Causes of toothache
The main causes of toothache are caries, pulpitis and other inflammatory processes, as well as the growth of wisdom teeth.
The most common cause of toothache is caries; it starts with a small spot on the tooth and can destroy the tooth completely.
The appearance of caries is caused by pathogenic bacteria that live on the teeth and feed on food debris. The product of their vital activity is acid, which gradually destroys tooth enamel. A hole appears, which increases in size and begins to hurt. When the destruction process reaches the nerve, the pain becomes very severe.
Important! Pulpitis is an inflammation of the soft tissue of the tooth (pulp). Advanced caries leads to this disease. Bacteria penetrating through the carious cavity infect the pulp and cause inflammation. Pulpitis causes severe pain and requires immediate treatment.
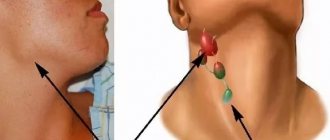
Inflammatory processes sometimes affect even those teeth in which the nerves have already been removed. When this happens, a person may feel pain not in the problem tooth, but in the entire oral cavity. Sometimes it can even be difficult to determine where exactly the unpleasant sensations come from. Another common cause of toothache is the eruption of third molars – wisdom teeth. They are considered the most problematic teeth, since their eruption and growth are rarely without difficulties. This process is often accompanied not only by unpleasant sensations in the mouth, but also by fever, weakness, enlarged lymph nodes, and headache. All organs of the human body are interconnected, so a disease or injury to one of them often causes pain in neighboring ones. The same applies to teeth.
Causes of wisdom tooth pain
If the direction of growth of a molar is incorrect (dystopic position), it grows at an angle, horizontally, which damages neighboring teeth and the cheek. Various options for the horizontal internal arrangement of the molar rudiment can be seen in the photo accompanying the article.
READ IN DETAIL: what to do if a wisdom tooth grows into the cheek?
A so-called pocket of gum tissue forms above a tooth growing obliquely, into which food debris and bacteria enter, which leads to carious damage to the wisdom tooth. In this case, the inflammatory process can worsen, quickly develop into a putrefactive process and invade deeper areas. What should I do? You need to see a doctor as soon as possible, since the wisdom tooth is difficult to treat due to its location as the last one in the row.
The biggest concern is the eruption of the lower molars, since the gum tissue above them is the densest. However, dystopic upper molars also cause a lot of trouble. Having already erupted, they unpleasantly scratch the cheek and tongue, move adjacent teeth to the center, and change the bite.
Teething
The eruption of wisdom teeth begins at different ages, individually for each person, and lasts from three to five years (more details in the article: at what age do wisdom teeth usually grow?). According to norms, by the age of thirty, all four outer molars should erupt. This process is difficult because the jaw is already fully formed. The gum tissue above the surface of the tooth is dense and thick, sometimes it is not only connective tissue, but also periosteum. The tooth itself is wide, has several rounded tops (tops), which makes teething difficult.
When a tooth cannot break through the gum on its own and rests against its dense layer, it can continue to grow in the direction of least tissue resistance - sideways, towards other teeth. Due to constant compression and pressure, the gum tissue hurts. The pain impulse spreads along the lateral branches of the facial nerve to the neck, cheek, and ear. During teething, the tooth moves its “neighbors” towards the center, which also causes discomfort and spoils the appearance of the jaw. To speed up teething during a long process, you need to visit a dental surgeon, who, after anesthesia, will cut the gums.
Inflammation
With prolonged teething with pain, inflammation occurs, often aseptic, that is, without a bacterial component. It is accompanied by pain radiating along the nerve endings to the ear and temple; severe unilateral swelling and redness of the gums and cheeks. Ulcers and erosions form on the gums, and they may hurt. Swelling and inflammation can affect all nearby tissues. Chewing food, swallowing, and speaking are difficult. Sometimes it's even difficult to open your mouth. The local inflammatory process is manifested by systemic reactions: headache, weakness, low-grade fever.
READ ALSO: how and with what is an ulcer on the gum treated?
If oral bacteria enter the blood through an open wound in the gums during pericoronitis, the situation worsens. Pus begins to ooze out of the wound profusely, or a purulent abscess—flux—forms at the root of the tooth. The remains of dead microbes (pus) can permeate all layers of tissue layer by layer. Then phlegmon occurs, which requires urgent surgical intervention.
A serious complication of bacterial inflammation is the penetration of infection into deep tissues. In this case, bacteria are carried by the bloodstream to the area of the middle and inner ear, the consequence of which is purulent otitis media. The submandibular and parotid lymph nodes are affected, and a significant amount of pus accumulates in them. When an infection enters the systemic bloodstream, a general blood infection occurs - sepsis.
