the proliferation of connective tissue.
Ossifying chronic and fibrous forms in most cases require surgical treatment.
Conservative treatment of radicular cyst of the upper jaw
Treatment of an altered cystic tooth root requires cleaning and disinfection of the tooth and filling. Another alternative treatment method is the introduction of a healing suspension containing calcium and honey, followed by the impact of small electrical discharges on the tooth. The main indications for drug therapy are: poor filling in the root canals (not along the entire length); absence of fillings on the root canals; the size of the cyst barely reaches eight millimeters.
When treating radicular cysts of the jaws, special agents are used that negatively affect the cystic capsule and its contents. Then the purulent exudate is completely removed, and instead of it, dental paste is injected into the cystic cavity, restoring the bone structure. The manipulations end with filling the crown and canal. Relapses of the disease are possible. What operations are performed for radicular cyst of the upper jaw?
Surgery
There are two methods of surgical treatment of this pathology: cystectomy and cystotomy. During cystotomy, the specialist makes a hole so that the cystic cavity communicates with the external environment, thereby reducing the hydrostatic pressure inside the formation after the outflow of fluid into the oral, nasal cavity or paranasal sinus. Such an intervention to remove a radicular cyst of the upper jaw is desirable for large formations that destroy the surface of the maxillary sinus and touch several tooth roots, without having radiological symptoms of an increase in the periodontal gap, and extensive mandibular cysts that thin the jaw bone tissue. The operation is performed under local anesthesia as follows: the doctor cuts out a mucoperiosteal semi-oval flap in the area of cystic formation, exposes the bone wall and performs trepanation, then the cystic cavity is washed and filled with a tampon with iodoform. In order to prevent the disease from returning during the procedure, it is advisable to carefully check the tissue and eliminate areas with necrosis. After a week, the tampon is changed, and subsequently the bandage is changed 3-4 times. This operation for a radicular cyst of the upper jaw is well tolerated by patients, but is accompanied by a long existence of the defect after the operation.
During cystectomy, the cyst is completely removed by separating the fibrous membrane of the formation from the adjacent tissues. Then a cavity tamponade is performed or the edges of the mucous membrane damaged during the procedure are brought together. Such manipulation is desirable for people with small cysts or large formations in places where teeth are missing, if a fairly thick layer of bone tissue is preserved. In some cases, surgeons consider it correct to combine both surgical procedures to remove a radicular cyst of the upper jaw.
Due to the absence of obvious clinical signs, the disease is diagnosed late, when its course is usually complicated by deformation of the anatomical structure of the oral cavity or the addition of an infection. To identify a radicular cyst in a timely manner, you need to constantly visit the dentist. Preventive measures include ensuring oral health and quality treatment of various diseases, such as periodontitis, pulpitis and caries.
For a radicular cyst of the upper jaw, how long does healing take?
Causes of cheek abscess and disease code according to ICD -10
The main provoking factor in the formation of pus is the addition of an infection, which, with the progression of the disease, in the absence of treatment and weak immune defense, leads to the melting of tissues with necrotic contents inside.
An abscess develops against the background of provoking factors:
- in case of disruption of the protective barrier of the mucous membrane, weakening of local or general immunity;
- infection in the cheek area spreads from foci of chronic infection - tonsillitis, adenoiditis, with the appearance of stomatitis with white aphthae widespread in the oral cavity, with the formation of injuries - if you bite the mucous membrane until it bleeds, damage the gums with cutlery.
An abscess of the buccal area is classified according to ICD-10 as a purulent skin lesion, boil or carbuncle of the face - code L02.0.
Rehabilitation and healing time
Removal of a cyst is always followed by a period of rehabilitation, during which restorative treatment is used. To speed up the tissue regeneration process, a special drug is injected into the cavity that remains from the eliminated cyst. A noticeable recovery is observed approximately six months after the intervention.
Complications with a radicular cyst of the upper jaw cannot be excluded.