Pericoronitis
In such a case, even before complications arise, you should consult a surgeon. Necessary treatment is removal of excess tissue over the tooth, removal of the gingival hood, instrumental removal of food debris. It is impossible to clean the inside of the hood on your own due to the inconvenient position of the figure eight.
Caries
Caries is the destruction of enamel and dentin. Caries is one of the consequences of pericoronitis and causes toothache. Carious cavities are not visible under the gum hood of the wisdom tooth, where excellent conditions are created for the penetration of microbes into the enamel. After resection of the gingival hood and healing of the wounds, you need to contact a dentist for filling. Otherwise, the occurrence and progression of pulpitis is very likely, the treatment of which is difficult due to the position of the molar.
Toothache radiates to head
For many people, toothache causes headaches. Most often, the side of the head on which the problem tooth is located begins to hurt. Different teeth provoke pain in different areas of the head:
- molars cause pain in the parietal or occipital part of the head;
- the fangs give off throbbing pain in the temporal part;
- incisors provoke pain in the forehead;
- Lower teeth can often cause pain throughout the entire head at once.
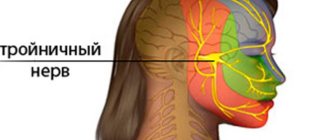
If a toothache radiates to the head, it is not always sharp and obvious. Some patients suffer from chronic headaches without even realizing that they are caused by a dental problem. This type of pain is called dental pain. The mechanism for the appearance of pain of a dental nature is irritation of the endings of the second and third branches of the trigeminal nerve and the autonomic facial nerve ganglia. The cause of migraine can be not only inflammatory processes of dental tissues, but also malocclusion. When the jaws close incorrectly, the temporomandibular joint receives additional stress and over time this leads to dull pain in the ear, temple, crown or back of the head.
A pinched triangular nerve caused by a malocclusion can cause severe headaches.
Many patients have noticed that after tooth extraction they often experience a headache. This phenomenon is quite normal, because tooth extraction is a rather traumatic surgical procedure. When removing a tooth, it is impossible not to damage the mucous membrane, gums and bone tissue, and this leads to headaches. The head may also hurt from the anesthesia that the dentist uses during the procedure. Usually the next day after surgery the headache stops hurting. What to do if a tooth gives you a headache? Taking painkillers may provide temporary relief. But at the first opportunity, you should consult a dentist to identify the cause of the disease and eliminate it.
Malocclusion and cervical osteochondrosis
When the lower jaw moves in any direction as a result of tooth loss or an incorrectly placed crown or filling, it results in muscle imbalance. Since the skull is attached to the first two vertebrae of the cervical spine, where the facial muscles originate, their imbalance can contribute to the curvature of the cervical vertebrae, and over time, the entire spine. The end result of such a disorder can be scoliosis and the resulting osteochondrosis in the cervical spine.
Why is this happening? The thing is that the structure of all organs of perception, such as vision and hearing, is symmetrical and the vestibular apparatus, in the event of any misalignment of the skull, reacts to this, compensating by tilting the head. And since you have to leave your head in a straight position, a bend occurs in the cervical spine, against which osteochondrosis develops. Signs of cervical osteochondrosis, which developed against the background of malocclusion of the jaw, in addition to the standard symptoms of pain and radicular syndrome, as well as pain when turning the head, there is a misalignment in the position of the shoulders, swelling of the joints of the hands, and the shoulder blade may hurt. Due to the close location of the mandibular joint to the auditory nerve, when opening the mouth, the neck may hurt and tinnitus may occur.
In this case, treatment is carried out in two directions - correction of the existing dental problem, as well as complex procedures aimed at maintaining the functions of the spine and restoring its mobility in the cervical region.
Treatment of malocclusion begins with diagnosis; for this, with the help of electrodes placed at the beginning of the jaw and a small current passing through them, complete relaxation of the facial muscles is achieved. Once the muscle tension that causes the imbalance is removed, the jaw will be in the correct position, which will make it possible to adjust the teeth for normal closure in the future. In this case, the dentist can build up teeth or cut down the protruding part, which caused the misalignment of the jaw.
Toothache radiates to temple
It happens that your tooth hurts and your temple hurts. As mentioned above, pain in the temple usually occurs when the fangs become inflamed. Another reason may be inflammation of the temporomandibular joint, in which the temple also begins to hurt. This inflammation can occur if a person has an incorrect bite or chews food on one side for a long time. Dentists recommend distributing the load on both sides when chewing food. But if there is at least one diseased chewing tooth, a person tries to eat so that food does not fall on him. As a result, the entire load falls on one side, forcing the temporomandibular joints to work twice as hard. To avoid this, it is necessary to promptly treat or remove diseased teeth.