What kind of disease is this?
Periostitis is the development of an inflammatory process in the periosteum.
In most cases, the disease is acute (95%) and rarely chronic (5%). Of all inflammatory diseases of the jaw, this pathology is detected in 5-6% of patients. This is what periostitis looks like on the upper jaw (photo)
Popularly, due to the development of edema on the face, dental periostitis is often called gumboil . This term came into use by Russian people from Germany; translated it means “movement, flow.” These words well reflect the mechanism of development of the disease; infection of the jaw usually occurs due to the ingress of microbes localized in diseased teeth ( carious or pulpitis) or gums (with periodontitis).
It is impossible to delay the treatment of gumboil; it develops rapidly and can cause serious complications:
- abscess (formation of large accumulations of purulent exudate in the cavities and its breakthrough outward);
- dissection of the periosteum;
- phlegmon (damage to subcutaneous tissue);
- impregnation of bone and soft tissues with pus and their death (necrosis);
- spread of the process to nearby organs (eyes, ears, brain, neck);
- general blood infection (sepsis).
Prognosis and consequences of jaw cysts, complications
If the formation is small in the early stages, the prognosis is positive. In such cases, dentists most often manage to eliminate the benign cyst and save the tooth.
With a significant size of the cystic cavity, the prognosis becomes satisfactory. Patients will have to lose one or even several teeth.
The negative consequences of jaw cysts are associated with disruption of the walls of the maxillary and nasal sinuses, the appearance of spontaneous jaw fractures, purulent lesions of the bone and periosteum, and sudden bleeding. The success of surgical intervention for follicular and radicular cysts largely depends on the time of diagnosis and the radical intervention performed at the right time.
Reviews about surgery for radicular cyst of the upper jaw
Patients say that in rare cases it is possible to do without surgical treatment. If you follow all the doctor’s recommendations, you can get rid of the pathology and restore your health.
Reviews about the operations are mostly positive. Complications very rarely occur after surgery.
People report that during the rehabilitation period they should carefully monitor the condition of the oral cavity, use antiseptic rinses and carry out all hygiene procedures efficiently. If there are signs of intoxication and the temperature rises, you need to urgently go to a dental surgeon.
Characteristic local signs of abscesses and phlegmon of the buccal area
The clinical picture of the development of an abscess differs in symptoms:
- increasing pain intensifies when chewing food or trying to open the mouth;
- purulent infiltrate creates a visual effect of facial asymmetry and swelling on the affected side;
- sensation of pulsation in the affected cheek;
- the skin above the abscess may be red, hot to the touch, stretched, upon palpation with cavity fluctuation, irradiation, pain occurs in the ears, eyes, neck;
- as the abscess progresses, there is a limitation in mouth opening;
- numbness of the surface of the lips is often observed during the extraction of wisdom teeth;
- increase in general body temperature to 39 degrees Celsius;
- a dense formation can be felt from the outside;
- the abscess provokes swelling of the lower eyelid and nasolabial folds;
- as inflammation spreads, an increase in the submandibular lymph nodes is noted;
- in a severe stage of pathology on the cheek, the voice changes, the patient finds it difficult to talk and move his tongue;
- features of the lesion - weakness, malaise, lack of appetite, headaches with an abscess.
READ ALSO: Pimples on the genitals: what causes them and how to treat them
Timely identification of symptoms and contacting a specialized clinic will help to quickly and effectively get rid of the problem, preventing the development of negative consequences for human health.
Prevention of the disease
There are no specific measures to guarantee the possibility of eliminating the possibility of a radicular cyst of the upper jaw (ICD K09). Prevention is based on regular oral hygiene, timely treatment of caries and various complications, and numerous infectious diseases. It is necessary to regularly clean plaque from the teeth so that it does not harden and transform into tartar.
It is very important to visit the dentist at least once a year for a preventive examination, which will prevent the occurrence of various oral pathologies.