Toothache radiates to jaw
Some patients ask the doctor: can a tooth cause jaw pain? Yes, this problem is familiar to any dentist. Its cause may be a serious dental disease such as osteomyelitis. Osteomyelitis of the jaw is a purulent-inflammatory process of the bone of the upper or lower jaw. It occurs as a result of infection of bone tissue by bacteria. The reason for this is advanced, untreated caries. With osteomyelitis, a person's jaw begins to hurt severely. This disease is fraught with serious complications and requires urgent treatment. Another cause of pain is the same wisdom teeth. When the lower wisdom teeth erupt, not only they, but the entire jaw often hurt. Jaw pain is often observed in people who wear braces and dentures. A brace system or denture puts pressure on the dentition and can cause quite unpleasant sensations in the jaw. At first, when wearing these structures, pain is the norm, because the jaws are not yet accustomed to them. When installing braces or dentures, dentists usually warn patients about this. But if wearing the prosthesis is very painful or the discomfort does not go away for a long time, you need to consult a doctor: perhaps the prosthesis is installed incorrectly or complications have arisen.
Bracket is a system on the lower jaw.
Toothache radiates to ear
It happens that toothache radiates to the ear. A common cause of this is pulpitis. When pressing on a sore tooth, the discomfort in the ear intensifies. From the ear, pain can spread to the entire temporal region. Pain in the ear is often observed after tooth extraction. They arise due to trauma to soft tissues during surgery and usually disappear within two days. If during this time the pain does not disappear, but only intensifies, this indicates the occurrence of complications. Inflammation of the trigeminal nerve also leads to ear pain. If the cause of such inflammation is not related to dental diseases, you should seek help from a neurologist. Inflammation of the upper jaw joint, malocclusion, and, of course, the growth of third molars also cause pain radiating to the ear. In this case, temporary help can be provided by rinsing with herbal decoctions or taking painkillers. But this cannot eliminate the cause of the pain, so a trip to the dentist is inevitable.
Toothache leads to a number of inconveniences: it is difficult to open your mouth, an unpleasant odor occurs due to the sprinkling of bacteria, pain in the ear...
Types of neck and jaw pain
The neck may hurt on the left side under the jaw, or the pain occurs on the right or in the front and radiates to the back. The nature of pain can be very different, due to one or another reason for its occurrence. The nature of the pain is very important for making a diagnosis, so it is necessary to describe it to the doctor as accurately as possible.
Intense pain on the sides of the neck under the jaw
Most often, such pain occurs due to inflammation of the lymph nodes and tonsillitis. Both diseases are the result of an infection entering the body. Migraines and dental infections can also cause severe pain under the jaw.
#!NevrologSeredina!#
It's a dull pain
If the pain is aching in nature, then it could be caused by a migraine, which, with bright light, changes in lighting or loud sounds, intensifies and concentrates in one place. Additionally, symptoms such as vomiting, nausea, vision problems and constant thirst may appear. Aching pain can also be associated with infectious dental diseases.
Pain under the jaw on the left
If your neck hurts on the left side under the jaw, then this may indicate almost any of the diseases that were listed above; Pain can also be associated with problems in the cardiovascular system. For example, pain on the left under the jaw appears with a heart attack or angina, which, as a rule, comes from pain in the chest area and is accompanied by acute pain in the teeth.
Pain when pressing
If your neck under your jaw begins to hurt when pressed or pressed, this may indicate inflammation of the lymph nodes, as well as diseases such as auricular ganglion neuralgia, osteogenic sarcoma, or the presence of sialoliths. Any painful sensations cannot be ignored. Even if discomfort in the neck and jaw does not cause any particular problems, this is not a reason to ignore it. Seeing a doctor in a timely manner is a decision that needs to be made immediately. Only a doctor can tell why your neck hurts under your jaw and what needs to be done about it.
Toothache radiates to the eye
The eye is another organ that can be affected by toothache. Its causes are the same factors as in other cases: caries, pulpitis, inflammatory processes such as periodontitis, periostitis, abscess, eruption of upper wisdom teeth. Inflammation in the oral cavity causes irritation of the nerve endings associated with the eyes, so toothache often radiates to the eye. And pain in the eye can cause headaches. To eliminate it, you can take a tablet of any painkiller. For this purpose, you can use ibuprofen, pentalgin, Nise and other analgesics that can be bought at the pharmacy. However, it should be remembered that medications provide only temporary relief, but do not cure the disease itself. Meanwhile, the tooth continues to decay. Therefore, you should not delay your visit to the dentist. Oral hygiene, balanced nutrition and regular preventive examinations at the dentist will prevent many dental problems and forever forget about such an unpleasant phenomenon as toothache.